Abstract
Imatinib is a novel tyrosine kinase inhibitor used for the treatment of Philadelphia chromosome–positive leukemias and other malignancies. Side effects are mostly moderate; however, a dose-dependent hematologic toxicity affecting all hematopoietic lineages is observed clinically. The aim of this study was to investigate the effect of imatinib on normal hematopoietic stem and progenitor cells in vitro. A dose-dependent decrease in proliferation potential was found when CD34+ cells were expanded in serum-free medium supplemented with 6 growth factors and imatinib. Functionally, a decrease in colony-forming capacity was observed under increasing doses of imatinib. However, no such effect on more primitive cobblestone area–forming cells was detectable. Both withdrawal of stem cell factor from our expansion cultures or functional inhibition of c-kit led to a similar degree of inhibition of expansion, whereas the effect of imatinib was substantially greater at all dose levels tested. These data suggest a significant inhibitory effect of imatinib on normal CD34+ progenitor (but not stem) cells that is largely independent of c-kit signaling.
Introduction
The selective tyrosine kinase inhibitor imatinib (formerly STI571) has been shown to block phosphorylation of tyrosine residues by occupying the adenosine triphosphate (ATP)–binding site of the Abl tyrosine kinases Bcr-Abl, c-Abl, v-Abl,1,2 and Abl-related gene (ARG)3 as well as platelet-derived growth factor receptor (PDGF-R) α and β and the receptor for human stem cell factor (SCF) c-kit.4-6 In a phase 3 study, imatinib has been shown to induce complete cytogenetic remissions in 74% of patients with chronic myeloid leukemia (CML) treated in early chronic phase (CP) after a median follow-up of 18 months.7 Furthermore, in clinical phase 2 studies, major cytogenetic remissions were observed in 24% of patients with CML in accelerated phase (AP)8 and 16% in myeloid blast crisis (BC).9 Based on these studies, imatinib is considered the new gold standard of treatment for CML.10 In gastrointestinal stromal tumors (GISTs), a tumor entity with constitutive activation of c-kit, imatinib induced sustained responses in more than 50% of the patients after a median follow-up of 9 months.11 Furthermore, patients with myeloproliferative diseases and rearrangements in the PDGF-Rβ gene on chromosome 5q33 have been shown to respond to treatment with imatinib.12
Typical nonhematologic side effects of imatinib are mostly moderate and only rarely lead to interruption of treatment. Hematologic side effects include all 3 lineages and are reversible on cessation of treatment.6 In patients with CP disease pretreated with interferon, the most common grade 3 or 4 toxicities were neutropenias, which occurred in 35% of the patients, followed by thrombocytopenia (in 20%) and anemia (in 7%).13 During first-line treatment, these incidences were 14%, 8%, and 3%, respectively.7 However, when imatinib was used at a higher dose, that is, 800 mg/d, incidence of grade 3 or higher toxicities increased substantially to 38%, 17%, and 5%, respectively, even when imatinib was administered in early CP.14
Due to the higher incidence of hematologic side effects seen in later stages of the disease, such as AP8 and BC,9 myelosuppression under imatinib treatment was at least in part attributed to the fact that after reduction of Philadelphia chromosome–positive (Ph+) hematopoiesis in response to treatment, normal hematopoietic stem and progenitor cells would need some time to recover from pre-existing suppression by the malignant clone and to re-expand in the bone marrow. Therefore, data from imatinib-treated patients with GISTs were of particular interest because these patients can be assumed to have an unimpaired bone marrow function. Interestingly, even in patients with GISTs treated with imatinib for a median follow-up of 9 months, 7% developed neutropenias (5% of which were grade 3 or 4) and 9% developed anemia (2% of which were grade 3 or 4).11
So far, the limited experience with imatinib does not allow estimates of long-term toxicity of the drug. Based on the known inhibitory effect of the drug on cAbl, c-kit, and PDGF-R, one could however speculate on potential hematotoxic side effects particularly after daily and long-term exposure to the drug. c-kit (or CD117) represents the receptor for human SCF, a cytokine that, together with Flt-3 ligand and thrombopoietin (TPO), is assumed to be critical for the expansion of immature human hematopoietic stem/progenitor cells (HSCs) at least in vitro.15-17 Moreover, just recently, PDGF has been demonstrated to be an effective cytokine for the ex vivo expansion of normal early stem and progenitor cells.18
The aim of this study was to investigate the effect of imatinib on the proliferative potential as well as on the functional properties of normal human CD34+ cells in vitro as well as to investigate potential signaling pathways affected by imatinib in Bcr-Abl– cells.
Materials and methods
Cell samples
Human umbilical cord blood (CB) was obtained from healthy full-term deliveries after informed consent was given. Fresh leukapheresis products from healthy donors and patients with nonhematopoietic disorders were collected after individuals gave their informed consent. Within 24 hours mononuclear cells (MNCs) were purified using Ficoll-Hypaque density gradient centrifugation (Biochrom, Berlin, Germany). The study was approved by the ethics review board of the medical faculty of the University of Tübingen.
Purification of stem and progenitor cells
Human CB cells were depleted of CD34+ cells using a negative StemSep column system (StemCell Technologies, Vancouver, BC, Canada) according to the supplier's directions. CD34+ cells from fresh leukapheresis samples were selected using a Midi-MACS CD34 isolation kit (Miltenyi Biotec, Bergisch Gladbach, Germany) according to the manufacturer's instructions. The purity of CD34+ cells ranged between 92% and 99% in all samples as determined by flow cytometry.
Reagents
Imatinib was generously provided by Novartis Pharma (Basel, Switzerland). For in vitro experiments, stock solutions of imatinib were prepared at 10 mg/mL and 100 μg/mL by dissolving the compound in dimethyl sulfoxide (DMSO)/H2O (1:1) and stored at –20°C. The final concentration of DMSO in the media was less than 0.1% or 0.37%, and it had no effect on the cell growth inhibition in the present study. The monoclonal antihuman c-kit antibody used in the present study is derived from the K44.2 hybridoma (Sigma-Aldrich, St Louis, MO). For in vitro experiments, stock solutions of the monoclonal antihuman c-kit antibody at 2.0 mg/mL in 0.01 M phosphate-buffered saline were stored at –20°C.
Short-term expansion of bulk CD34+ cells
For the time-course study, 1 × 103 mobilized CD34+ cells from healthy donors (n = 1) and from patients with nonhematopoietic disorders (n = 2) were seeded in triplicate (n = 2) or duplicate (n = 1, except of 0.625 μM where only a single value was obtained) in 96-well plates (Nunc, Roskilde, Denmark) containing 100 μL serum-free medium (SFM) supplemented with human SCF (100 ng/mL), human Flt-3 ligand (100 ng/mL), human TPO (50 ng/mL), human interleukin 3 (IL-3), human IL-6 (both 20 ng/mL, all from CellSystems, St Kartharinen, Germany) and granulocyte colony-stimulating factor (G-CSF; 20 ng/mL; Amgen, Munich, Germany).16 The same cytokine-supplemented SFM was used for all in vitro expansion experiments reported. Imatinib was added at increasing doses from 0 μM to 10 μM. The cells were incubated at 37°C in humidified atmosphere with 5% CO2 in air. After 5 days of culture, another 100 μL growth factor- and imatinib-containing medium was added. Estimation of the cell number within each individual well was performed for a total of 12 days in time intervals of 3 days under an inverted microscope.16
Flow cytometry, single-cell sorting, and expansion
Cells were analyzed on a FACSCalibur flow cytometer (Becton Dickinson, Heidelberg, Germany). The fluorescence of cells stained with fluorescein isothiocyanate (FITC) or phycoerythrin (PE) was excited with an argon laser at 488 nm and the emissions detected at 530 nm and 570 nm, respectively. Cell acquisition and analysis was performed using the CellQuest software program (Becton Dickinson).
Pre-enriched CD34+ cells from human umbilical CB (n = 2) were labeled with anti–CD34-FITC, anti–CD38-PE (Becton Dickinson), and 1 μg/mL propidium iodide (PI; Sigma-Aldrich). Using a FACSVantage cell sorter (Becton Dickinson), the subset of CD34+CD38–PI– cells was individually sorted directly into round-bottomed tissue culture plates (Nunc) containing either no imatinib or imatinib at a concentration of 5 μM in 100 μL SFM supplemented with the hematopoietic growth factors mentioned.
MTT assay
Cell proliferation and survival were measured by cellular uptake of 3,-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT; Sigma-Aldrich).19 Fresh CD34+ cells from 4 individual healthy donors were resuspended in growth factor-supplemented SFM at a concentration of 3 × 104 cells/150 μL. Cells were preincubated for 24 hours in 96-well flat-bottomed microtiter plates (Becton Dickinson) before imatinib was added at increasing concentrations (0-5 μM and 0-10 μM, respectively). All analyses were performed in triplicate. After 48 hours, 10 μL MTT solution (10 mg/mL) was added to each well. Plates were incubated for another 2 hours before 90 μL MTT lysis solution (15% sodium dodecyl sulfate [SDS] 50% dimethylformamide [DMF]) was added to each well and the absorbance was measured after 12 hours on an enzyme-linked immunosorbent assay (ELISA) plate reader (Dynatech MR7000; Dynatech, Denkendorf, Germany). The dose-effect relationship for imatinib at the point of IC50 was analyzed by the median-effect method20 using the Calcusyn Software (Biosoft, Cambridge, United Kingdom). The IC50 is defined as the concentration of drug that produces 50% cell growth inhibition and corresponds to the affected fraction (Fa value) of 0.5.
Apoptosis and cell cycle analysis
CD34+ cells (1 × 105 cells/well) from 3 healthy donors were cultured in 48-well tissue plates under the conditions described (see “Short-term expansion of bulk CD34+ cells”). After 24 hours of preincubation, imatinib was added at increasing doses from 0 μM to 10 μM and the cells were incubated either for another 24 hours or 48 hours before the fraction of apoptotic as well as phase G1 and G2 cells were measured by flow cytometry according to Nicoletti et al.21 Briefly, nuclei were prepared by lysing cells in a hypotonic lysis buffer (1% sodium citrate, 0.1% Triton X-100, 50 μg PI/mL) and subsequently analyzed by flow cytometry. Nuclei to the left of the 2N peak containing hypodiploid DNA were considered as apoptotic.
Methylcellulose progenitor assay for colony-forming units
The content of lineage-committed progenitors of CD34+ cells from healthy donors was assessed using a methylcellulose assay. Enriched CD34+ cells were plated in 1.1 mL semisolid methylcellulose progenitor culture medium (StemCell Technologies) containing a cocktail of recombinant human cytokines: SCF (50 ng/mL), granulocyte-macrophage colony-stimulating factor (GM-CSF; 10 ng/mL), IL-3 (10 ng/mL), and erythropoietin (Epo; 3 U/mL) and increasing concentrations of imatinib (0-10 μM). After 14 to 16 days of culture at 37°C in a humidified atmosphere with 5% CO2, plates were assessed for the presence of erythroid (mainly erythroid burst-forming units [BFU-Es]), myeloid (colony-forming units granulocyte, macrophage, and granulocyte-macrophage [CFU-Gs, CFU-Ms, CFU-GMs, respectively]) and mixed colonies (CFU-Mix).
Cobblestone area–forming cell assay of mobilized CD34+ cells
Confluent stromal layers of FBMD-1 cells in 96-well plates were overlaid with enriched CD34+ cells from 3 healthy donors in a limiting dilution setup.22 Input values ranged between 1 and 2000 CD34+ cells/well, each containing 200 μL medium (MyeloCult, CellSystems) supplemented with IL-3 (10 ng/mL) and G-CSF (20 ng/mL). Additionally, imatinib was added to the medium at different concentrations (0-10 μM) with 16 replicate wells per dilution. Once a week half the medium (100 μL) was replaced with fresh medium containing the previously described imatinib concentrations. The appearance of cobblestone areas, consisting of at least 5 cells, was evaluated after 5 weeks with a phase-contrast illumination on an inverted microscope. The frequency of cobblestone area–forming cells (CAFCs) was calculated with L-Calc software (StemCell Technologies) on the basis of the reciprocal of the concentration of test cells that yielded 37% negative cells.
Inhibition of c-kit signaling
To investigate whether the growth inhibitory effect of imatinib was solely due to inhibition of the c-kit signaling, 1 × 103 mobilized CD34+ cells from healthy donors (n = 3) were expanded in triplicate either under the same expansion conditions outlined or under the same conditions but in the absence of SCF. In both cases short-term expansion was performed with or without the addition of the c-kit inhibitory monoclonal antibody K44.2 (1 μg/mL; Sigma-Aldrich).
Transendothelial migration
Fresh CD34+ cells from 3 healthy donors were cultured in 24-well tissue plates under the conditions described containing either no imatinib or 1.25 μM imatinib. Cells were harvested after 24 and 48 hours of incubation. Migration across bone marrow endothelial cells was quantitatively analyzed as described previously23 using BMEC-1 cells grown to confluency on 3-μm microporous Transwell inserts (BD-Falcon, Heidelberg, Germany) placed in 24-well tissue culture plates. Recombinant human stromal-derived factor 1α (SDF-1; 500 ng/mL; R&D Systems, Wiesbaden, Germany) was added as a chemoattractant to the lower chamber and 1 × 105 CD34+ cells to the upper chamber of the transmigration system. Transmigrated cells were recovered and enumerated by flow cytometry after 14 hours.
Statistical analysis
Cellular expansion of CD34+ cells under increasing doses of imatinib in bulk cultures (Figures 1 and 7) as well as in colony-forming assays (Figure 4) was compared to control cells by using a post-hoc test after analysis of variance (ANOVA) including Bonferroni adjustment. The impact of imatinib on the apoptotic cell fraction (Figure 2), on CAFC frequency (Figure 5), and on transmigration (Figure 6) of CD34+ cells was analyzed by paired t test. The number of cells derived from single-cell expansion cultures with and without imatinib treatment was compared using the Wilcoxon test (Figure 3).
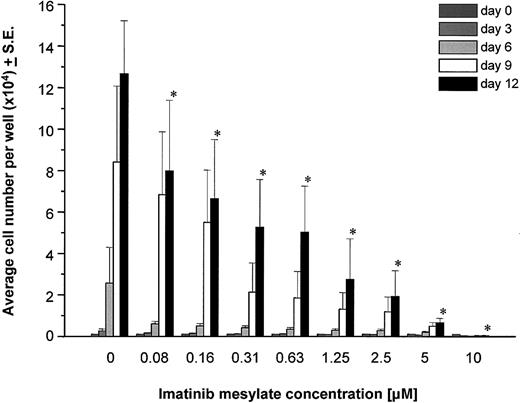
Cellular expansion of CD34+ cells with increasing doses of imatinib. Mobilized CD34+ cells from donors with nonhematopoietic disorders were expanded in serum-free medium (SFM) supplemented with growth factors starting with 1 × 103 cells/well under increasing doses of imatinib (0-10 μM). The average cell number per well was determined every third day for a total of 12 days in culture. The mean ± SE of replicate experiments (n = 3) is shown. The asterisk (*) indicates significantly reduced expansion in imatinib-treated as compared to control cells at day 12 (P < .001).
Cellular expansion of CD34+ cells with increasing doses of imatinib. Mobilized CD34+ cells from donors with nonhematopoietic disorders were expanded in serum-free medium (SFM) supplemented with growth factors starting with 1 × 103 cells/well under increasing doses of imatinib (0-10 μM). The average cell number per well was determined every third day for a total of 12 days in culture. The mean ± SE of replicate experiments (n = 3) is shown. The asterisk (*) indicates significantly reduced expansion in imatinib-treated as compared to control cells at day 12 (P < .001).
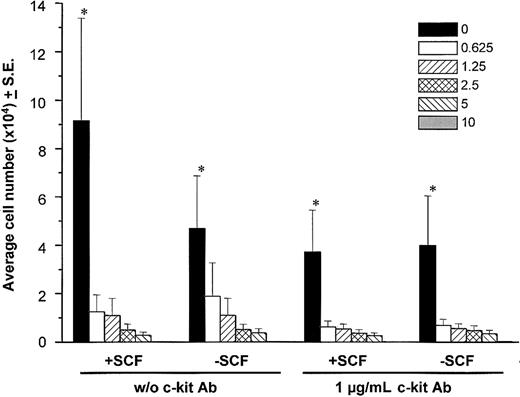
Comparison of imatinib treatment with functional inhibition of c-kit signaling. Mobilized CD34+ cells from healthy donors were expanded in SFM supplemented with human growth factor starting with 1 × 103 cells/well under increasing doses of imatinib (0-10 μM) either with or without SCF or with or without the addition of a monoclonal antibody that blocks SCF-dependent dimerization of c-kit. The mean ± SE of 3 individual donors after 12 days in culture is shown. The asterisk (*) denotes significant differences in imatinib-treated as compared to untreated control cells (▪) for each condition. Note that no significant difference was observed between untreated cells that either did not receive SCF or where c-kit signaling was functionally blocked by the addition of a monoclonal anti–c-kit antibody. Effect of treatment with imatinib was significantly more pronounced than the effect achieved by functional c-kit inhibition alone (P < .001).
Comparison of imatinib treatment with functional inhibition of c-kit signaling. Mobilized CD34+ cells from healthy donors were expanded in SFM supplemented with human growth factor starting with 1 × 103 cells/well under increasing doses of imatinib (0-10 μM) either with or without SCF or with or without the addition of a monoclonal antibody that blocks SCF-dependent dimerization of c-kit. The mean ± SE of 3 individual donors after 12 days in culture is shown. The asterisk (*) denotes significant differences in imatinib-treated as compared to untreated control cells (▪) for each condition. Note that no significant difference was observed between untreated cells that either did not receive SCF or where c-kit signaling was functionally blocked by the addition of a monoclonal anti–c-kit antibody. Effect of treatment with imatinib was significantly more pronounced than the effect achieved by functional c-kit inhibition alone (P < .001).
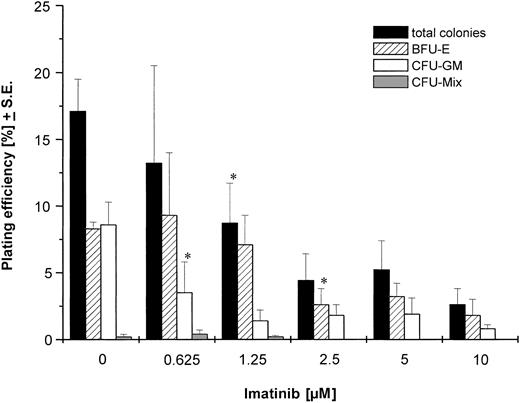
Methylcellulose assay illustrating the inhibitory effect of imatinib on normal lineage-committed progenitor cells in vitro. To evaluate imatinib-dependent CFU growth, 500 cells each were cultured in methylcellulose medium supplemented with different concentrations of imatinib ranging from 0 to 10 μM. The mean ± SE of the plating efficiency (in percent) of CFUs was determined 14 to 16 days after incubation (n = 3 individual donors; except for 0.625 μM, where results from only 2 donors were available). The asterisk (*) indicates lowest imatinib concentration at which significant differences compared to untreated cells were observed for total colonies (P < .002), BFU-Es (P < .002), and CFU-GMs (P < .001).
Methylcellulose assay illustrating the inhibitory effect of imatinib on normal lineage-committed progenitor cells in vitro. To evaluate imatinib-dependent CFU growth, 500 cells each were cultured in methylcellulose medium supplemented with different concentrations of imatinib ranging from 0 to 10 μM. The mean ± SE of the plating efficiency (in percent) of CFUs was determined 14 to 16 days after incubation (n = 3 individual donors; except for 0.625 μM, where results from only 2 donors were available). The asterisk (*) indicates lowest imatinib concentration at which significant differences compared to untreated cells were observed for total colonies (P < .002), BFU-Es (P < .002), and CFU-GMs (P < .001).
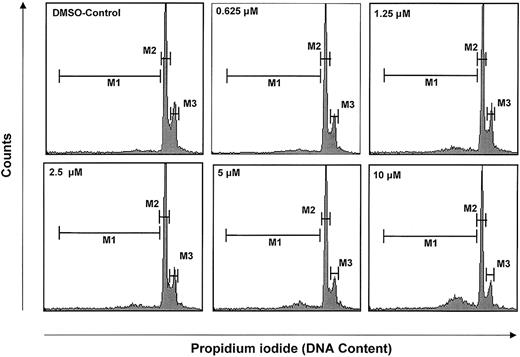
Apoptosis and cell cycle analysis. Apoptosis and cell cycle analysis after 48 hours of exposure to imatinib was performed according to Nicoletti et al.21 Note that no significant increase in the fraction of apoptotic cells was observed up to doses of 10 μM imatinib.
Apoptosis and cell cycle analysis. Apoptosis and cell cycle analysis after 48 hours of exposure to imatinib was performed according to Nicoletti et al.21 Note that no significant increase in the fraction of apoptotic cells was observed up to doses of 10 μM imatinib.
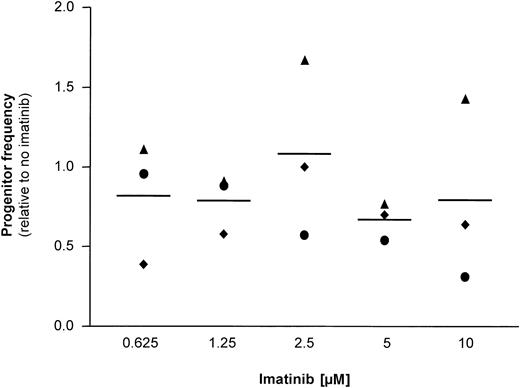
Frequency of CAFCs. CAFC frequency of CD34+ cells from healthy donors (n = 3) that were exposed to imatinib at the concentrations ranging from 0 to 10 μM for 5 weeks. The frequency of CAFCs was calculated with L-Calc software (StemCell Technologies). The relative progenitor frequency as compared to untreated cells for every single donor as well as the mean (horizontal bar) is shown.
Frequency of CAFCs. CAFC frequency of CD34+ cells from healthy donors (n = 3) that were exposed to imatinib at the concentrations ranging from 0 to 10 μM for 5 weeks. The frequency of CAFCs was calculated with L-Calc software (StemCell Technologies). The relative progenitor frequency as compared to untreated cells for every single donor as well as the mean (horizontal bar) is shown.
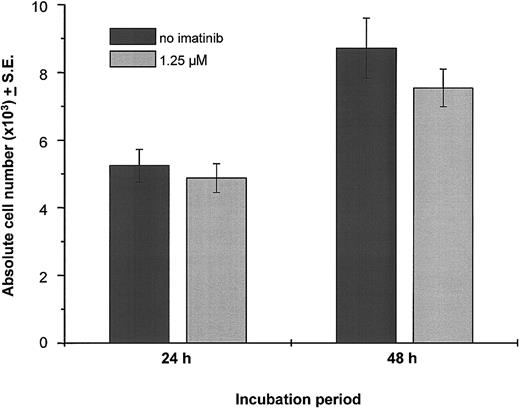
Transendothelial migration across bone marrow endothelium after 24 and 48 hours of incubation with imatinib. The mean absolute cell number (± SE) of migrated hematopoietic progenitor cells treated with imatinib (1.25 μM) for 24 or 48 hours is shown.
Transendothelial migration across bone marrow endothelium after 24 and 48 hours of incubation with imatinib. The mean absolute cell number (± SE) of migrated hematopoietic progenitor cells treated with imatinib (1.25 μM) for 24 or 48 hours is shown.
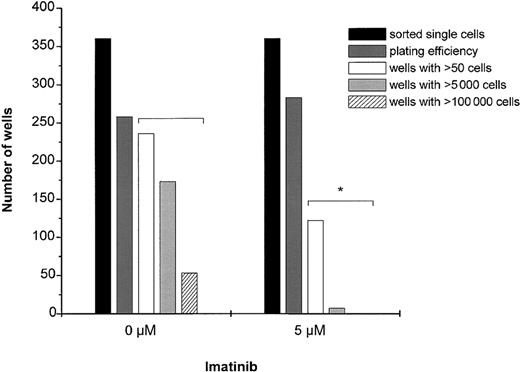
Number of clones derived from single-cell expansion cultures. Distribution of clones derived from single-cell expansion cultures of CD34+38– cells from human umbilical CB (n = 2) in SFM supplemented with 6 growth factors and either with or without imatinib (concentration, 5 μM). Note that whereas 15% of the single CD34+38– cells were expandable to more than 105 cells in vitro, none of the imatinib-treated clones reached that margin. The asterisk (*) indicates significant difference between imatinib-treated and control cells at day 18 (P < .001).
Number of clones derived from single-cell expansion cultures. Distribution of clones derived from single-cell expansion cultures of CD34+38– cells from human umbilical CB (n = 2) in SFM supplemented with 6 growth factors and either with or without imatinib (concentration, 5 μM). Note that whereas 15% of the single CD34+38– cells were expandable to more than 105 cells in vitro, none of the imatinib-treated clones reached that margin. The asterisk (*) indicates significant difference between imatinib-treated and control cells at day 18 (P < .001).
Results
Short-term expansion of bulk CD34+ cells
Mobilized CD34+ cells were expanded for 12 days in SFM supplemented with human growth factors starting with 1 × 103 cells/well under increasing doses of imatinib (0-10 μM). A concentration of 10 μM imatinib caused a reduction of the start fraction to 318 ± 266 (mean ± SE) viable CD34+ cells at day 12 (Figure 1). For doses up to 5 μM imatinib, a continuous expansion of hematopoietic cells was observed for 12 days in culture. However, even at the lowest concentration studied (ie, 0.08 μM imatinib), a significant reduction of the clone size compared to the untreated cells became evident (P = .01). The degree of expansion decreased in a dose-dependent fashion in treated compared to untreated cells (P < .001).
MTT assay
A tetrazolium-based MTT assay was used to quantity 50% growth inhibition (IC50) of cytokine-stimulated CD34+ cells from healthy donors after 48 hours of exposure to imatinib. The mean IC50 (± SD) for imatinib on normal CD34+ progenitor cells was 0.9 ± 0.6 μM (raw data: 0.8 μM; 0.6 μM; 0.3 μM; 1.8 μM, not shown).
Apoptosis
Apoptosis as well as cell cycle analysis was performed according to Nicoletti et al.21 No significant effect on the fraction of apoptotic cells was observed up to concentrations of 10 μM after 24 hours and 48 hours of exposure to imatinib, respectively (Table 1; Figure 2).
Apoptosis and cell cycle analysis in normal CD34+ hematopoietic progenitor cells after 24 or 48 hours of exposure to imatinib
. | 24 h . | . | . | 48 h . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Imatinib, μM . | Apoptosis, % . | G1, % . | S/G2/M, % . | Apoptosis, % . | G1, % . | S/G2/M, % . | ||||
| 0 | 7.8 ± 3.4 | 70.2 ± 3.0 | 20.4 ± 3.7 | 5.0 ± 1.1 | 70.7 ± 5.4 | 20.4 ± 4.4 | ||||
| 0.3125 | 10.1 ± 4.0 | 69.5 ± 2.5 | 16.6 ± 2.0) | 8.6 ± 1.8 | 71.2 ± 6.5 | 18.5 ± 2.5 | ||||
| 0.625 | 9.8 ± 4.9 | 73.7 ± 3.8 | 14.8 ± 1.0 | 10.5 ± 3.4 | 69.7 ± 7.9 | 17.5 ± 2.8 | ||||
| 1.25 | 9.6 ± 4.9 | 73.0 ± 4.9 | 15.2 ± 1.8 | 10.7 ± 4.1 | 70.7 ± 7.6 | 15.6 ± 4.2 | ||||
| 2.5 | 9.4 ± 4.4 | 73.3 ± 6.0 | 14.6 ± 2.2 | 10.5 ± 2.7 | 70.3 ± 6.0 | 16.4 ± 3.3 | ||||
| 5 | 10.9 ± 5.5 | 73.3 ± 6.0 | 13.8 ± 2.3 | 13.1 ± 3.8 | 69.2 ± 8.0 | 14.4 ± 4.1 | ||||
| 10 | 12.0 ± 7.2 | 71.7 ± 9.3 | 13.1 ± 2.3 | 21.5 ± 11.3 | 62.8 ± 10.8 | 12.3 ± 4.3 | ||||
. | 24 h . | . | . | 48 h . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Imatinib, μM . | Apoptosis, % . | G1, % . | S/G2/M, % . | Apoptosis, % . | G1, % . | S/G2/M, % . | ||||
| 0 | 7.8 ± 3.4 | 70.2 ± 3.0 | 20.4 ± 3.7 | 5.0 ± 1.1 | 70.7 ± 5.4 | 20.4 ± 4.4 | ||||
| 0.3125 | 10.1 ± 4.0 | 69.5 ± 2.5 | 16.6 ± 2.0) | 8.6 ± 1.8 | 71.2 ± 6.5 | 18.5 ± 2.5 | ||||
| 0.625 | 9.8 ± 4.9 | 73.7 ± 3.8 | 14.8 ± 1.0 | 10.5 ± 3.4 | 69.7 ± 7.9 | 17.5 ± 2.8 | ||||
| 1.25 | 9.6 ± 4.9 | 73.0 ± 4.9 | 15.2 ± 1.8 | 10.7 ± 4.1 | 70.7 ± 7.6 | 15.6 ± 4.2 | ||||
| 2.5 | 9.4 ± 4.4 | 73.3 ± 6.0 | 14.6 ± 2.2 | 10.5 ± 2.7 | 70.3 ± 6.0 | 16.4 ± 3.3 | ||||
| 5 | 10.9 ± 5.5 | 73.3 ± 6.0 | 13.8 ± 2.3 | 13.1 ± 3.8 | 69.2 ± 8.0 | 14.4 ± 4.1 | ||||
| 10 | 12.0 ± 7.2 | 71.7 ± 9.3 | 13.1 ± 2.3 | 21.5 ± 11.3 | 62.8 ± 10.8 | 12.3 ± 4.3 | ||||
DNA content was determined according to Nicoletti et al21 and analyzed by flow cytometry. The percentage of apoptotic cells was defined as the percentage of CD34+ cells containing decreased levels of DNA (hypodiploid peak). Data are expressed as mean ± SD of 3 independent experiments.
Expansion of single-sorted CD34+38– cells from human umbilical CB
To extend the studies to the more primitive CD38– subset of CD34+ cells, individual CD34+38– stem cell candidates (n = 720) from human umbilical CB (n = 2) were directly sorted into 96-well plates and expanded under the described conditions containing either no imatinib or imatinib at a concentration of 5 μM. The expansion and the growth kinetics of the single-sorted CD34+38– stem cell candidates were analyzed in time intervals of 3 days up to day 18 (Figure 3). Cloning efficiency (defined as individual clones with > 50 cells/well) in untreated compared to treated cells was 66% compared to 34%. Whereas 15% of the untreated clones expanded to more than 1 × 105 cells, none of the treated cells reached that size threshold. A significant (P < .001) difference in the average cell number per well at day 18 of expansion culture in treated cells (mean ± SE, 160 ± 38) compared to untreated cells (mean ± SE, 17 704 ± 1584) was observed (Wilcoxon test).
Inhibitory effect of imatinib on colony-forming capacity of CD34+ cells
To investigate the impact of imatinib on hematopoietic progenitor cell growth in vitro, a clonal colony assay was used. CFU formation from CD34+ cells was inhibited by imatinib treatment in a dose-dependent fashion (Figure 4). A reduction of colony-forming capacity due to treatment with imatinib for 14 to 16 days was detectable at a concentration of 1.25 μM (total colonies, P = .001) and affected both BFU-Es (significant from 2.5 μM, P < .002) and CFU-GMs (significant from 0.625 μM, P < .001). Furthermore, imatinib treatment led to a reduction in colony size as compared to controls.
CAFC assay of mobilized CD34+ cells
The effect of imatinib on more primitive progenitor growth was evaluated by in vitro exposure of CD34+ cells to imatinib under the described growth factor conditions followed by enumeration of primitive CAFCs. CD34+ cells were exposed to imatinib for 5 weeks. The number of CAFCs per individual CD34+ cell was variable between individuals (Figure 5). However, as opposed to CFUs, normal CAFC capacity was not significantly suppressed by exposure to imatinib at concentrations ranging from 0.625 to 10 μM. Furthermore, no difference in size and morphology of treated CAFCs as compared to untreated CAFCs was observed.
Transendothelial migration of imatinib-treated CD34+ hematopoietic cells
To study the effects of imatinib on transendothelial migration of normal CD34+ cells, CD34+ progenitor cells from healthy donors were incubated with 1.25 μM imatinib, that is, at a clinically relevant dose level, where inhibition of proliferation but no significant induction of apoptosis had been observed in the previous experiments. In vitro migration across bone marrow endothelial cells was quantitatively analyzed by flow cytometry after 24 hours and 48 hours of incubation. Figure 6 shows the absolute number of migrated hematopoietic CD34+ progenitor cells indicating no significant effect of imatinib on the number of transmigrated progenitor cells as compared to controls.
Inhibition of c-kit signaling
Another aim of the current study was to investigate whether the growth inhibitory effect of imatinib on CD34+ cells from healthy donors was solely due to inhibition of c-kit. Both withdrawal of SCF or inhibition of c-kit led to a similar degree of inhibition of expansion, whereas the growth inhibitory effect of imatinib was substantially greater than this for all conditions even at the lowest dose level tested (P < .001) suggesting that other pathways apart from c-kit are involved in the inhibitory effect (Figure 7).
Discussion
Hematologic side effects of imatinib are dose-dependent, are reversible, and include all 3 hematopoietic lineages to a variable degree.7,9,11,13,14 To investigate the effect of imatinib on normal human CD34+ stem/progenitor cells in vitro, we used a bulk culture system including SFM supplemented with cytokines that had been shown to be effective for ex vivo expansion of immature hematopoietic cells.16,17 The degree of expansion decreased in a significant and dose-dependent fashion in treated compared to untreated cells. To extend these studies to the more primitive CD38– subset of CD34+ cells, individual CD34+38– cells were single-sorted and expanded under the same conditions either with or without imatinib. Both average expansion as well as maximum expansion potential of the clones derived from individual CD34+38– cells was significantly reduced in the presence of imatinib. The mechanism by which imatinib exerts its antiproliferative effect on normal CD34+ cells has yet to be elucidated. Induction of apoptosis has been described in Bcr-Abl+ cells.24 However, in vitro exposure to imatinib up to a concentration of 10 μM for 48 hours neither led to a significant induction of apoptosis nor to a significant G1 arrest in normal cytokine-stimulated CD34+ cells, similar to results reported by others using annexin V staining.25,26 Thus, the apoptosis-inducing effects of imatinib seem unlikely to be responsible for its growth inhibitory effect on normal hematopoiesis at least at the concentrations usually achieved in patients (ie, 1-2 μM).
The observation of an antiproliferative effect of imatinib on Bcr-Abl– hematopoietic cells is supported clinically by the observations that the incidence of grade 3 or higher myelosuppression in imatinib-treated early CP patients is highly dose dependent14 and that hematologic side effects also occur (although at a lower incidence) in disease entities such as GISTs,11 which are not assumed to compromise the hematopoietic system. Furthermore, recent reports derived from patients with Ph– myeloproliferative disorders that have been successfully treated with imatinib,27,28 even in the absence of chromosomal translocations involving chromosome 5q33, suggest an effect of imatinib on Bcr-Abl– hematopoietic progenitor cells.29
To date, the functional level at which imatinib exerts its antiproliferative effect on normal hematopoietic cells has not been fully clarified. Data from a recent study showing no effect of imatinib on the reconstitution of murine cells after allogeneic transplantation in a syngeneic mouse transplantation model argue against a stem cell toxic effect of the drug.30 This finding is also in agreement with the lack of an effect observed in the experimental human-mouse31 transplantation model and with first clinical observations confirming that administration of imatinib after allogeneic stem cell transplantation is safe and does not increase hematologic toxicities.32 Further support for the assumption that imatinib acts primarily on the more actively cycling (as opposed to the quiescent) components of the stem/progenitor cell compartment comes from the observation that even Ph+ nondividing CD34+ cells are accumulating under treatment in vitro.33 In addition, recent data demonstrating that in patients with CML, achieving a complete cytogenetic remission with imatinib treatment, Bcr-Abl transcripts are enriched in the CD34+ (as compared to the total MNC) fraction and remain detectable in the long-term culture-initiating cell (LTC-IC) compartment,34 provide further support for this hypothesis.
To determine the functional level at which the inhibition of normal CD34+ cells occurred, we studied the impact of imatinib on colony formation as well as on the CAFC capacity of normal CD34+ cells. Although we confirmed a dose-dependent decrease in CFU formation with imatinib treatment,25,30,35,36 no significant effect on the CAFC capacity of normal CD34+ cells was observed, similar to findings by others.25 Altogether, these results argue for a selective inhibitory effect of imatinib on the progenitor cell level, whereas the immature stem cell compartment seems to be spared. Alternatively, the presence of stromal cells could have a protective effect on the proliferation of normal CD34+ cells.
The feasibility of mobilization of normal CD34+ cells for the purpose of autologous transplantation has recently been demonstrated in pilot studies in patients with CML.37-39 In line with this observation, we found no effect on the migration of normal CD34+ cells in a transendothelial migration assay arguing against a negative effect of imatinib on the mobilization of normal CD34+ cells.
Unexpectedly, based on the relatively mild hematologic side effects of imatinib observed clinically, the IC50 of imatinib on normal CD34+ cells under cytokine stimulation measured by MTT assay was not substantially different from what we had observed in Bcr-Abl+ cell lines such as K562 grown in culture without cytokine stimulus. We therefore hypothesized that the extensive cytokine stimulation by the growth factor cocktail used in this study was one of the reasons for the increased susceptibility of the normal cells to imatinib. However, from a clinical standpoint, it remains questionable whether these in vitro cytokine conditions reflect steady-state hematopoiesis in vivo or the state of regeneration of Ph– polyclonal hematopoiesis once its suppression by the Ph+ clone is relieved due to the initiation of imatinib treatment. On the other hand, more than one third of patients with newly diagnosed CML being treated with 800 mg imatinib have experienced grade 3 or higher neutropenia.14
To investigate whether the growth inhibitory effect of imatinib on normal CD34+ cells was solely due to inhibition of the SCF/c-kit pathway, we expanded mobilized CD34+ cells from healthy donors under the same growth conditions outlined but either in the absence of SCF or by adding a monoclonal antibody that had been shown to block SCF-dependent dimerization of c-kit.40 Although both withdrawal of SCF and blocking of c-kit by a monoclonal antibody led to a similar degree of inhibition of expansion, the inhibitory effect of imatinib was substantially more pronounced, arguing for an inhibition of normal CD34+ cells via additional factors other than c-kit signaling. One potential candidate target receptor for a growth inhibitory effect by imatinib might be PDGF-R. First, although not expressed on fresh CD34+ cells, an up-regulation of the receptor was noted after culture for 3 days.18 Second, PDGF-R could potentially exert its effect on the expansion of HSCs by secondary mechanisms, for example, mediated via macrophages or other cells that express PDGF-R.41
Furthermore, inhibition of c-Abl could contribute to the growth inhibitory effect observed with imatinib. Using antisense strategies, it has been demonstrated that inhibition of c-Abl leads to accumulation of CD34+ cells in G0/G1 and to inhibition of CFU-GM formation, whereas BFU-Es remained unaffected.42 Interestingly, no evidence of the induction of apoptosis was observed, which is in agreement with the results reported here. Alternatively, other as of yet unknown targets of imatinib could be responsible for this effect.
In summary, these data suggest a significant inhibitory effect of imatinib on normal CD34+ progenitor (and not stem) cells that is largely independent of c-kit signaling and seems to be linked to cell cycle activity of the cells. The results of this study might (at least partly) explain the dose dependency of the hematologic side effects of imatinib and could provide a rationale for further in vitro studies evaluating the use of the drug in Ph– myeloproliferative syndromes.
Prepublished online as Blood First Edition Paper, September 11, 2003; DOI 10.1182/blood-2003-05-1535.
Supported by the Sonderforschungsbereich 510 (Teilprojekt A6) of the Deutsche Forschungsgemeinschaft, as well as a grant from the Deutsche Krebshilfe (no. Br 70-2746).
K.B. and S.B. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We would like to thank Alexandra Wahl, Iris Schäfer, and Bettina Kirchner for excellent technical assistance and Dr Martin Eichner (Department of Medical Biometry, Tübingen) for help with statistical analysis of the data. Furthermore, we want to thank Tessa L. Holyoake (Glasgow, United Kingdom) for critical reading of the manuscript.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal