Inflammatory reactions are often associated with hemolysis and consequently with the accumulation of free heme released from oxidized hemoglobin. This results in internalization of the free heme by vascular endothelial cells (ECs), where the iron in the core of the heme structure acts as a potent pro-oxidant to promote EC cytotoxicity.1 The only manner in which ECs can decrease the intracellular levels of free heme is to up-regulate the expression heme oxygenase-1 (HO-1), a stress-responsive enzyme that catalyzes the initial and rate-limiting steps in the oxidative degradation of heme into biliverdin, iron, and carbon monoxide (CO).
We and others have previously shown that the expression of HO-1 prevents the deleterious effects associated with vascular injury, such as the development of arteriosclerotic lesions that arise following EC injury/denudation.2,3 This protective effect is mimicked by exogenous CO, thus suggesting that it is mediated via the ability of HO-1 to convert heme into CO.3 An interesting feature in the protective effect of CO is that a single “pulse” of exogenous CO (one hour) seems to be sufficient to block the development of arteriosclerotic lesions, such as those that arise following balloon injury of the carotid artery in rats.3 This suggests that CO triggers a protective response in cells of the vascular wall that continues to act despite the fact that exposure of these cells to CO has been discontinued. The molecular mechanism underlying this potent and long-lasting protective effect remains to be established.
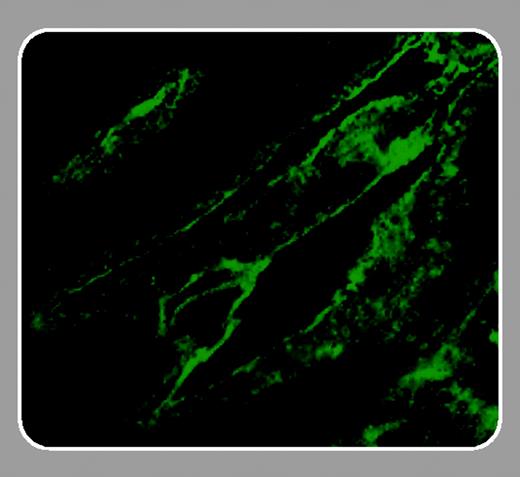
The article by Bussolati and colleagues that appears in this issue of Blood (page 761) may help to further explain the mechanism underlying the protective effect of HO-1 and CO. The authors demonstrate that vascular endothelial growth factor (VEGF) induces the expression of HO-1 in ECs and, perhaps more important, that HO-1 enzymatic activity in these cells can be critical for the angiogenic effect of VEGF. This adds significantly to the previous observation that HO-1 promotes angiogenesis,4 in that it directly links the potent angiogenic effect of VEGF to the expression and enzymatic activity of HO-1. In addition, the data obtained by the authors may provide important answers related to the mechanism of action of VEGF in terms of modulating arteriosclerotic lesions triggered by EC injury/denudation. Based on these findings, it is likely that the salutary effects of VEGF are largely due to the expression of HO-1. Induction of HO-1 would not only enhance re-endothelialization of the injured vessels, but it would also protect the newly formed ECs from undergoing apoptosis, suppress the proinflammatory phenotype associated with monocyte/macrophage (Mϕ) activation, and inhibit smooth muscle cell proliferation, all of which are key features in the development of arteriosclerotic lesions (reviewed in Soares et al5 ).
It is interesting to note that expression of VEGF and HO-1 in ECs may trigger a “positive feedback loop” in which VEGF up-regulates HO-1 and HO-1 up-regulates VEGF.6 A similar phenomenon has been shown to mediate the anti-inflammatory effect of interleukin-10 (IL-10) in Mϕ, in which IL-10 up-regulates HO-17 and HO-1 up-regulates IL-10.8 These types of positive feedback loops may explain why a single pulse of exogenous CO, given before vascular injury, is sufficient without further treatment to block the development of arteriosclerotic lesions.3 This may also explain the potent and long-lasting protective effects of HO-1 and/or CO in a variety of other inflammatory situations.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal