β-thalassemias are the most common single gene disorders and are potentially amenable to gene therapy. However, retroviral vectors carrying the human β-globin cassette have been notoriously unstable. Recently, considerable progress has been made using lentiviral vectors, which stably transmit the β-globin expression cassette. Thus far, mouse studies have shown correction of the β-thalassemia intermedia phenotype and a partial, variable correction of β-thalassemia major phenotype. We tested a lentiviral vector carrying the human β-globin expression cassette flanked by a chromatin insulator in transfusion-dependent human thalassemia major, where it would be ultimately relevant. We demonstrated that the vector expressed normal amounts of human β-globin in erythroid cells produced in in vitro cultures for unilineage erythroid differentiation. There was restoration of effective erythropoiesis and reversal of the abnormally elevated apoptosis that characterizes β-thalassemia. The gene-corrected human β-thalassemia progenitor cells were transplanted into immune-deficient mice, where they underwent normal erythroid differentiation, expressed normal levels of human β-globin, and displayed normal effective erythropoiesis 3 to 4 months after xenotransplantation. Variability of β-globin expression in erythroid colonies derived in vitro or from xenograft bone marrow was similar to that seen in normal controls. Our results show genetic modification of primitive progenitor cells with correction of the human thalassemia major phenotype.
Introduction
β-thalassemias are the most common single gene defects, caused by mutations in the β-globin gene/regulatory elements, resulting in reduced or absent adult hemoglobin (HbA; α2β2). Thalassemia heterozygotes are mildly anemic and lead normal lives. Homozygosity results in disease: thalassemia intermedia, where individuals are moderately anemic due to reduced β-globin production; and thalassemia major or Cooley anemia, characterized by absent or severely reduced β-globin production. The latter individuals get profoundly anemic within 6 to 9 months after birth when the fetal hemoglobin (HbF) to HbA switch is complete, and become transfusion dependent for life.1 Chronic transfusions are associated with iron overload, the major cause of death.2 Bone marrow transplant, a curative modality, is limited by the availability of matched donors and is associated with potential complications, including graft-versus-host disease.3-5
Gene therapy using autologous bone marrow can potentially permanently cure β-thalassemia major. However, retroviral vectors carrying the β-globin gene and its regulatory elements have notoriously suffered from problems of vector instability, low titers, and variable expression.6-11 In a pioneering study, May et al12 were able to stably transmit the human β-globin gene and its regulatory elements in lentiviral vectors and correct β-thalassemia in Hbbth3/+ mice with an average increase of hemoglobin by 3 to 4 g/dL. Subsequently, others have shown 1.1 to 2.3 g/dL increase in hemoglobin per vector copy in mouse models using similar lentiviral vectors.13-17 The Hbbth3/+ mice carry deletion of the βmajor and βminor genes on one allele and resemble the human thalassemia intermedia phenotype.18,19 Homozygous deletion of both the βminor and βmajor globins is embryonic lethal, because unlike humans, the switch to adult globin production occurs in utero in mice.
Rivella et al17 developed an elegant mouse model of β-thalassemia major by transplanting fetal liver cells from thalassemia major fetuses, prior to embryonic fatality, into lethally irradiated normal adult mice. They showed that fully engrafted mice die of severe anemia (hemoglobin levels 2 to 3 g/dL) within 6 to 8 weeks of transplantation, while genetic correction of the β-thalassemia major fetal liver cells with the same vector, previously shown to correct thalassemia intermedia mice, 12 rescued the lethality. However, gene transfer resulted in conversion of the β-thalassemia major phenotype to that of severe thalassemia intermedia in all but one mouse.17 Thus far, all of these reports of gene therapy in thalassemia mice14,15,17 using human β- or γ-globin–based lentiviral vectors suggest that vectors with higher expression may be necessary for correction of human thalassemia major.
Another notable feature in murine studies is the highly variable β- or γ-globin expression among different mice, 16,20,21 despite the presence of β- or α-globin regulatory elements, which are known to confer position independent expression. The chicken hypersensitive site 4 (cHS4) chromatin insulator element in oncoretroviral vectors has been reported to reduce position effect variegation (PEV) and, therefore, improve expression.22 Additionally, cHS4 elements have enhancer-blocking activity23 and, therefore, may have a better vector biosafety profile. This is especially important in light of recent reports of insertional oncogenesis induced by retroviral vectors24 and subsequent analysis showing the high propensity of these vectors to integrate into intragenic sites.25,26 We have analyzed expression of an enhanced green fluorescent protein (GFP) reporter from an erythroid-specific vector in vivo in secondary mice with analogous self-inactivating (SIN) lentiviral vectors with or without the cHS4 insulator and observe increased expression and reduced PEV with insertion of the cHS4 element.27
We therefore constructed an SIN lentiviral vector carrying the human β-globin gene and regulatory elements and the cHS4 insulator and tested its ability to reverse the phenotype of human thalassemia major. We have previously reported a human model of normal28 and thalassemia erythropoiesis29 that results in generation of enucleated red blood cells (RBCs) from normal hematopoietic progenitor cells and recapitulates the ineffective erythropoiesis observed in patients with thalassemia major. In this study, we report complete correction of human thalassemia major phenotype after gene transfer into β-thalassemia major CD34+ cells in the in vitro model and confirm these results in vivo in the β2mnull NOD-SCID human xenograft mice.
Materials and methods
Lentiviral vectors
A 3.1-kilobase (kb) human β-globin locus control region (LCR) fragment and the 2.3-kb human β-globin gene were cloned in reverse orientation to the vector transcriptional unit into a SIN HIV vector (derived from the HXB2 and NL4-3 strains) to generate the β-globin vector, termed BG. The LCR fragment, amplified by polymerase chain reaction (PCR), consisted of a 0.7-kb fragment of HS2, a 1-kb fragment of HS3, and a 1.4-kb fragment of HS4 (Gene Bank accession number U01317). The β-globin gene was amplified from genomic DNA in 2 parts: one amplicon contained the β-globin promoter, exon1, intron1, exon2, and part of intron2, and the other amplicon contained the β-globin intron2, exon3, and the 3′ flanking DNA containing a putative 3′ enhancer.30 Ligation of the 2 amplicons deleted the 272 bp of intron2, previously shown to interfere with vector production.10 The 1.2-kb XbaI cHS4 insulator fragment from pJC13-1 (kindly provided by Dr G. Felsenfeld, Bethesda, MD) was cloned into the EcoRV and PvuII sites in the U3 region (3′ long terminal repeat [LTR]) to replace the enhancer and promoter sequences. The insulator-containing LTR replaced the 3′LTR in BG to generate the insulated vector termed BGI. The details of PCR, cloning, and coordinates of the LCR and 3′ enhancer sequences are available upon request.
Virus production
Virus was produced by transient cotransfection of 293T cells using the vector, packaging, and envelop plasmids (VSV-G)20 and virus-containing supernatant collected at 60 hours after transfection and concentrated by low-speed filtration using 0.2-μM polyethersulfone filter (Millipore, Bedford, MA) followed by ultracentrifugation (26 000 rpm × 90 minutes). The virus was concentrated 10 000-fold from viral supernatants. Viral titers were determined by infecting mouse erythroleukemia (MEL) cells, using serial dilution of concentrated virus, differentiating them, and analyzing them for HbA expression by fluorescence-activated cell-sorter scanner (FACS) and a semiquantitative PCR.20 PCR was performed using primers to human β-globin: forward primer 5′-AAGTCGACGTGCTAGTCTCCCG-GAAC-3′ and reverse primer 5′-AACTCGAGCAGAAGCACCATA-AGGGA-3′ amplified for 2 cycles at 92°C × 30,” 60°C × 30,” 72°C × 30”; 18 cycles at 94°C × 30,” 60°C × 30,” 72°C × 30”, and 1 cycle at 72°C × 5 minutes.
Human CD34 isolation and transduction: sample collection and processing
All bone marrow samples were obtained from voluntary donors using protocols approved by the local institutional review board at Childrens Hospital Los Angeles (CHLA) after obtaining informed consent. Normal bone marrow (NBM) was obtained from cadaveric donors and healthy volunteers. Thalassemia bone marrow was obtained when patients were under general anesthesia for another clinically indicated surgery. β-thalassemia major patients were 0.5, 1.5, 6, and 22 years of age (n = 4). Diagnosis of β-thalassemia major was based on family history, complete transfusion dependence, and hemoglobin electrophoresis. In 3 patients, diagnosis was confirmed by β-globin gene mapping. CD34+ progenitor cells were isolated from mononuclear cells using Midi-MACS columns (Miltenyi Biotech, Auburn, CA).20 CD34+ samples with less than 90% purity after MACs isolation were subjected to a second sort on FACS-Vantage flow cytometer to a more than 99% purity.
CD34+ cells were suspended overnight in transduction medium (X-vivo 15 medium [Biowhittaker, Walkersville, MD] containing the following recombinant human cytokines, all at 100 ng/mL: interleukin-6, Flt-3 ligand, thrombopoietin, and stem cell factor) in the presence of deoxynucleoside triphosphate (10 mM) and protamine sulfate (1 μg/mL) on plates coated with retronectin (Takara Shuzo, Japan).20 The following day, 2 × 106 to 9 × 106 cells were suspended in 100 μL lentiviral supernatants at multiplicity of infection (MOI) ranging from 1 to 14 at a viral concentration of 3 × 107 to 2 × 108 IU/mL. This process was repeated a second time, 4 hours apart. Cells were washed the following day, and portions of transduced cells were either plated in methylcellulose medium for colony-forming assays, 20 placed in liquid unilineage erythroid cultures, 28 or injected into sublethally irradiated (400 cGy) β2mnull nonobese diabetic–severe combined immunodeficient (NOD-SCID) mice (Figure 1).
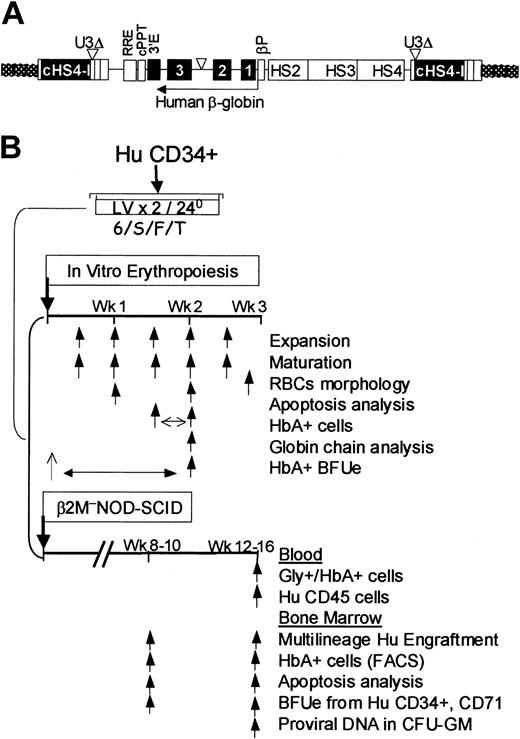
Integrated vector and experimental design. (A) The BGI vector was constructed using an SIN lentiviral backbone containing a 1.2-kb cHS4 insulator (cHS4-I) element inserted to replace the 398-bp U3 promoter and/or enhancer deletion (U3Δ). Upon proviral integration into host genome, the U3 region containing the cHS4 is copied over to the 5′LTR. A 3.1-kb human β-globin LCR region consisting of hypersensitive sites (HS) 2, 3, and 4; β-globin promoter (βPr; 254 bp); the β-globin gene (with a 372-bp deletion in IVS2); and the 3′ enhancer (3′E) were cloned in reverse orientation to the viral transcriptional unit downstream of the rev response element (RRE) and the central polypurine tract (cPPT). (B) Experimental design. Cryopreserved normal and thalassemia major bone marrow CD34+ cells were thawed simultaneously and transduced twice in the presence of recombinant human IL-6, stem cell factor, Flt-3 ligand, and thrombopoietin (6/S/F/T) within 24 hours. Cells were washed and portions of cells were plated in vitro, in erythroid liquid cultures, in semisolid medium for colony-forming assays, and transplanted into β2mnull NOD-SCID mice. Arrows depict serial time points at which various analyses were performed.
Integrated vector and experimental design. (A) The BGI vector was constructed using an SIN lentiviral backbone containing a 1.2-kb cHS4 insulator (cHS4-I) element inserted to replace the 398-bp U3 promoter and/or enhancer deletion (U3Δ). Upon proviral integration into host genome, the U3 region containing the cHS4 is copied over to the 5′LTR. A 3.1-kb human β-globin LCR region consisting of hypersensitive sites (HS) 2, 3, and 4; β-globin promoter (βPr; 254 bp); the β-globin gene (with a 372-bp deletion in IVS2); and the 3′ enhancer (3′E) were cloned in reverse orientation to the viral transcriptional unit downstream of the rev response element (RRE) and the central polypurine tract (cPPT). (B) Experimental design. Cryopreserved normal and thalassemia major bone marrow CD34+ cells were thawed simultaneously and transduced twice in the presence of recombinant human IL-6, stem cell factor, Flt-3 ligand, and thrombopoietin (6/S/F/T) within 24 hours. Cells were washed and portions of cells were plated in vitro, in erythroid liquid cultures, in semisolid medium for colony-forming assays, and transplanted into β2mnull NOD-SCID mice. Arrows depict serial time points at which various analyses were performed.
Colonies were scored and picked at 2 weeks. Liquid cultures were studied for erythroid cell expansion, differentiation (Wright-Giemsa stains on cytospins), β-globin production (via high-performance liquid chromatography (HPLC) and FACS, as described in the section below), and apoptosis (annexin-V labeling) biweekly, as previously described.29 Enucleated RBCs were isolated using Hoechst labeling and FACS.28
Vector copy numbers were determined using semiquantitative PCR with vector-specific primers designed in the 5′ region of the provirus: forward primer 5′-AACAGGGACCTGAAAGCGAAA-3′, reverse primer 5′-ACTATTCTTTCCCCTGCACTG-3′), and thermocycled at 94°C × 5 minutes, 18 cycles of 94°C × 30 seconds, 60°C × 30 seconds, 72°C × 60 seconds, and 72°C × 5 minutes to give a vector-specific band. An MEL cell clone containing 4 copies of the integrated provirus was used to generate a standard curve.
β-globin production: HbA staining and FACS analyses
The cells were fixed in 60 μL 4% paraformaldehyde for 60 minutes at room temperature, washed once with phosphate-buffered saline (PBS), and the pellet resuspended in 50 μL 100% methanol for 5 minutes. The fixed cells were then washed with PBS, and nonspecific antibody (Ab) binding was blocked using 75 μL 5% nonfat milk for 10 minutes at room temperature. Subsequently, cells were washed in PBS, pelleted, and permeabilized with 10 μL Caltag Reagent B (Caltag Laboratories, Burlingame, CA). The cells were divided into 2 tubes and stained with either anti–Zeta globin-fluorescein isothiocyanate (FITC) (1 μg/106 cells) as a negative control or anti–HbA-FITC (1 μg/106 cells) (PerkinElmer, Norton, OH) for 30 minutes at room temperature in the dark. Unbound Abs were removed by a final wash with PBS before they were analyzed on FACS Calibur (BDIS).
β-globin production: HPLC analyses for individual globin chains
Erythroid cells from in vitro cultures were resolved by reverse-phase HPLC.28
In vivo human xenograft experiments
Four- to 6-week-old β2mnull NOD-SCID mice (Jackson Laboratories, Bar Harbor, ME) were maintained in accordance with the policies of the local Institutional Animal Care and Use Committee at CHLA. Mice were splenectomized under general anesthesia and allowed to recover for 5 days following the surgery to allow survival of human RBC progeny in circulation (P.M., unpublished results, 2004), prior to intrafemoral delivery of CD34+ cells.31,32 Blood and bone marrow were analyzed at weeks 10 and 12 to 16 following transplantation. Intraperitoneal injections of recombinant human cytokines (erythropoietin 10 IU, stem cell factor, and granulocyte-macrophage colony-stimulating factor, 10 ng each) were given 3 times a week for 5 doses just prior to bone marrow analysis.33 Bone marrow was analyzed for multilineage engraftment (human CD45+, CD19+, CD33+, CD71+, and glycophorin A+ cells) and for HbA and annexin-V. Human progenitors and erythroid progenitors (CD34+/CD71+/glycophorin A+) cells were isolated from the bone marrow by labeling marrow with FITC-conjugated antihuman CD71 and CD34 and glycophorin A Ab, followed by secondary labeling with anti-FITC microbeads and immunomagnetic selection, and plated in colony-forming assays. Although CD71 and glycophorin A would also co-isolate mature human erythroid cells, they were added with the CD34 Ab to enrich for erythroid progenitors that would coexpress CD34 and CD71/glycophorin A. We have shown expression of glycophorin A and CD71 on CD34+ cells that give rise to higher burst-forming unit–erythroid (BFUe) and erythroid progeny from CD34+ and 34+/CD38 cells from patients with thalassemia and sickle cell disease.29
Results
Human thalassemia major bone marrow CD34+ cells from 4 patients were transduced with a SIN-lentivirus vector termed BGI containing the cHS4 insulator inserted in the SIN deletion of the 3′ LTR, 3.1 kb of the β-globin LCR, and the human β-globin gene driven by the β-globin promoter in the opposite orientation to the vector transcript (Figure 1A). Two of the thalassemia major patients were β0 thalassemia, one patient was compound heterozygous for 2 β+ mutations, and one patient was compound heterozygous for a β0 and a β+ mutation. All 4 patients had 4 intact α genes, and all of them were completely transfusion dependent since infancy. Cryopreserved thalassemia major bone marrow (TBM) and normal bone marrow (NBM) CD34+ cells were thawed simultaneously for each set of experiments. NBM CD34+ cells were mock transduced (and in some experiments, transduced with a modified erythroid-specific GFP-encoding vector I8HKGW20 that additionally included the cHS4 insulator element in the U3 region; termed K6I). TBM CD34+ cells were mock transduced or transduced with the BGI vector. The experimental design of the in vitro and in vivo experiments is shown in Figure 1B.
Effective erythropoiesis from vector-transduced human thalassemia major bone marrow CD34+ cells in vitro
The transduced CD34+ cells were placed in liquid cultures that promote unilineage erythroid differentiation, recapitulating normal and thalassemia erythropoiesis that is observed in vivo.28,29 Erythroid cell expansion and differentiation were analyzed biweekly for 2 to 3 weeks. BGI-transduced TBM cultures were indistinguishable from NBM cultures (either mock transduced or those transduced with a GFP-encoding K6I vector) with regards to erythroid differentiation (Figure 2A-C) and erythroid expansion (Figure 2E). While NBM erythroid cells underwent normal erythroid differentiation with hemoglobinization occurring from the polychromatophil normoblast stage to intensely hemoglobinized orthochromic normoblasts, this feature was distinctly absent in mock-transduced TBM cultures. TBM-BGI cultures, on the other hand, closely resembled NBM erythroid differentiation. Unlike NBM and TBM-BGI cultures, enucleation events were rare in TBM cultures. We next labeled 2- to 3-week-old cultures with a supravital DNA-binding dye, Hoechst 33342, and sorted the enucleated RBCs by FACS. NBM RBCs derived in vitro were mainly reticulocytes, showing the normal puckered appearance and normal discoid-shaped RBCs, unlike control TBM RBCs. The latter were rare and the few present were dysmorphic. TBM-BGI RBCs, however, were indistinguishable from NBM-derived RBCs (Figure 2D).
Effective erythropoiesis from vector-transduced human thalassemia major bone marrow CD34+ cells in vitro. Wright-Giemsa–stained cytospins of predominant cell types in erythroid cultures. (A) Cells are mainly pronormoblasts in NBM, TBM, and TBM-BGI at day 4, (B) orthochromic normoblasts in NBM and TBM-BGI, but polychromatophilic normoblasts in TBM, at day 13. (C) Enucleated RBCs produced in NBM and TBM-BGI at day 17, while TBM shows apoptotic cells. (D) Differential interference contrast microscopy of Hoechst 33342–negative cells (enucleated RBCs) sorted by FACS showing normal reticulocyte and discocyte morphology of NBM and TBM-BGI RBC. Occasional RBCs derived from TBM were dysmorphic. (E) Fold expansion of erythroid cultures derived from CD34+ cells (n = 4): mock-transduced NBM (⋄), K6I-transduced NBM (▪), mock-transduced TBM (▴), and BGI-transduced TBM (▵). The mean fold expansion at day 13 was NBM 356 ± 22, NBM K6I 360 ± 101, TBM 110 ± 31, TBM-BGI 308 ± 28; and at day 17 was NBM 494 ± 36, NBM K6I 498 ± 119, TBM 108 ± 36, TBM-BGI 458 ± 78 (P < .001 and P < .002 for NBM versus TBM and P = .1 and P = .3 for NBM versus TBM-BGI, at day 13 and day 17, respectively). (F) Representative apoptosis analysis using annexin-V labeling of NBM, TBM, and TBM-BGI erythroid cultures. (G) Quantification of apoptotic (annexin-V+) cells at day 7 and day 14 from the 4 experiments. NBM (filled bars), TBM (open bars), and TBM-BGI (hatched bars). Day 7: P < .01 NBM versus TBM; P < .08 NBM versus TBM-BGI; day 14: P < .004 NBM versus TBM; P < .1 NBM versus TBM-BGI.
Effective erythropoiesis from vector-transduced human thalassemia major bone marrow CD34+ cells in vitro. Wright-Giemsa–stained cytospins of predominant cell types in erythroid cultures. (A) Cells are mainly pronormoblasts in NBM, TBM, and TBM-BGI at day 4, (B) orthochromic normoblasts in NBM and TBM-BGI, but polychromatophilic normoblasts in TBM, at day 13. (C) Enucleated RBCs produced in NBM and TBM-BGI at day 17, while TBM shows apoptotic cells. (D) Differential interference contrast microscopy of Hoechst 33342–negative cells (enucleated RBCs) sorted by FACS showing normal reticulocyte and discocyte morphology of NBM and TBM-BGI RBC. Occasional RBCs derived from TBM were dysmorphic. (E) Fold expansion of erythroid cultures derived from CD34+ cells (n = 4): mock-transduced NBM (⋄), K6I-transduced NBM (▪), mock-transduced TBM (▴), and BGI-transduced TBM (▵). The mean fold expansion at day 13 was NBM 356 ± 22, NBM K6I 360 ± 101, TBM 110 ± 31, TBM-BGI 308 ± 28; and at day 17 was NBM 494 ± 36, NBM K6I 498 ± 119, TBM 108 ± 36, TBM-BGI 458 ± 78 (P < .001 and P < .002 for NBM versus TBM and P = .1 and P = .3 for NBM versus TBM-BGI, at day 13 and day 17, respectively). (F) Representative apoptosis analysis using annexin-V labeling of NBM, TBM, and TBM-BGI erythroid cultures. (G) Quantification of apoptotic (annexin-V+) cells at day 7 and day 14 from the 4 experiments. NBM (filled bars), TBM (open bars), and TBM-BGI (hatched bars). Day 7: P < .01 NBM versus TBM; P < .08 NBM versus TBM-BGI; day 14: P < .004 NBM versus TBM; P < .1 NBM versus TBM-BGI.
The different stages of erythroid maturation at serial days in culture were quantified by performing differential counts on cytospins of liquid cultures (Table 1). Control TBM cultures typically differentiated like those from NBM for 1 week. Thereafter, TBM erythroid cells arrested at the polychromatophil normoblast stage, with very little progression to the orthochromic normoblast stage or enucleation to RBCs. However, TBM-BGI CD34+ cells showed erythroid differentiation that was indistinguishable from NBM, resulting in serial progression from the pronormoblast, basophilic normoblast, polychromatophilic normoblast, orthochromic normoblast, and enucleated red cells at serial time points in culture.
Differential counts on Wright-Giemsa–stained cytospins from NBM, TBM, and TBM-BGI CD34+ cells from all 4 patients with thalassemia major after different days in culture showing the erythropoietic differentiation
. | Pronormoblast . | Basophilic normoblast . | Polychromatophilic normoblast . | Orthochromic normoblast . | RBC . | WBC . |
|---|---|---|---|---|---|---|
| NBM | ||||||
| d4 | 46 ± 5* | 43 ± 5* | 2 ± 0 | 0 ± 0 | 0 ± 0† | 9 ± 1 |
| d7 | 22 ± 4* | 42 ± 4* | 26 ± 4* | 5 ± 4 | 1 ± 1† | 5 ± 2 |
| d10 | 12 ± 2 | 22 ± 5* | 34 ± 3* | 23 ± 9* | 4 ± 1† | 7 ± 2 |
| d13 | 8 ± 1 | 15 ± 4 | 23 ± 3* | 40 ± 5* | 11 ± 2† | 7 ± 2 |
| d17 | 4 ± 2 | 10 ± 3 | 25 ± 3* | 41 ± 4* | 12 ± 3† | 7 ± 1 |
| TBM | ||||||
| d4 | 48 ± 5* | 39 ± 3* | 5 ± 2 | 0 ± 0 | 0 ± 0 | 9 ± 1 |
| d7 | 21 ± 3* | 36 ± 2* | 30 ± 3* | 6 ± 4 | 1 ± 2† | 5 ± 1 |
| d10 | 11 ± 3 | 25 ± 5* | 52 ± 5* | 4 ± 2 | 1 ± 1† | 9 ± 2 |
| d13 | 8 ± 4 | 16 ± 6 | 49 ± 7* | 11 ± 4 | 1 ± 1† | 11 ± 4 |
| d17 | 6 ± 3 | 16 ± 3 | 49 ± 7* | 15 ± 4 | 3 ± 1† | 12 ± 2 |
| TBM-BGI | ||||||
| d4 | 49 ± 6* | 36 ± 8* | 3 ± 1 | 0 ± 0 | 0 ± 0 | 13 ± 2 |
| d7 | 16 ± 6* | 36 ± 8* | 28 ± 3* | 11 ± 8 | 1 ± 1† | 10 ± 3 |
| d10 | 8 ± 4 | 20 ± 7 | 33 ± 5* | 28 ± 11* | 5 ± 2† | 7 ± 2 |
| d13 | 7 ± 3 | 14 ± 1 | 30 ± 5* | 34 ± 8* | 10 ± 3† | 6 ± 2 |
| d17 | 5 ± 2 | 13 ± 3 | 21 ± 7 | 35 ± 5* | 14 ± 3† | 13 ± 4 |
. | Pronormoblast . | Basophilic normoblast . | Polychromatophilic normoblast . | Orthochromic normoblast . | RBC . | WBC . |
|---|---|---|---|---|---|---|
| NBM | ||||||
| d4 | 46 ± 5* | 43 ± 5* | 2 ± 0 | 0 ± 0 | 0 ± 0† | 9 ± 1 |
| d7 | 22 ± 4* | 42 ± 4* | 26 ± 4* | 5 ± 4 | 1 ± 1† | 5 ± 2 |
| d10 | 12 ± 2 | 22 ± 5* | 34 ± 3* | 23 ± 9* | 4 ± 1† | 7 ± 2 |
| d13 | 8 ± 1 | 15 ± 4 | 23 ± 3* | 40 ± 5* | 11 ± 2† | 7 ± 2 |
| d17 | 4 ± 2 | 10 ± 3 | 25 ± 3* | 41 ± 4* | 12 ± 3† | 7 ± 1 |
| TBM | ||||||
| d4 | 48 ± 5* | 39 ± 3* | 5 ± 2 | 0 ± 0 | 0 ± 0 | 9 ± 1 |
| d7 | 21 ± 3* | 36 ± 2* | 30 ± 3* | 6 ± 4 | 1 ± 2† | 5 ± 1 |
| d10 | 11 ± 3 | 25 ± 5* | 52 ± 5* | 4 ± 2 | 1 ± 1† | 9 ± 2 |
| d13 | 8 ± 4 | 16 ± 6 | 49 ± 7* | 11 ± 4 | 1 ± 1† | 11 ± 4 |
| d17 | 6 ± 3 | 16 ± 3 | 49 ± 7* | 15 ± 4 | 3 ± 1† | 12 ± 2 |
| TBM-BGI | ||||||
| d4 | 49 ± 6* | 36 ± 8* | 3 ± 1 | 0 ± 0 | 0 ± 0 | 13 ± 2 |
| d7 | 16 ± 6* | 36 ± 8* | 28 ± 3* | 11 ± 8 | 1 ± 1† | 10 ± 3 |
| d10 | 8 ± 4 | 20 ± 7 | 33 ± 5* | 28 ± 11* | 5 ± 2† | 7 ± 2 |
| d13 | 7 ± 3 | 14 ± 1 | 30 ± 5* | 34 ± 8* | 10 ± 3† | 6 ± 2 |
| d17 | 5 ± 2 | 13 ± 3 | 21 ± 7 | 35 ± 5* | 14 ± 3† | 13 ± 4 |
Data are represented as mean ± SEM from 200 cells counted from 4 different TBM patients and normal controls; P < .01 (NBM vs TBM), p = NS (NBM vs TBM-BGI).
RBCs indicate red blood cells; WBC, white blood cells.
The predominant stages of maturation on any particular day in culture.
Mature RBCs.
Cultures were assessed for apoptotic cells, a feature characteristic of thalassemia major erythropoiesis.29 While NBM cultures had very few apoptotic cells (1% ± 0.5%) as assessed by annexin-V labeling, there were significant proportions of apoptotic cells in control TBM cultures (49% ± 12% at day 14). However, the proportions of apoptotic cells in TBM-BGI cultures were negligible (2% ± 1%), as seen in NBM cultures (NBM versus TBM, P < .004; NBM versus TBM-BGI, P = .1; Figure 2F-G). These results in TBM are similar to previously reported findings, where we have shown arrest at the polychromatophil stage of erythroid differentiation and apoptosis of this population as the cause of ineffective erythropoiesis in TBM.29 Taken together, these data show normal erythroid expansion and maturation of BGI-transduced TBM progenitor cells, with reversal of apoptosis and effective RBC production, identical to NBM cultures.
Gene transfer efficiency and β-globin production in transduced thalassemia bone marrow burst-forming units–erythroid
To determine gene transfer efficiency and intensity of HbA expression, we plated transduced CD34+ cells from NBM, TBM, and TBM-BGI in methylcellulose colony-forming assays from the 4 patients and analyzed 20 individual erythroid burst-forming units (BFUe's) per arm in each experiment for β-globin by intracellular staining for HbA followed by FACS. Gene transfer efficiency of the lentiviral vector in the CD34+ progenitors was determined by assessing the proportion of BFUe colonies that expressed the human β-globin transgene. The clonogenicity of TBM, TBM-BGI, and NBM was similar (data not shown), since TBM BFUe's have significant amounts of fetal globin in this colony-forming unit (CFU) assay34 that ameliorates the globin chain imbalance. All of the BFUe's from NBM CD34+ cells expressed HbA at a clonal level, in contrast to TBM BFUe's, where only occasional BFUe's (5% ± 2.5%) showed minimal HbA expression (Figure 3). However, 86% ± 5% BFUe's from TBM-BGI expressed HbA, showing a high transduction efficiency. The transduction efficiency achieved in the 4 experiments was 75%, 100%, 90%, and 80% (Figure 3).
High-level gene transfer and β-globin production in individual BFUe's from thalassemia major bone marrow transduced with the BGI vector. Individual BFUe's were picked at 2 weeks and HbA analysis performed after intracellular labeling of half the colony with human zeta-globin (A) as a negative control and the other half with HbA (B) and analyzed by FACS. Panels C to F show the MFI from 20 individual BFUe colonies from NBM, TBM, and TBM-BGI from experiments 1, 2, 3, and 4 respectively. The average MFIs ± SEMs of HbA were as follows: experiment 1, NBM 549 ± 34, TBM 17 ± 4, TBM-BGI 304 ± 41; experiment 2, NBM 140 ± 6, TBM 4 ± 2, TBM-BGI 118 ± 4; experiment 3, NBM 132 ± 8, TBM 44 ± 5, TBM-BGI 167 ± 11; experiment 4, NBM 650 ± 49, TBM 33 ± 9, TBM-BGI 369 ± 39. The horizontal lines in panels C-F represent the average MFI of the 20 BFUe's in that group.
High-level gene transfer and β-globin production in individual BFUe's from thalassemia major bone marrow transduced with the BGI vector. Individual BFUe's were picked at 2 weeks and HbA analysis performed after intracellular labeling of half the colony with human zeta-globin (A) as a negative control and the other half with HbA (B) and analyzed by FACS. Panels C to F show the MFI from 20 individual BFUe colonies from NBM, TBM, and TBM-BGI from experiments 1, 2, 3, and 4 respectively. The average MFIs ± SEMs of HbA were as follows: experiment 1, NBM 549 ± 34, TBM 17 ± 4, TBM-BGI 304 ± 41; experiment 2, NBM 140 ± 6, TBM 4 ± 2, TBM-BGI 118 ± 4; experiment 3, NBM 132 ± 8, TBM 44 ± 5, TBM-BGI 167 ± 11; experiment 4, NBM 650 ± 49, TBM 33 ± 9, TBM-BGI 369 ± 39. The horizontal lines in panels C-F represent the average MFI of the 20 BFUe's in that group.
HbA analyses demonstrated the same pattern of expression in NBM and TBM-BGI BFUe's (representative BFUe's shown in Figure 3A-B). The HbA mean fluorescence intensity (MFI) of the TBM-BGI–derived BFUe colonies were comparable to that seen in NBM-derived BFUe colonies (Figure 3C-F), suggesting equivalent amounts of β-globin in the erythroid cells in TBM-BGI and NBM.
Normal levels of HbA and β-globin production in transduced thalassemia bone marrow erythroid liquid cultures
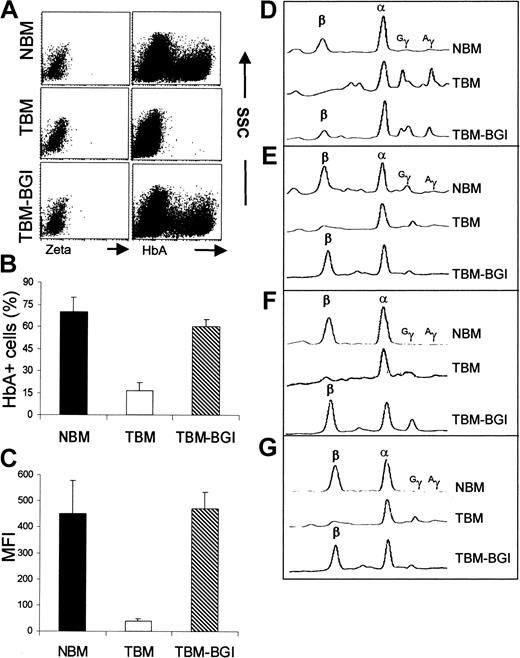
HbA determination by FACS analysis on the liquid cultures showed results very similar to the clonal data. While NBM CD34+ cell-derived erythroid liquid cultures showed robust HbA expression in a large proportion of cells, TBM cultures had very little HbA expression confined to few cells. Representative FACS analysis shown in Figure 4A demonstrates that TBM-BGI cultures showed comparable proportion of HbA+ cells as seen in NBM cultures and have a similar MFI, in contrast to control TBM cultures that had negligible HbA expression.
Normal levels of HbA and β-globin production in transduced thalassemia bone marrow erythroid liquid cultures. (A) FACS analysis of a 12-day erythroid culture from NBM, TBM, and TBM-BGI with the panels on the left showing the negative controls labeled with zeta-globin and the panels on the right showing HbA labeling. (B) The mean proportion (mean ± SEM; n = 4) of HbA+ cells in culture between days 10 and 12 was 70% ± 11% in NBM, 16% ± 6% in TBM, and 60% ± 5% in TBM-BGI; P < .001 NBM versus TBM, P < .2 NBM versus TBM-BGI. (C) The MFI of HbA in the same cultures was 451 ± 141 in NBM, 39 ± 8 in TBM, and 469 ± 72 in TBM-BGI; P < .001 NBM versus TBM, P = .45 NBM versus TBM-BGI. (D-G) Reverse phase HPLC analysis on the cells from liquid cultures done at 2 weeks of culture from the 4 individual experiments showing the β, α, Gγ, and Aγ globin chains marked in NBM, TBM, and TBM-BGI.
Normal levels of HbA and β-globin production in transduced thalassemia bone marrow erythroid liquid cultures. (A) FACS analysis of a 12-day erythroid culture from NBM, TBM, and TBM-BGI with the panels on the left showing the negative controls labeled with zeta-globin and the panels on the right showing HbA labeling. (B) The mean proportion (mean ± SEM; n = 4) of HbA+ cells in culture between days 10 and 12 was 70% ± 11% in NBM, 16% ± 6% in TBM, and 60% ± 5% in TBM-BGI; P < .001 NBM versus TBM, P < .2 NBM versus TBM-BGI. (C) The MFI of HbA in the same cultures was 451 ± 141 in NBM, 39 ± 8 in TBM, and 469 ± 72 in TBM-BGI; P < .001 NBM versus TBM, P = .45 NBM versus TBM-BGI. (D-G) Reverse phase HPLC analysis on the cells from liquid cultures done at 2 weeks of culture from the 4 individual experiments showing the β, α, Gγ, and Aγ globin chains marked in NBM, TBM, and TBM-BGI.
To quantify the β-globin produced from these vectors, cell lysates from liquid cultures from the 4 experiments were subjected to a reverse phase HPLC analysis (Figure 4D-F). There was negligible β-globin expression in TBM cultures, with a compensatory increase in γ-globin chains in some cultures. β-globin production in TBM-BGI cultures was comparable to that produced in NBM in all but the first experiment (Figure 4D). In the latter, the amount of β-globin in TBM-BGI cultures was 58% of that in NBM at this time point in culture and corresponded to the transduction efficiency shown in BFUe colonies (Figure 3C). Overall, β-globin chains comprised 70% ± 5% of all β-like globins in NBM, 7.3% ± 7% in TBM, and 75% ± 14% in TBM-BGI cultures (P < .005 NBM versus TBM; P = .34 NBM versus TBM-BGI). Of note, the β-globin production by HPLC correlated well with HbA MFI by FACS (Figure 4). Vector copy numbers, determined by semiquantitative PCR analysis, showed a mean of 2 proviral copies per cell (1.1, 2.6, 2.2, and 1.4 copies per cell in the 4 experiments). When corrected for gene-transfer efficiency, the vector copy numbers were 1.5, 2.6, 2.4, and 1.8 in the 4 experiments, respectively, with an average of 2.2 vector copies per cell.
Genetic correction was sustained in vivo in β2mnull NOD-SCID mice with multilineage engraftment
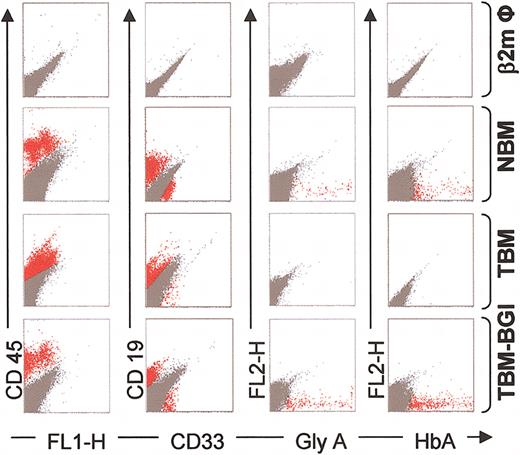
We injected mock-transduced NBM and TBM CD34+ cells and BGI-transduced TBM CD34+ cells into 4- to 6-week-old splenectomized, sublethally irradiated β2mnull NOD-SCID mice (NBM n = 11, TBM n = 11, TBM-BGI n = 13) and evaluated bone marrow at 8 to 10 weeks and bone marrow, blood, and human CFUs at 12 to 14 weeks following transplantation. Although the overall engraftment (CD45+, CD71+ cells and the CD19 population) was much lower than previously observed in this xenograft model, 33 this was likely a result of splenectomies performed to prevent destruction of circulating human erythroid populations (P.M., unpublished results, 2004). Nevertheless, there was multilineage engraftment, with 0.1% to 5% human CD45+ cells, 0.1% to 0.5% human CD33+ cells, and 0.5% to 2% human CD19+ cells. Figure 5 shows a FACS analysis of β2mnull NOD-SCID mouse bone marrow, performed 10 to 12 weeks following transplantation with human NBM, TBM, and TBM-BGI CD34+ cells. Untransplanted β2mnull NOD-SCID mice also were analyzed simultaneously. We observed CD45+, CD33+, CD19+, and glycophorin A+ cells in these mice, showing multilineage human cell engraftment. Glycophorin A expression was not seen in the TBM group of mice, despite multilineage human cell engraftment. We have observed similar reduced-to-absent glycophorin A expression in differentiated TBM erythroid cultures in vitro (data not shown), conceivably due to α-globin–induced membrane damage in thalassemia erythroid cells. NBM group of mice demonstrated HbA-expressing cells in bone marrow (0.1%-5%), while TBM group had a negligible proportion (0%-0.08%) of HbA-expressing cells. TBM-BGI group of mice showed a similar proportion of HbA+ cells as seen in the NBM group of mice, confirming that β-globin expression was sustained due to transduction of primitive hematopoietic progenitor cells. In the NBM group of mice, the proportion of HbA-expressing cells to glycophorin A expressing cells was 95% ± 9%, while in the TBM-BGI group of mice the proportion of HbA-expressing cells to glycophorin A–expressing cells was 89% ± 8%. The HbA MFI was similar in NBM and TBM-BGI mice.
Multilineage engraftment and β-globin expression in β2mnull NOD-SCID mice. FACS analysis of β2mnull NOD-SCID mouse bone marrow, performed 12 to 16 weeks following transplant with human CD34+ cells: β2m Φ (no human cells, row 1), NBM (mock transduced, row 2), TBM (mock transduced, row 3), and TBM-BGI (BGI transduced, row 4). Representative dot-plots showing human CD45 (y-axis, column 1), human CD19 (y-axis, column 2), human CD33 (x-axis, column 2), and human glycophorin A (x-axis, column 3) expression from one mouse in each group. Bone marrow also was labeled intracellularly with HbA Ab, and dot-plots showing HbA expression in the bone marrow of these mice (x-axis, column 4) are shown. All samples in columns 1 to 3 were gated on the basis of appropriate isotype controls, and events falling within the isotype control gate are shown in dark gray. All events labeled positive with the respective human antibodies are shown in red. For intracellular HbA staining, human zeta-globin was used as the negative control, and events falling within this gate are shown in dark gray. HbA-labeled events falling outside this gate are shown in red.
Multilineage engraftment and β-globin expression in β2mnull NOD-SCID mice. FACS analysis of β2mnull NOD-SCID mouse bone marrow, performed 12 to 16 weeks following transplant with human CD34+ cells: β2m Φ (no human cells, row 1), NBM (mock transduced, row 2), TBM (mock transduced, row 3), and TBM-BGI (BGI transduced, row 4). Representative dot-plots showing human CD45 (y-axis, column 1), human CD19 (y-axis, column 2), human CD33 (x-axis, column 2), and human glycophorin A (x-axis, column 3) expression from one mouse in each group. Bone marrow also was labeled intracellularly with HbA Ab, and dot-plots showing HbA expression in the bone marrow of these mice (x-axis, column 4) are shown. All samples in columns 1 to 3 were gated on the basis of appropriate isotype controls, and events falling within the isotype control gate are shown in dark gray. All events labeled positive with the respective human antibodies are shown in red. For intracellular HbA staining, human zeta-globin was used as the negative control, and events falling within this gate are shown in dark gray. HbA-labeled events falling outside this gate are shown in red.
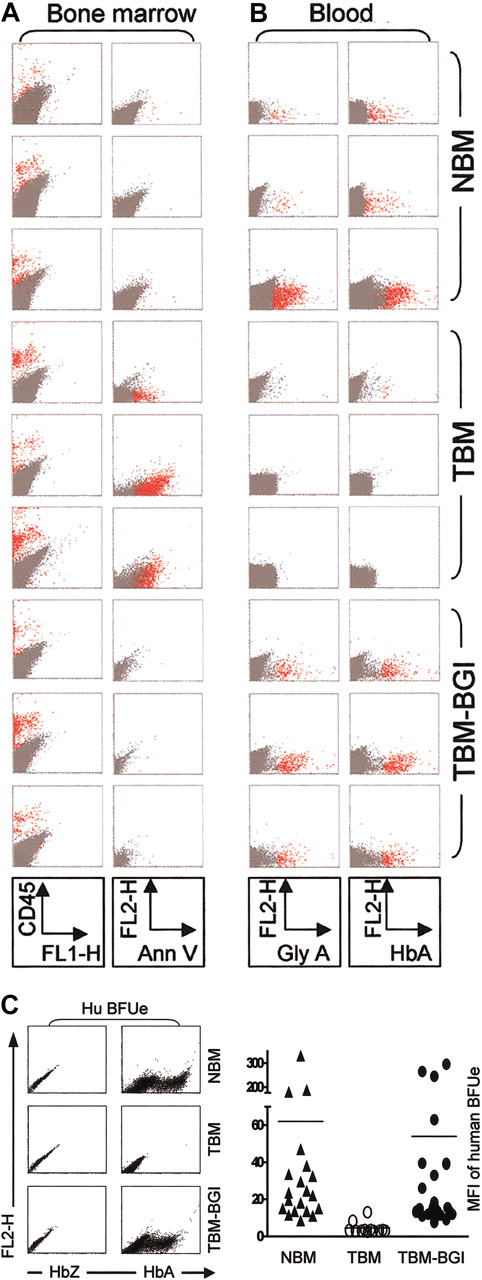
We next determined the presence of effective erythropoiesis and circulating erythroid cells in the xenografted mice in each group at 12 to 14 weeks, following 10 days of human cytokine stimulation.35 Figure 6A-B shows 3 representative mice from NBM, TBM, and TBM-BGI. Figure 6A shows that human CD45 cell engraftment was present in the bone marrow of all 9 mice. While there were negligible annexin-V–labeled cells in the bone marrow of NBM mice, there was a distinct annexin-V–labeled cell population in bone marrow of TBM mice. Bone marrow from TBM-BGI mice showed negligible annexin-V labeling, like NBM xenografts. Overall, cumulative results from all the xenografts showed 0.8% to 3% annexin-V+ cells in the bone marrow of the TBM mice and 0.01% to 0.2% annexin-V+ cells in the NBM and TBM-BGI mice.
Restoration of effective erythropoiesis and normal HbA production in xenografts. Representative dot-plots of 3 β2mnull NOD-SCID mice from each group (NBM, TBM, TBM-BGI) 12 to 16 weeks following transplantation. (A) Bone marrow labeled with anti–human CD45 Ab (column 1) showing human cell engraftment and showing apoptotic cells labeled with annexin-V (column 2). (B) Blood from the same mice was labeled with anti–human Ab to glycophorin A (column 3), showing circulating human erythroid cells. Blood also was labeled with anti–human HbAAb (column 4). All samples in columns 1 to 3 were gated on the basis of appropriate isotype controls, and events falling within this gate are shown in dark gray. All events labeled with the respective human antibodies are shown in red. For intracellular HbA staining, anti–human zeta-globin Ab was used as the negative control, and events falling within this gate are shown in dark gray. HbA-labeled events falling outside this gate are shown in red. (C) FACS analysis for HbA on individual human BFUe derived from human progenitors sorted from xenograft bone marrow. The top panel shows representative BFUe's from NBM, TBM, and TBM-BGI xenografts: zeta-globin and HbA expression are shown on the x-axes in columns 1 and 2, respectively. HbA MFI of individual BFUe's derived from different xenografts (NBM n = 20, TBM n = 11, TBM-BGI n = 23) were plotted (bottom panel). MFI of each BFUe is shown on the y-axis. The average HbA MFI of the BFUe's (plotted as a line) was NBM 62 ± 17, TBM 4 ± 1 and TBM-BGI 54 ± 17.
Restoration of effective erythropoiesis and normal HbA production in xenografts. Representative dot-plots of 3 β2mnull NOD-SCID mice from each group (NBM, TBM, TBM-BGI) 12 to 16 weeks following transplantation. (A) Bone marrow labeled with anti–human CD45 Ab (column 1) showing human cell engraftment and showing apoptotic cells labeled with annexin-V (column 2). (B) Blood from the same mice was labeled with anti–human Ab to glycophorin A (column 3), showing circulating human erythroid cells. Blood also was labeled with anti–human HbAAb (column 4). All samples in columns 1 to 3 were gated on the basis of appropriate isotype controls, and events falling within this gate are shown in dark gray. All events labeled with the respective human antibodies are shown in red. For intracellular HbA staining, anti–human zeta-globin Ab was used as the negative control, and events falling within this gate are shown in dark gray. HbA-labeled events falling outside this gate are shown in red. (C) FACS analysis for HbA on individual human BFUe derived from human progenitors sorted from xenograft bone marrow. The top panel shows representative BFUe's from NBM, TBM, and TBM-BGI xenografts: zeta-globin and HbA expression are shown on the x-axes in columns 1 and 2, respectively. HbA MFI of individual BFUe's derived from different xenografts (NBM n = 20, TBM n = 11, TBM-BGI n = 23) were plotted (bottom panel). MFI of each BFUe is shown on the y-axis. The average HbA MFI of the BFUe's (plotted as a line) was NBM 62 ± 17, TBM 4 ± 1 and TBM-BGI 54 ± 17.
Glycophorin A and HbA analysis was performed on peripheral blood obtained from the same mice that are shown in Figure 6A. NBM mice showed a small but distinct proportion of glycophorin A+ and HbA+ cells (0.01%-0.2%), which was negligible in the TBM group (Figure 6B). However, the TBM-BGI group of mice showed similar proportions of glycophorin A+ and HbA+ cells as seen in the NBM group. Therefore, like NBM, TBM-BGI progenitor cells were able to sustain effective erythropoiesis in vivo with circulating erythroid cells, in contrast to TBM progenitor cells.
Next, human progenitor cells and erythroid precursors (CD34+, CD71+, and GlyA+)36 were sorted from the mouse bone marrow and plated in methylcellulose CFU assays, and individual BFUe's and granulocyte macrophage colony-forming units (CFU-GMs) were analyzed after 2 weeks for HbA expression and presence of the provirus, respectively. Figure 6C, top panel, shows a representative BFUe from NBM, TBM, and TBM-BGI showing robust HbA expression in the NBM BFUe colonies. While there was negligible HbA expression in the TBM BFUe colonies, TBM-BGI BFUe colonies showed HbA expression similar to that of an NBM BFUe. The MFI of all BFUe colonies picked from the 3 groups of mice are shown in the bottom panel (Figure 6C). There was negligible HbA expression in BFUe's from the TBM group. Interestingly, the HbA MFI from BFUe's derived from NBM and TBM-BGI group of mice showed wide variability in expression, probably due to variable degrees of erythroid maturation of individual colonies. Nevertheless, the variability in HbA expression was similar in both the NBM and TBM-BGI groups.
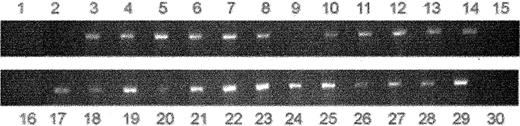
CFU-GM colonies from 6 TBM-BGI mice also were screened for the presence of provirus by PCR. Of 27 GM colonies, 24 were found to have vector-specific sequences, indicating a gene transfer efficiency of 89% (Figure 7). These data are similar to the transduction rate of 85% shown in BFUe colonies in vitro, suggesting high-efficiency transduction of primitive human hematopoietic progenitor cells with long-term correction.
Provirus was present in 89% of human myeloid colonies derived from xenografted TBM-BGI mice. CFU-GM colonies were picked and PCR analysis performed on DNA using vector-specific primers: lane 1, NBM; lane 2, TBM; lanes 3 to 29, TBM-BGI; and lane 30, Φ. Vector-specific bands were seen only in the CFU-GM colonies (in 24 of 27 colonies) derived from the TBM-BGI xenografts.
Provirus was present in 89% of human myeloid colonies derived from xenografted TBM-BGI mice. CFU-GM colonies were picked and PCR analysis performed on DNA using vector-specific primers: lane 1, NBM; lane 2, TBM; lanes 3 to 29, TBM-BGI; and lane 30, Φ. Vector-specific bands were seen only in the CFU-GM colonies (in 24 of 27 colonies) derived from the TBM-BGI xenografts.
Taken together, the xenograft data show (1) multilineage engraftment, (2) HbA production in thalassemia major bone marrow, accompanied by reversal of apoptosis and HbA+ BFUe's, (3) effective erythropoiesis with circulating HbA+ erythroid cells, and (4) presence of provirus in CFU-GM in the TBM-BGI mice, 12 to 16 weeks after transplantation. These data suggest transduction of a primitive multipotential progenitor cell in TBM-BGI group of mice, which were indistinguishable from the NBM group, and confirmed the in vitro results of successful correction of thalassemia major phenotype.
Discussion
We sought to develop a vector that would express human β-globin at levels higher than previously reported and that would have reduced position effects and improved vector biosafety, for effective gene therapy of human thalassemia major. We designed and tested a lentiviral vector that would express the human β-globin gene under control of its regulatory elements and be flanked with chromatin insulator elements upon integration into host hematopoietic cells. In this report, we show (1) high-level transduction of bone marrow progenitor cells from 4 patients with transfusion-dependent thalassemia major, (2) complete phenotypic and functional correction of the in vitro model of human thalassemia erythropoiesis, (3) levels of β-globin similar to that derived from normal bone marrow progenitors, and (4) effective human erythropoiesis with circulating β-globin producing human erythroid cells in genetically corrected xenografts at levels comparable to normal bone marrow xenograft controls. To the best of our knowledge, this is the first report of complete correction of human thalassemia major in vitro and in a xenograft model in vivo.
May et al12 were first able to stably transmit the human β-globin gene and its regulatory elements in lentiviral vectors and correct β-thalassemia in heterozygous mice, with an average increase of hemoglobin by 2 to 4 g/dL per copy of the integrated vector. However, this increase in hemoglobin level reported by them and similar reports in mice by others14-16 are insufficient to correct the phenotype of human thalassemia major and would theoretically convert a patient with thalassemia major (with hemoglobin levels ranging from 2 to 4 g/dL) into that with severe thalassemia intermedia (4-8 g/dL), as was confirmed in a recent mouse model of thalassemia major.17 Our results show complete correction of the phenotype and show near-normal levels of β-globin production with approximately 2 proviral copies per cell. It is to be noted, however, that an incomplete correction in mice (where human β-globin forms tetramers with mouse α-globin) may be an underestimate of the degree of correction that would be achieved with similar vectors in human cells (where natural tetramers of human α and β globins would be formed), and this may partially explain the success of our study. Determinations of increase in hemoglobin are not possible in the in vitro model or in the xenograft model and require testing in mice. These studies are under way in the laboratory. It is also conceivable that we have converted the thalassemia major (Hb 2-3 g/dL) into a thalassemia trait phenotype (hemoglobin 10-11 g/dL), which is asymptomatic in humans.
The high transduction efficiency into human CD34+ cells is comparable to previously published studies. Levasseur and colleagues16 show 85% βAS3-globin gene marking in mouse reticulocytes with vector copy numbers of 2.2. Sadelain and colleagues have shown similar results with 50% and 92% HbA+ cells in murine bone marrow with copy numbers of 1 and 1.9, respectively.12 The high gene transfer efficiency also may be due in part to a species-specific effect or a short transduction protocol. Lentiviral vectors transduce human cells at much higher efficiencies than mouse cells. Nguyen and colleagues37 have shown gene transfer efficiencies of approximately 80% in primary human hepatocytes with a MOI of 1 to 5, while rodent hepatocytes were transduced only to approximately 10% to 20%. Using a short transduction protocol, Ailles and colleagues38 and Levasseur and colleagues16 have achieved approximately 80% or greater transduction efficiency with lentiviral vectors in human CD34+ cells in NOD-SCID xenografts and sickle transgenic mice, respectively.
Of note, we observed slightly higher apoptosis at day 7 in TBM-BGI erythroid liquid cultures compared to NBM, although not statistically significant. This may be arising from the 15% untransduced progenitor progeny. In erythroid liquid cultures, where globin chain production mimics that seen in vivo, 28 presence of HbA may give the corrected progenitors a survival advantage. Persons et al39 have generated chimeras by transplanting different amounts of normal hematopoietic stem cells into thalassemia mice and show significant improvement in hemoglobin with approximately 20% engraftment. However, there should be minimal selection bias in colony-forming assays, where high amounts of HbF ameliorates the globin chain imbalance and therefore prevents apoptosis, 34 or in vivo, in the xenografts, where these mice are not anemic. We observe no differences in clonogenicity in the thalassemia versus normal bone marrow in colony-forming assays. These data are corroborated by similar clonal gene transfer levels seen in CFU-GM colonies from xenografts, 3 to 4 months of gene transfer, and equivalent results in HbA expression in NBM and TBM-BGI BFUe's.
Conceivably, the BGI vector may have increased hemoglobin levels more than those reported in previously published studies, and this increase may be attributed to incorporation of the insulator element. Expression of β/γ-globin reported in various mouse studies is highly variable.14,15,17 Incorporation of the cHS4 insulator may have reduced position effects and thereby improved expression, resulting in a predictable rise in β-globin. Emery and colleagues compared cHS4-containing insulated oncoretroviral vectors to analogous noninsulated vectors carrying the human γ-globin gene in MEL cells and in mouse transplantation models and found that flanking the γ-globin vector with the cHS4 insulator increases the likelihood of expression by nearly 10-fold by reducing position effects.22 Similar results on increased transgene expression and reduced PEV have been recently reported in vitro with SIN lentiviral vectors by Ramezani and colleagues.40
Moreover, the cHS4 insulator element is well characterized for its barrier function and enhancer blocking effects23 and therefore should result in reduced genotoxicity of the BGI vector, although this has not been formally tested in these experiments. The recent reports of insertional leukemogenesis in 2 of 10 patients who received gene therapy for X-linked SCID due to activation of LMO2 gene by the vector promoter and/or enhancer near the integrated provirus24 underscores the need for safer vectors that would be lineage specific and have enhancer-blocking effects.
In summary, we report successful correction of β-thalassemia major in a human model. The next important step will be to test the safety and gene transfer using these vectors in large animal models before they can be introduced into human trials. The recent report by Hanawa et al41 showing high-level long-term transduction of rhesus macaques with an SIV-based vector are very encouraging. Conceivably, strategies for selectively amplifying a genetically modified population in vivo also would be very useful, as it would decrease the need for myeloablation prior to transplanting the transduced hematopoietic stem cells into a patient.
Prepublished online as Blood First Edition Paper, August 3, 2004; DOI 10.1182/blood-2004-04-1427.
Supported by National Institutes of Health, Bethesda, MD, grants RO1-HL70135-01, 1P01HL073104-010004, and 1U54HL070595-010003.
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are deeply indebted to the thalassemia patients and their families who volunteered bone marrow samples for research. We would like to also thank Dr Jan Nolta for advice on xenograft transplantation; Dr Yasuyoshi Sohara and Dr Gordon Wu for assistance with intrafemoral injections and splenectomy, respectively; Lora Barsky and Mary Price for flow-sorting; the Division of Hematology-Oncology and the Division of Research Immunology/BMT, Childrens Center for Cancer and Blood Diseases, for help with obtaining patient samples; and Dr Donald B. Kohn for critical review of the manuscript.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal