Abstract
Outgrowth, long-term self-renewal, and terminal maturation of human erythroid progenitors derived from umbilical cord blood in serum-free medium can be modulated by steroid hormones. Homogeneous erythroid cultures, as characterized by flow cytometry and dependence on a specific mixture of physiologic proliferation factors, were obtained within 8 days from a starting population of mature and immature mononuclear cells. Due to previous results in mouse and chicken erythroblasts, the proliferation-promoting effect of glucocorticoids was not unexpected. Surprisingly, however, androgen had a positive effect on the sustained expansion of human female but not male erythroid progenitors. Under optimal conditions, sustained proliferation of erythroid progenitors resulted in a more than 109-fold expansion within 60 days. Terminal erythroid maturation was significantly improved by adding human serum and thyroid hormone (3,5,3′-triiodothyronine [T3]) to the differentiation medium. This resulted in highly synchronous differentiation of the cells toward enucleated erythrocytes within 6 days, accompanied by massive size decrease and hemoglobin accumulation to levels comparable to those in peripheral blood erythrocytes. Thus, obviously, different ligand-activated nuclear hormone receptors massively influence the decision between self-renewal and terminal maturation in the human erythroid compartment.
Introduction
Hematopoietic development within the erythroid lineage requires a delicate balance between the opposing effects of proliferation-promoting factors maintaining the renewal capacity of immature erythroid progenitors and differentiation-inducing factors required for successful terminal maturation of erythroid progenitors into red blood cells.1 In adult humans, erythroid differentiation produces about 2 × 1011 (roughly 20 g) red cells per day, representing the most vigorous proliferation process in the entire body. Because low numbers of erythrocytes are immediately life-threatening, erythropoiesis needs regulatory mechanisms temporarily altering the balance toward enhanced proliferation to cope with stress situations such as low oxygen levels at elevated altitudes (hypoxia) or massive blood loss.
In vivo, both renewal and maturation of human erythroid progenitors proceed in parallel in the bone marrow. It has thus been difficult to assess the contribution of particular signaling pathways and their deregulation during aberrant depletion of these progenitors, or their death on differentiation in anemia, versus unscheduled progenitor proliferation (as occurring in leukemogenesis). Most information was obtained from established cell lines and, more recently, primary animal cell models of chicken and mouse in defined media.1-3 The latter approach even allowed analysis of cells from genetically modified mice.4-6 For sustained proliferation, both avian and murine primary erythroblasts require cooperation between erythropoietin (Epo), stem cell factor (SCF), and glucocorticoids (dexamethasone [Dex]). Involvement of Epo and SCF was expected from their contribution to proliferation and survival of erythroid cells,7-9 whereas the stress hormone Dex massively prolonged progenitor proliferation (from 10 to 30 days in chickens, 7 to 20 days in mice), at the same time reducing their rate of spontaneous differentiation. Our idea that this might point to specific roles for glucocorticoids in stress erythropoiesis could be verified in vivo using mutant mice carrying a dimerizationdefective glucocorticoid receptor (GR-dim). In contrast to wildtype mice, GR-dim mice could not respond to hypoxia or experimental anemia with increased erythroblast renewal.10
Interestingly, activated leukemia oncogenes use the same signaling pathways driving transient renewal during stress erythropoiesis to induce permanent proliferation as well as differentiation arrest in leukemia. The v-ErbB oncogene product of avian erythroblastosis virus (AEV) or endogenous mouse c-ErbB can substitute for ligand activation of Epo receptor (EpoR) plus c-Kit, the SCF receptor.11,12 On the other hand, GR can be replaced by v-ErbA, the second AEV oncogene, a constitutively repressing variant of thyroid hormone receptor α (TRα)/c-ErbA.13
These observations indicated a need for corresponding studies in human erythroblasts under in vivo–like conditions. Although cooperation between Epo, SCF, and Dex induced renewal of human erythroblasts,14 the use of serum-containing media limited the usefulness of these culture conditions with respect to cell numbers and homogeneity of cells obtained. Human erythroid cell lines such as K562, yielding unlimited cell numbers, are even less useful because they proliferate in the absence of physiologic regulators and thus compromise mechanistic studies. Finally, techniques to expand erythroid progenitors from multipotent ones in 2or 3-step protocols15 yield cell populations that undergo sustained proliferation for less than 2 weeks, accompanied by high rates of spontaneous differentiation. Thus, contributions of individual exogenous factors to self-renewal versus maturation were difficult to assess by these approaches.
We addressed this problem by systematically exploring the renewal and differentiation requirements of erythroid progenitors from umbilical cord blood. Cord blood has received a great deal of attention as a source for hematopoietic stem cells (mainly CD34+) as an alternative to bone marrow stem cells in transplantation medicine.16-19 Furthermore, cord blood is a source of multipotent stem cells, which may replace human embryonic stem (ES) cells in future forms of therapy20 and highly enriched in committed hematopoietic progenitors, including those of the erythroid lineage.21
Here, we describe thoroughly optimized long-term serum-free culture conditions that allowed expansion into mass cultures of highly homogeneous human erythroid progenitors derived from umbilical cord blood. Cells could be expanded routinely for more than 45 days, undergoing up to 35 population doublings, which approaches the in vitro lifespan of primary fetal human fibroblasts. In these experiments, we confirmed the requirement of glucocorticoids (Dex)14 for sustained proliferation. More importantly, human erythroblasts exhibited a sex-specific promotion of proliferation via androgen. Finally, we optimized induction of synchronous terminal differentiation, generating fully mature, enucleated erythrocytes, which required thyroid hormone (3,5,3′-triiodo-l-thyronine [T3]) in synergy with Epo/insulin (Ins) and as yet unidentified factors from human serum.
Materials and methods
Isolation and culture of mononuclear cells from cord blood
Umbilical cord blood (normal, full-term deliveries; informed consent obtained; General Hospital, Vienna, Division of Gynecological Endocrinology) was delivered in 20 U/mL heparin. Erythrocytes were removed by mixing blood with ery-lysis buffer (1:25 vol/vol; 89.9 g ammonium chloride, 10 g KHCO3, 0.37 g EDTA [ethylenediaminetetraacetic acid]) and several washes with ice-cold phosphate-buffered saline (PBS) until the cell pellet appeared white. For initial expansion, 5 × 106 cells/mL were cultivated in serum-free medium (StemSpan; Stem Cell Technologies, Vancouver, BC, Canada) supplemented with Epo (2 U/mL Erypo Janssen-Cilag, Baar, Switzerland), the synthetic glucocorticoid Dex (1 μM; Sigma, St Louis, MO), insulin-like growth factor 1 (IGF-1; 40 ng/mL; Promega, Mannheim, Germany), SCF (100 ng/mL; R&D Systems, Minneapolis, MN), and lipids (40 μg/mL cholesterol-rich lipid mix; Sigma). Homogeneous cultures of erythroid progenitors established after several days were kept in the same medium at 2 × 106 cells/mL by daily partial medium changes. Proliferation kinetics and size distribution of cells were monitored daily using an electronic cell counter (CASY-1; Schärfe-System, Reutlingen, Germany); cumulative cell numbers were calculated as described.22 Proliferating erythroid progenitors could be frozen and thawed with high efficiency (> 90%).
Induction of differentiation
To induce terminal differentiation, proliferating erythroblasts were washed in ice-cold PBS and reseeded at 2 × 106 cells/mL in StemSpan supplemented with Epo (10 U/mL), Ins (4 × 10–4 immunizing unit [IU] = 10 ng/mL; Actrapid HM, Bagsvaerd, Denmark), the Dex antagonist ZK112993 (3 μM; referred to as ZK),23 iron-saturated human transferrin (1 mg/mL; Sigma), and 3% human male serum (Sigma). Differentiating erythroblasts were maintained at 2 to 4 × 106 cells/mL by daily cell counts and partial medium changes.
Cell morphology, histologic staining, and hemoglobin determination
Erythroblasts at various differentiation stages were cytocentrifuged onto glass slides and stained with histologic dyes and benzidine for hemoglobin as described.24 To quantitate hemoglobin, 50-μL aliquots of cultures were analyzed in triplicate by photometry after normalization for cell number and volume as described.25
Apoptosis assay
Cells (2 × 106) were fixed in 0.5 mL 8% paraformaldehyde in PBS for 30 minutes at room temperature and stored in 70% ethanol at –20°C. Cells were washed in PBS and incubated in 45 μL labeling plus 5 μL enzyme solution (fluorescein-deoxyuridine triphosphate; terminal deoxynucleotide transferase; In situ Cell Death Detection Kit, Roche, Mannheim, Germany) for 1 hour at 37°C. Cells were washed once, resuspended in PBS, and subjected to flow cytometry to determine percentages of TdT-mediated dUTP nick-end labeling (TUNEL)–positive cells.
Flow cytometry
Erythroblasts (1 × 106) were washed twice with PBS plus 1% fetal calf serum (FCS) and stained with fluorescently labeled antibodies against CD15 (fluorescein isothiocyanate [FITC]; PharMingen, San Diego, CA; catalogue no. 555401), CD19 (FITC; PharMingen, no. 555412), CD116 (FITC; PharMingen, no. 554532), glycophorin A (GPA; FITC; PharMingen, 559943), CD8 (phycoerythrin [PE]; PharMingen, no. 555367), CD33 (PE; PharMingen, no. 30945X), CD38 (PE; PharMingen, no. 555460), CD45RA (PE; PharMingen, no. 555489), CD56 (PE; PharMingen, no. 555516), CD71 (transferrin receptor; PE; PharMingen, no. 555537), CD117 (c-Kit, the SCF receptor; PE; PharMingen, no. 555714), CD3 (phycoerythrin-Texas red [ECD]; Coulter-Immunotech, Marseille, France, no. IM2705), CD45 (ECD; Coulter-Immunotech, no. IM2710), CD4 (PE-cyanin 5.1 [PC5]; Coulter Immunotech, no. IM2636), CD14 (PC5; Coulter-Immunotech, no. IM2640), and CD34 (PC5; Coulter-Immunotech, no. IM2648). Surface marker expression was analyzed by flow cytometry (FacScan or LSR, Becton Dickinson, Heidelberg, Germany); quantitation of cell populations positive for individual markers was performed with the Paint-a-gate software package (Becton Dickinson).
DNA profiles were determined in a PAS-III flow cytometer (Partec, Munich, Germany) after staining cellular DNA with 6 μM DAPI (4,6-diamidino-2-phenylindole-dihydrochloride). Percentages of cells in specific cell-cycle phases were calculated using a software package of the same manufacturer.26
Density gradient purification of hematopoietic cells
Density gradient centrifugation (> 10 × 106 cells, to optimize the yield) was used to remove dead and spontaneously differentiating cells. Cultures were transferred into tubes with 2 mL lymphocyte separation medium (Eurobio, Les Ulis Cedex B, France, 1.077 g/mL). After centrifugation (600g, 7 minutes; immature progenitors band between the phases, dead and differentiating cells are in the pellet) erythroblasts were transferred into another tube, counted, washed with PBS, and recultivated.
Results
In vitro mass culture of human erythroid progenitors from umbilical cord blood
Human erythroid progenitors were expanded from umbilical cord blood after selective lysis of mature erythrocytes (see “Materials and methods”) in serum-free medium (StemSpan) by using a combination of Epo, SCF, Dex (synthetic glucocorticoid), and IGF-1, some of which are typical for stress erythropoiesis10 (Table 1). From day 3 on, a small population of expanding erythroid progenitors became visible in cytospins, which was clearly detectable in an electronic cell analyzer (CASY) around day 6 as an increasing population of large, nonadherent cells (∼12 μm in diameter; Figure 1). From day 10 onward, morphologically homogeneous erythroid progenitors could be expanded into mass cultures (Figure 1), which proliferated exponentially for over 30 days, demonstrating a clear capacity for long-term self-renewal. At regular intervals, more mature or apoptotic cells were removed by density gradient centrifugation. After 27 to 30 days, the majority of progenitors were undergoing gradual proliferation arrest before eventually undergoing apoptosis. During the entire expansion, a measured 4000-fold increase in cell numbers was obtained (Figure 2A, circles; also supplemental Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article).
Conditions for proliferation of human cord blood–derived erythroblasts in serum-free StemSpan medium
Factor . | Concentration . |
|---|---|
| Optimal long-term proliferation | |
| Erythropoietin | 2 U/mL |
| Dex (synthetic glucocorticoid) | 1 μM |
| IGF-1 | 40 ng/mL |
| SCF | 100 ng/mL |
| Cholesterol-rich lipid mix | 40 μg/mL |
| Dihydrotestosterone* | 1 μM |
| Factors without any effect | |
| Interleukin-3 | 1 ng/mL |
| TGF-β | 5 ng/mL |
| Heparin-binding EGF | 20 ng/mL |
| Testosterone† | 1 μM |
| Progesterone | 1 μM |
| Estrogen | 1 μM |
| Cpa (androgen antagonist) | 1 μM |
| Fibronectin-coated plates | 20 ng/mL |
| LY (PI-3-K inhibitor) | 1 μM |
Factor . | Concentration . |
|---|---|
| Optimal long-term proliferation | |
| Erythropoietin | 2 U/mL |
| Dex (synthetic glucocorticoid) | 1 μM |
| IGF-1 | 40 ng/mL |
| SCF | 100 ng/mL |
| Cholesterol-rich lipid mix | 40 μg/mL |
| Dihydrotestosterone* | 1 μM |
| Factors without any effect | |
| Interleukin-3 | 1 ng/mL |
| TGF-β | 5 ng/mL |
| Heparin-binding EGF | 20 ng/mL |
| Testosterone† | 1 μM |
| Progesterone | 1 μM |
| Estrogen | 1 μM |
| Cpa (androgen antagonist) | 1 μM |
| Fibronectin-coated plates | 20 ng/mL |
| LY (PI-3-K inhibitor) | 1 μM |
EGF indicates epidermal growth factor; PI-3-K, phosphoinositol 3-kinase.
Female erythroblasts only.
Male erythroblasts only.
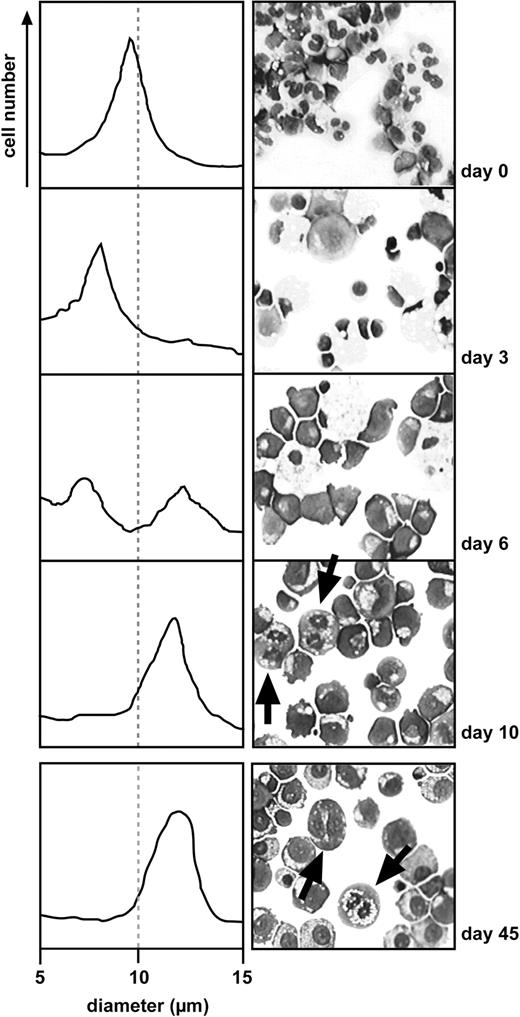
Outgrowth of erythroid progenitors from umbilical cord blood. Left panels show changes in cell size distribution during proliferation of erythroblast cultures for 45 days in optimized medium (Table 1). Cell volume changes were monitored with an electronic cell analyzer. In the right panels, at the times indicated, cells were cytocentrifuged onto glass slides and stained with cytologic dyes. During the first few days, multiple cell types like leukocytes, macrophages, and only few erythroblasts are present, the proportion of which increases on culture in specific erythroid factors (Epo, Dex, murine SCF, and IGF-1). At day 10, the majority of cells in the rapidly proliferating cultures (mitoses indicated by arrows) show an erythroblast morphology. Cells stained with May-Grünwald and Giemsa were visualized using an Axiovert 10 microscope (Zeiss, Oberkochen, Germany) equipped with a 63 × oil-immersion objective (numerical aperture 44-07-61; Zeiss). At 630 × original magnification, images were captured with a Sony 3CCD color video camera (Sony, Tokyo, Japan) and prepared for publication with IP Lab Spectrum P software v.3.1.1 (Signal Analytics, Vienna, VA).
Outgrowth of erythroid progenitors from umbilical cord blood. Left panels show changes in cell size distribution during proliferation of erythroblast cultures for 45 days in optimized medium (Table 1). Cell volume changes were monitored with an electronic cell analyzer. In the right panels, at the times indicated, cells were cytocentrifuged onto glass slides and stained with cytologic dyes. During the first few days, multiple cell types like leukocytes, macrophages, and only few erythroblasts are present, the proportion of which increases on culture in specific erythroid factors (Epo, Dex, murine SCF, and IGF-1). At day 10, the majority of cells in the rapidly proliferating cultures (mitoses indicated by arrows) show an erythroblast morphology. Cells stained with May-Grünwald and Giemsa were visualized using an Axiovert 10 microscope (Zeiss, Oberkochen, Germany) equipped with a 63 × oil-immersion objective (numerical aperture 44-07-61; Zeiss). At 630 × original magnification, images were captured with a Sony 3CCD color video camera (Sony, Tokyo, Japan) and prepared for publication with IP Lab Spectrum P software v.3.1.1 (Signal Analytics, Vienna, VA).
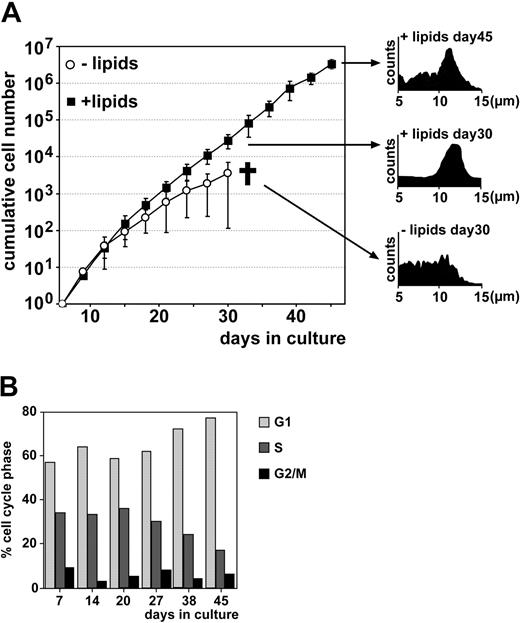
Long-term expansion of human erythroid progenitors. (A) Cell size and proliferation kinetics were determined in the presence (from day 0; = standard medium composition for all other experiments if not stated otherwise) or absence of cholesterol-rich lipids by daily measurements in an electronic cell counter. For clarity, values are shown for every third day only; for the full data set, see supplemental Figure S1. Cumulative cell numbers were calculated as described in “Materials and methods”; error bars indicate SD of mean, n = 5. Cultures without lipid were terminated at day 30 due to excessive cell death (cross symbol). Insets on the right show size distribution of cultures grown with or without lipids; a narrow size range corresponds to healthy cultures. Data are also shown in Table 1. (B) DNA content of cells (+ lipid) was monitored by flow cytometry after DAPI staining and the percentage of cells in particular cell cycle phases determined as described in “Materials and methods.”
Long-term expansion of human erythroid progenitors. (A) Cell size and proliferation kinetics were determined in the presence (from day 0; = standard medium composition for all other experiments if not stated otherwise) or absence of cholesterol-rich lipids by daily measurements in an electronic cell counter. For clarity, values are shown for every third day only; for the full data set, see supplemental Figure S1. Cumulative cell numbers were calculated as described in “Materials and methods”; error bars indicate SD of mean, n = 5. Cultures without lipid were terminated at day 30 due to excessive cell death (cross symbol). Insets on the right show size distribution of cultures grown with or without lipids; a narrow size range corresponds to healthy cultures. Data are also shown in Table 1. (B) DNA content of cells (+ lipid) was monitored by flow cytometry after DAPI staining and the percentage of cells in particular cell cycle phases determined as described in “Materials and methods.”
In experiments to further improve the medium composition (Table 1), lipids (40 μg/mL, cholesterol-rich) reproducibly extended the period of sustained proliferation from 30 to more than 45 days (in 2 experiments up to 60 days), resulting in another 3 logs of cumulative cell number obtained. This corresponds to a total of 3 million-fold cell expansion (Figure 2A, squares). Extrapolating from the data on cell numbers and proliferation rates back to day 0, an apparent overall increase in cell number of 108-fold to more than 109-fold was obtained. This corresponds to 30 to 35 generations, almost approaching the known in vitro lifespan of primary human skin fibroblasts.27 Unless explicitly stated otherwise, all further experiments were performed in medium supplemented with lipid from day 0 on, although no differences in cell phenotype or proliferation were observed on inclusion of lipid at any time between day 0 and 18. Of several additional cytokines and hormones tested for their potential to improve progenitor cell outgrowth, none proved effective (Table 1), with the exception of androgen (see “Androgen enhances proliferation of female but not male human erythroblasts”).
During the last third of the expansion period, the cultures showed a gradual increase of cells in G1 plus a simultaneous decrease in percentage of S-phase cells (Figure 2B; analysis of DNA content by flow cytometry; duration of G2/M nearly unchanged). This effect is somewhat overestimated by the presence of noncycling cells arising through spontaneous differentiation, despite repeated density gradient purification of the immature progenitors.
Long-term expansion of human erythroblasts: continuous requirement for Epo, SCF, and Dex for proliferation and differentiation arrest
To verify that the cultures remained dependent on each of the proliferation factors required for erythroid progenitor expansion and survival during the entire expansion period, cell batches pregrown for 18 days in complete medium were switched to media lacking either single or all factors. The requirement for Epo, SCF, or Dex was then assessed by measuring cell numbers (Figure 3A) and rates of apoptosis by TUNEL assays (Figure 3B; see “Materials and methods”). In our hands, omission of IGF-1 did not decrease proliferation rates within 8 days, consistent with findings in murine erythroblasts.12 Because, however, IGF-1 was previously reported several times to support long-term survival of myeloid progenitors28,29 as well as committed erythroid cells,7,30 the media used in further experiments were nevertheless supplemented with IGF-1.
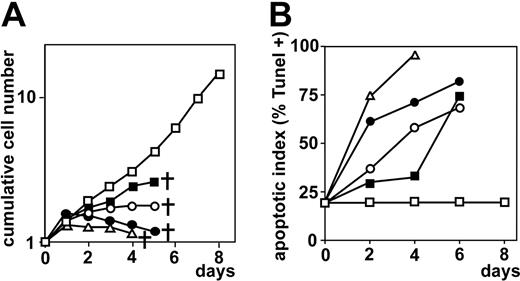
Human erythroid progenitors require Epo, SCF plus Dex for long-term expansion. (A) After precultivation for 18 days (in the absence of lipids), cumulative cell numbers (Figure 2) were determined from cultures kept for 8 more days in either the absence of Epo (▪), or SCF (○), or Dex plus glucocorticoid antagonist ZK (•), or without any factors (▵) by daily counting in an electronic cell counter. Control (□) cultures grown in the presence of all factors. Cross symbol indicates termination of cultures due to excessive cell death. (B) Erythroblasts from cultures in panel A were analyzed for the percentage of apoptotic cells by TUNEL staining and flow cytometry (see “Materials and methods”); symbols are as described for panel A.
Human erythroid progenitors require Epo, SCF plus Dex for long-term expansion. (A) After precultivation for 18 days (in the absence of lipids), cumulative cell numbers (Figure 2) were determined from cultures kept for 8 more days in either the absence of Epo (▪), or SCF (○), or Dex plus glucocorticoid antagonist ZK (•), or without any factors (▵) by daily counting in an electronic cell counter. Control (□) cultures grown in the presence of all factors. Cross symbol indicates termination of cultures due to excessive cell death. (B) Erythroblasts from cultures in panel A were analyzed for the percentage of apoptotic cells by TUNEL staining and flow cytometry (see “Materials and methods”); symbols are as described for panel A.
As expected, erythroblasts exposed to medium without factors stopped proliferating within 24 to 48 hours. After 2 days, more than 75% and after 4 days essentially all cells had died from apoptosis (Figure 3B). Glucocorticoid receptor (GR) signaling was abolished by removal of Dex plus addition of the glucocorticoid antagonist ZK.23 Under these conditions, cells rapidly ceased to proliferate; more than 50% were apoptotic after 2 days, confirming the strict requirement for this hormone for renewal.14 Omitting Dex from the medium alone caused only partial effects, in line with findings in several nuclear receptors, including GR, that antagonist is required to enforce an inactive receptor conformation and releasing receptor-bound ligand.31,32 The glucocorticoid levels present in serum-containing media make it difficult or impossible to observe Dex effects.33,34 However, addition of the ZK antagonist showed that human erythroblasts require Dex also for expansion in serum-containing media.14 In the absence of Epo or SCF, all progenitors disintegrated within 6 days, but proliferation arrest and apoptosis were delayed in the absence of Epo as compared with SCF, similar to previous findings in the chicken and mouse.12,35 Taken together, cultured human erythroblasts remain strictly dependent on Epo, SCF, and Dex throughout their extended period of exponential proliferation.
Cell surface marker expression indicates synchronous, gradual establishment of cells committed to the erythroid lineage
Next, we determined cell-type composition of cord blood–derived cultures during early and later phases of expansion, using surface markers for different lineages and immature progenitors. First, we analyzed markers for immature and mature erythroid cells. High CD117 (c-Kit) expression levels are typical for erythroid progenitors (besides expression on very immature progenitors).9,36 Freshly established cord blood cultures (day 1) exhibited very low CD117 levels, which steadily increased, reached a maximum with almost 100% positive cells around day 14 (Figure 4A), and then gradually declined to 50% CD117high cells at day 35. This suggested that proliferating progenitors gradually increased c-Kit expression from an immature to a more mature erythroid progenitor phenotype, in line with a similar decrease in CD45 (data not shown). This marker for immature cells of most leukocyte lineages is down-regulated during erythroid maturation.37 Gradual maturation of the cultured erythroblasts was also indicated by the continuous increase of CD71high cells (transferrin receptor, up to 100% at day 35; Figure 4A-B). CD71 shows maximal expression in differentiating erythroid cells but disappears on mature erythrocytes. Similarly, GPA, a protein abundant on more mature erythroid cells,38 resembled CD71 in its gradual increase during the whole culture period. These patterns of changes in marker distribution were reproducible for several samples from individual cord blood donors.
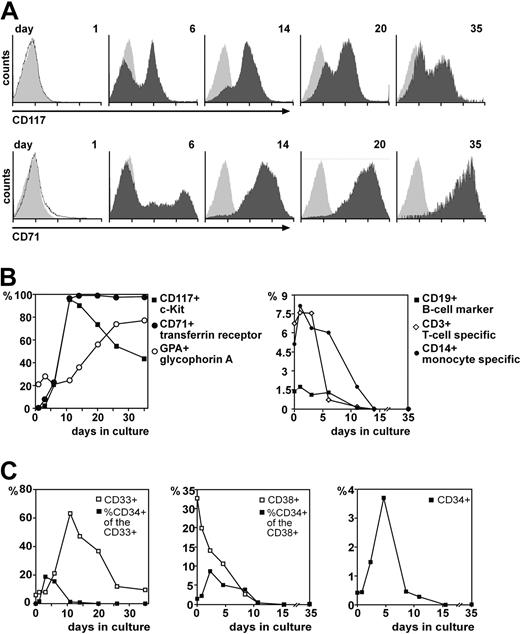
Progression of cell–surface marker expression in developing erythroblast cultures. Aliquots of proliferating cells were harvested at the times indicated, stained with combinations of fluorescently labeled antibodies against markers characteristic for different hematopoietic lineages and stages of development, and subjected to flow cytometry. (A) Histograms showing the changes in CD117 (c-Kit) and CD71 (transferrin receptor) expression over time. Light gray histograms, background fluorescence. (B) Quantitation (as percentage of positive cells) of erythroid (left panel) versus selected nonerythroid marker expression (right panel) during prolonged in vitro cultivation (see also supplemental Table S1). To eliminate nonspecific staining of myeloid cells by the glycophorin antibody, the fraction of cells expressing the erythroid-specific protein glycophorin A (GPA+) is expressed as percentage of transferrin receptor–positive cells. (C) Quantitation of pluripotent (CD34+; gated to be CD45dim) hematopoietic progenitors over time. The fraction of CD34+ cells within the myeloid (CD33+; left panel) and lymphoid compartment (CD38+; middle panel) is shown. Right panel shows total numbers of CD34+ cells for comparison, to depict the overall abundance of immature hematopoietic progenitors during the early phases of erythroblast culture.
Progression of cell–surface marker expression in developing erythroblast cultures. Aliquots of proliferating cells were harvested at the times indicated, stained with combinations of fluorescently labeled antibodies against markers characteristic for different hematopoietic lineages and stages of development, and subjected to flow cytometry. (A) Histograms showing the changes in CD117 (c-Kit) and CD71 (transferrin receptor) expression over time. Light gray histograms, background fluorescence. (B) Quantitation (as percentage of positive cells) of erythroid (left panel) versus selected nonerythroid marker expression (right panel) during prolonged in vitro cultivation (see also supplemental Table S1). To eliminate nonspecific staining of myeloid cells by the glycophorin antibody, the fraction of cells expressing the erythroid-specific protein glycophorin A (GPA+) is expressed as percentage of transferrin receptor–positive cells. (C) Quantitation of pluripotent (CD34+; gated to be CD45dim) hematopoietic progenitors over time. The fraction of CD34+ cells within the myeloid (CD33+; left panel) and lymphoid compartment (CD38+; middle panel) is shown. Right panel shows total numbers of CD34+ cells for comparison, to depict the overall abundance of immature hematopoietic progenitors during the early phases of erythroblast culture.
These data show that the initial population of mononuclear cells isolated from cord blood and used to initiate erythroblast cultures contained very low levels of erythroid progenitors. The most prominent subpopulations of fresh cord blood isolates were mature granulocytes (40%-70%), T lymphocytes (7%-15%), monocytic cells (5%-8%), and other more immature progenitors as seen from corresponding marker analysis (lymphoid cells: CD3, CD4, CD8, CD19; CD45RA; natural killer cells: CD56; granulocytic cells: CD15; monocytes: CD14; CD116). Changes in subpopulation distribution over time suggested that nonerythroid cell types persisted for several days (Figure 4B; data on CD3, CD14, CD19; supplemental Table S1 for other CD antigens mentioned) but did not proliferate under our culture conditions, thus being gradually diluted out by the rapidly proliferating erythroid progenitors.
To determine the abundance of multipotent progenitors in the cord blood cultures, CD33 (myelomonocytic progenitors), CD34 (multipotent progenitors), and CD38 expression (immature lymphoid progenitors) were quantitated in parallel. Starting from low levels (< 0.5%; similar to values reported for freshly prepared cord blood39 ), the percentage of CD34+ cells increased 10-fold up to 4% (Figure 4B) by day 6. In absolute numbers, however, this corresponded to a slight decrease from about 106 to 5 × 105 cells while during the same time the total population of nonerythroid mononuclear cells was declining about 40-fold (from 3 × 108 to 8 × 106 cells). The majority of the CD34+ cells (> 85%) were derived from the myelomonocytic compartment, as indicated by CD33/CD34 double staining. The increase in CD34+ cells peaked around day 6, well preceding the maximum in CD33 expression (> 60% positive cells at day 11) and CD117 (day 14). This argues for persistence of multipotent progenitors during the first 10 to 14 days, which then gradually developed into progenitors of the erythroid lineage.
Androgen enhances proliferation of female but not male human erythroblasts
Due to their predominantly sex-specific actions, the potential of sex steroids to modulate human hematopoietic development in vitro has not been addressed so far. However, disturbances in sex steroids contribute to a number of diseases such as anemia.40 In the chicken, estrogen and GR ligands (Dex) both contribute to long-term self-renewal of erythroid progenitors41,42 and, consequently, interfere with terminal maturation.43
These observations prompted us to expand human erythroblasts in the presence of various other hormones besides Dex. Whereas estrogen and progesterone had no effects (Table 1), dihydrotestosterone (an androgen) significantly enhanced the proliferation rate of cells from certain cord blood donors but not from others. One way to interpret this puzzling behavior was that androgen might act in a sex-specific manner. Thus, erythroid progenitors from cord blood of male and female newborns were expanded in the presence or absence of dihydrotestosterone. As a control, the androgen antagonist cyproterone acetate (Cpa)44 was included (Figure 5 and supplemental Figure S2).
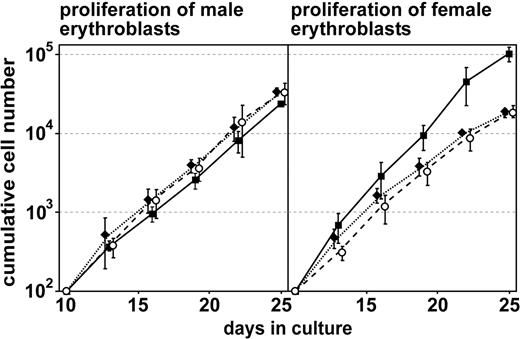
Proliferation of male versus female human erythroblasts on addition of androgen. Cell numbers from cultures of male versus female cord blood donors (pregrown for 8 days in the absence of sex steroids) were counted daily in an electronic cell counter, and cumulative cell numbers determined (Figure 2; see “Materials and methods”). For clarity, values are shown for every third day only; for the full data set, see supplemental Figure S2. Cells were cultivated either under standard proliferation conditions (control, ♦), or in the presence of 1 μM testosterone (▪) or testosterone plus the androgen antagonist cpa (1 μM; ○). Error bars are SD of mean; n = 3.
Proliferation of male versus female human erythroblasts on addition of androgen. Cell numbers from cultures of male versus female cord blood donors (pregrown for 8 days in the absence of sex steroids) were counted daily in an electronic cell counter, and cumulative cell numbers determined (Figure 2; see “Materials and methods”). For clarity, values are shown for every third day only; for the full data set, see supplemental Figure S2. Cells were cultivated either under standard proliferation conditions (control, ♦), or in the presence of 1 μM testosterone (▪) or testosterone plus the androgen antagonist cpa (1 μM; ○). Error bars are SD of mean; n = 3.
Dihydrotestosterone had no effect on the proliferation of “male” cells over 25 days of culture. However, for “female” erythroblasts a significant and reproducible enhancement in proliferation was observed with dihydrotestosterone. The antagonist Cpa reduced the testosterone-induced increased proliferation of female cultures back to the level of untreated controls but not below, whereas again it had no effect on male cultures (Figure 5). This indicates that the androgen effect was specific and argues against unspecific cross talk between different steroid hormone–dependent signaling pathways.
Induction of synchronous terminal differentiation
Most established erythroid cell lines to study terminal erythroid differentiation suffer from drawbacks such as nonphysiologic stimuli required to initiate maturation, asynchronous progress into differentiation, low levels of hemoglobin synthesized, and a failure to enucleate. Recently, we established conditions for efficient terminal maturation of primary and permanently proliferating (p53-deficient) mouse erythroblasts2,3 by removing proliferation factors (Epo, SCF, Dex) and exposing the cells to differentiation conditions (Epohigh, Ins, iron-saturated transferrin, ZK). Initially, we tried to adapt these protocols to terminally differentiate homogeneous cell populations of cultured human erythroid progenitors pre-expanded for 14 days. Differentiation media consisted of serum-free medium (StemSpan) used for expansion plus factors/hormones to be tested (Table 2).
Standard conditions allowing efficient terminal differentiation of human erythroblasts in serum-free StemSpan medium
Factor . | Concentration . |
|---|---|
| Efficient terminal differentiation | |
| Erythropoietin | 10 U/mL |
| Insulin | 4 × 10-4 IE/mL |
| Human transferrin (iron saturated) | 1 mg/mL |
| ZK-112993 (glucocorticoid antagonist) | 3 μM |
| T3 | 1 μM |
| Human serum (commercial; Sigma) | 3% |
| Factors without any effect | |
| Cholesterol-rich lipid mix (Sigma) | 20-100 μg/mL |
| TGF-β | 1-25 pg |
| Activin | 1-25 pg |
| Fetal chicken serum | 10% |
| Chicken serum | 5%-10% |
| Human anemic serum | 2%-10% |
| Human cord blood serum | 2%-10% |
| Dihydrotestosterone | 1 μM |
| Progesterone | 1 μM |
| Estrogen | 1 μM |
| LY (PI-3-K inhibitor) | 1 μM |
| Fibronectin-coated plates | 20 μg/mL |
| Cpa (androgen antagonist) | 1 μM |
Factor . | Concentration . |
|---|---|
| Efficient terminal differentiation | |
| Erythropoietin | 10 U/mL |
| Insulin | 4 × 10-4 IE/mL |
| Human transferrin (iron saturated) | 1 mg/mL |
| ZK-112993 (glucocorticoid antagonist) | 3 μM |
| T3 | 1 μM |
| Human serum (commercial; Sigma) | 3% |
| Factors without any effect | |
| Cholesterol-rich lipid mix (Sigma) | 20-100 μg/mL |
| TGF-β | 1-25 pg |
| Activin | 1-25 pg |
| Fetal chicken serum | 10% |
| Chicken serum | 5%-10% |
| Human anemic serum | 2%-10% |
| Human cord blood serum | 2%-10% |
| Dihydrotestosterone | 1 μM |
| Progesterone | 1 μM |
| Estrogen | 1 μM |
| LY (PI-3-K inhibitor) | 1 μM |
| Fibronectin-coated plates | 20 μg/mL |
| Cpa (androgen antagonist) | 1 μM |
To follow the progress of terminal maturation, proliferation rate, volume decrease (measured in a cell analyzer), and hemoglobin accumulation (quantitative photometric assay; see Kowenz et al25 and “Materials and methods”) were monitored daily. In addition, cytocentrifugation followed by histologic staining was applied for phenotypic characterization, again to assess hemoglobinization but also to detect enucleated erythrocytes at the end of maturation. Differentiation with the factor mix used for mouse cells did not yield satisfying results. Rather than differentiating, the cells underwent apoptosis at high frequency and accumulated little hemoglobin (Figure 6A-E). Systematic variation of multiple differentiation medium components to improve terminal maturation of immature progenitors was ineffective (Table 2). In contrast, addition of normal human serum combined with Epohigh/Ins was found to strongly improve synchronous differentiation.
Terminal differentiation of human erythroid progenitors. Proliferation kinetics (A) and volume decrease (B) during differentiation in the presence or absence of 3% human serum (HS) was monitored daily by an electronic cell counter. (C) Quantitation of hemoglobin accumulation (for photometric assay, see Kowenz et al25 and “Materials and methods”); 500 AU corresponds to 11.0 pg hemoglobin. Error bars in panels A-C represent the SD of mean, n = 5. (D) Cells before (left) and after differentiation for 6 days in the absence (middle panel) or presence of HS (right panel) were cytocentrifuged onto slides and stained with neutral benzidine (to detect hemoglobin; brownish stain) plus histologic dyes (see “Materials and methods”). Image acquisition was performed as described for Figure 1. (E) Kinetics of changes in cell size distribution during differentiation of human erythroblasts without serum (upper panel) and with HS (lower panel). (F) Expression of erythroid cell-surface markers in proliferating and differentiating erythroblasts (left panel, labeled “control”: differentiation without serum; right panel, differentiation in the presence of 3% HS). Proliferating cells or erythroblasts induced to differentiate for 6 days were washed with PBS/1% FCS, stained with fluorescently labeled antibodies against c-Kit (CD117), transferrin receptor (CD71), and glycophorin A (GPA) and subjected to fluorescence-activated cell sorting (FACS) analysis. Orange graphs are FACS profiles of self-renewing erythroblasts; red graphs are cell-surface antigen expression in differentiating cells; light gray histograms indicate background fluorescence.
Terminal differentiation of human erythroid progenitors. Proliferation kinetics (A) and volume decrease (B) during differentiation in the presence or absence of 3% human serum (HS) was monitored daily by an electronic cell counter. (C) Quantitation of hemoglobin accumulation (for photometric assay, see Kowenz et al25 and “Materials and methods”); 500 AU corresponds to 11.0 pg hemoglobin. Error bars in panels A-C represent the SD of mean, n = 5. (D) Cells before (left) and after differentiation for 6 days in the absence (middle panel) or presence of HS (right panel) were cytocentrifuged onto slides and stained with neutral benzidine (to detect hemoglobin; brownish stain) plus histologic dyes (see “Materials and methods”). Image acquisition was performed as described for Figure 1. (E) Kinetics of changes in cell size distribution during differentiation of human erythroblasts without serum (upper panel) and with HS (lower panel). (F) Expression of erythroid cell-surface markers in proliferating and differentiating erythroblasts (left panel, labeled “control”: differentiation without serum; right panel, differentiation in the presence of 3% HS). Proliferating cells or erythroblasts induced to differentiate for 6 days were washed with PBS/1% FCS, stained with fluorescently labeled antibodies against c-Kit (CD117), transferrin receptor (CD71), and glycophorin A (GPA) and subjected to fluorescence-activated cell sorting (FACS) analysis. Orange graphs are FACS profiles of self-renewing erythroblasts; red graphs are cell-surface antigen expression in differentiating cells; light gray histograms indicate background fluorescence.
Like chicken and mouse erythroblasts,3,45 human erythroid progenitors continued to divide on differentiation initiation but only for 1 to 2 divisions, compared with 4 to 5 in chickens and 3 to 4 in mice (Figure 6A). Accompanying these “differentiation divisions,” cell size decreased from about 660 to 380 fL. Hemoglobin accumulation started from very low levels (Figure 6C,E), confirming the low rate of spontaneous differentiation in the renewing cells, and steadily increased more than 10-fold within 6 days. Hemoglobin levels reached about 35% (11.5 ± 1.0 pg; n = 5) of the value determined for peripheral human erythrocytes (31.6 ± 2.4 pg; n = 5). Although cells “differentiated” in the absence of human serum had a stronger size decrease (Figure 6B), this was due to massive cell death as indicated by broad size distribution, the extensive presence of cell debris, and the lack of hemoglobin (Figure 6C-E). Cytospins after 6 days of differentiation plus serum exhibited morphologic changes and staining for hemoglobin consistent with successful maturation (Figure 6E). The differentiation-promoting effect of serum was further confirmed by cultivating erythroblasts under standard proliferation conditions plus 3% serum, indeed observing reduced proliferation and enhanced spontaneous differentiation (Figure S3). Finally, due to the sex-specific proliferation effect, the influence of testosterone on differentiation of female versus male erythroid progenitors was tested: no effects were observed (data not shown).
Terminal erythropoiesis was also assessed on the basis of the cell surface markers c-Kit (CD117; characteristic for proliferating erythroid progenitors), transferrin receptor (CD71), and GPA (both markers for mature cells). As expected, erythroblasts differentiating in the presence of serum showed a down-regulation of c-Kit to background levels and a further induction of GPA (from 70% to 100% positive cells; Figure 6F). CD71 expression at the cell surface was slightly down-regulated, agreeing with our earlier data showing a partial redistribution of CD71 to intracellular compartments in differentiating avian and murine cells46 ; Lioba Lobmayr and E.W.M., unpublished observations, 2002). Whereas regulation of CD71 and GPA was similar in cells differentiating in the presence or absence of serum, c-Kit levels did not decrease when serum was absent (Figure 6F, top left panel). This was in striking contrast to data from murine erythroblasts, where removal of SCF plus Dex is sufficient to induce loss of c-Kit and terminal differentiation, provided the cells are protected from apoptosis.3 This indicates that human erythroid progenitors require human serum factors for terminal differentiation, which is not required in mouse cells, pointing to an apparent difference between murine and human erythropoiesis.
T3 improves terminal maturation of human erythroblasts
One possibility to explain the serum effects could be that human and murine erythroid cells differ in their responsiveness to T3. Because lack of T3 in humans is associated with anemia47,48 and its addition strongly accelerates terminal differentiation of chicken erythroblasts,13,49 we analyzed the effect of T3 on human erythroid differentiation, together with several other hormones (Table 2).
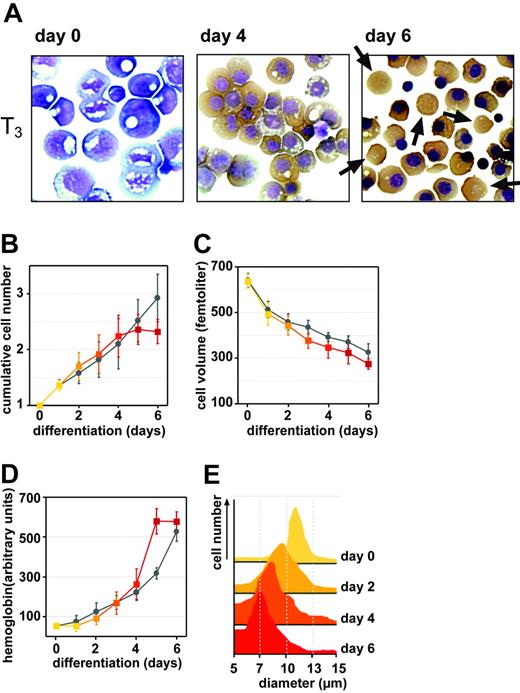
T3 further accelerated the rate of hemoglobin accumulation and the abundance of enucleated cells, which by morphologic criteria were indistinguishable from mature erythrocytes (Figure 7). Overall hemoglobin values in these populations (differentiated for 6 days) reached about 40% (12.9 ± 1.1 pg; n = 5) of the level in circulating human erythrocytes, an underestimate due to the fraction of nonenucleated cells (Figure 7A; cells with condensed, acentric nuclei, smaller than original blasts). Improved synchrony of maturation by T3 was also evident from the much narrower size distribution at each time point (Figure 7E; compare with Figure 6D). No major differences in expression of c-Kit, GPA, and CD71 were detected by cytofluorometry in cells differentiating in the presence or absence of T3.
Improved differentiation of human erythroblasts in the presence of T3.Human erythroblasts were induced to differentiate either in the presence or absence of T3 (1 μM). (A) Cells were analyzed by cytocentrifugation plus histochemical staining (Figure 6). Enucleated cells observed at day 6 of differentiation in the presence of T3 are indicated by arrows. Image acquisition was performed as described for Figure 1. Proliferation rates (B) and volume decrease (C) during differentiation were determined daily (Figure 6) using an electronic cell counter. (D) Quantitation of hemoglobin accumulation (see “Materials and methods”; 500 AU corresponds to 11.0 pg hemoglobin). Error bars in panels B-D represent the SD of mean, n = 5. (E) Changes in cell size distribution during differentiation plus T3 (compare with Figure 6D).
Improved differentiation of human erythroblasts in the presence of T3.Human erythroblasts were induced to differentiate either in the presence or absence of T3 (1 μM). (A) Cells were analyzed by cytocentrifugation plus histochemical staining (Figure 6). Enucleated cells observed at day 6 of differentiation in the presence of T3 are indicated by arrows. Image acquisition was performed as described for Figure 1. Proliferation rates (B) and volume decrease (C) during differentiation were determined daily (Figure 6) using an electronic cell counter. (D) Quantitation of hemoglobin accumulation (see “Materials and methods”; 500 AU corresponds to 11.0 pg hemoglobin). Error bars in panels B-D represent the SD of mean, n = 5. (E) Changes in cell size distribution during differentiation plus T3 (compare with Figure 6D).
As for serum, this T3 effect raised the question whether the hormone would shift the balance between proliferation and differentiation, as previously observed in chicken erythroblasts.49 Indeed, addition of T3 under proliferation conditions increased the proportion of spontaneous differentiation, as judged from reduced proliferation rates, gradual decrease of cell size, and detectable amounts of hemoglobin synthesized (supplemental Figure S4).
Discussion
The expansion of hematopoietic progenitors from umbilical cord blood or peripheral blood ex vivo is of great interest, both for basic research and the exploitation of clinical potential. Here we demonstrate, at least for the erythroid compartment, that steroid hormones play a larger than anticipated role in regulating the balance between sustained proliferation and terminal differentiation. Previously used procedures failed to yield long-term proliferating but immature erythroid progenitors, due to massive spontaneous differentiation.15,33,34 The use of serum-containing media limited the expansion of erythroid progenitors even when Epo, SCF, and glucocorticoid were provided.14 Using serum-free media together with Epo, SCF, glucocorticoid, and androgen, we could expand human erythroid progenitors from umbilical cord blood for about 7 weeks. This yielded mass populations with an in vitro lifespan of approximately 30 generations, almost absent spontaneous differentiation and essentially no hemoglobinization, largely facilitating future biochemical and molecular characterization. Optimization of differentiation conditions allowed induction of synchronous terminal maturation, resulting in enucleated cells virtually indistinguishable from erythrocytes of peripheral blood.
The role of glucocorticoids in enhancing proliferation and blocking differentiation of erythroid progenitors becomes increasingly recognized in vitro and in vivo. Glucocorticoids regulate multiple physiologic and developmental processes by binding to and modulating the transcriptional activity of their cognate nuclear receptor (GR).50-52 In both chicken and mouse erythroblasts, ligand-activated GR cooperates with activated EpoR and c-Kit, the SCF receptor, to retain erythroid cells in an immature state and thus to induce long-term proliferation.12,42,53,54 A similar effect of glucocorticoids was described in human erythroblasts,14 but their expansion was limited to 15 to 22 cell divisions, probably due to the use of serum-containing media. Importantly, GR is also required for stress erythropoiesis following hypoxia or blood loss in the mouse.10
In our hands, the serum-free medium (StemSpan) used here was critical for generating long-term cultures. Other serum-free media proved less efficient, the specific type of human serum albumin contained in this medium being one likely candidate. The inclusion of even small amounts of serum (human, calf) strongly increased the rate of spontaneous differentiation.34,55 Given our results on the differentiation-promoting effects of thyroid hormone and numerous reports on similar effects of transforming growth factor β (TGF-β),56-58 it may well be that the absence of these serum components from the synthetic StemSpan medium was critical for achieving long-term proliferation of erythroid progenitors. Compared with other current procedures, it should also be noted that our conditions did not require positive preselection for immature, pluripotent progenitors (eg, CD34+/c-Kit–),55,59 negative selection (depletion) against lymphoid or granulocytic cells nor highly complex mixtures of multiple cytokines.60 Importantly, the use of serum-free medium yielded immature erythroid progenitors with an in vitro lifespan approaching the “Hayflick Limit” of human fibroblasts (40-50 generations). Routinely, a (calculated) 108-fold expansion was obtained, in some experiments even a 1010-fold increase in cell numbers (about 35 generations). Thus, the procedure described here enables the production of large numbers of homogeneous primary human cells for detailed molecular characterization of mechanisms underlying progenitor renewal versus differentiation, including expression profiling.
The clear-cut effect of glucocorticoids, together with the renewal-enhancing role of estrogens on chicken erythroblasts,42,43 prompted us to evaluate the effects of additional (steroid) hormones on expansion/maturation of human erythroid progenitors. Whereas estradiol or progesterone were ineffective, androgen clearly promoted proliferation of cord blood erythroid cells from female but not from male donors. This sex-specific effect of androgens could be completely blocked by the androgen-antagonist, Cpa, demonstrating specificity.
The recent literature on androgen and hematopoietic cells is scarce. Whereas androgen ablation reduced the number of peripheral B cells in male mice,61 the hormone or an anabolic derivative thereof increased the number of red cells and erythroid colony-forming units (CFU-Es) in rats and mice, respectively.62,63 There is some biochemical evidence for the expression of androgen receptor (AR) in erythroblasts from human bone marrow cultures64 and megakaryocytes.65 Given the major role of GR in these cells, one might speculate about a cross-talk between AR and GR, similar to the cross-talk described between estrogen receptor (ER) and progesterone receptor (PR)66 or TGF-α receptor (c-ErbB).41 Similar to inhibition of the PR-ER cross-talk with estrogen antagonists, liver GR activity could be inhibited with Cpa.67 At present, we cannot explain the sex specificity of proliferation enhancement by androgen. No differences in GR potency/expression levels between males and females have been reported. Also, promiscuity for the corresponding hormone response elements is unlikely, because despite sequence similarities they are clearly distinguished by GR versus AR.68 Moreover, so far we failed to detect AR protein or mRNA in human erythroblasts. Thus, androgen might exert its effects via binding to other hormone-receptor family members69 or nonclassical pathways in the absence ofAR via androgen-binding proteins. The latter can stimulate second messenger cascades like the Src/mitogen-activated protein kinase (Src/MAPK) and cyclic adenosine monophosphate–protein kinaseA(cAMP/PKA) pathways, or might increase intracellular calcium levels,70 for example, via G protein-coupled receptors.
Clinically, effects of androgen administration on red cell numbers as evidenced by hematocrit levels are well documented, for example, for hypogonadal men,71 patients treated for prostate hyperplasia,72 men undergoing hemodialysis,73 as well as in athletes on doping with androgens.74 In addition, women receiving dihydrotestosterone therapy also show higher hematocrit values,75,76 which was already noted decades ago in patients with breast cancer who received androgen for therapeutic reasons.77,78 To our knowledge, however, there were so far no data on female-restricted proliferation-promoting effects of androgen in erythroid cells in vitro, which should facilitate molecular evaluation of the pathways involved.
Also the direct differentiation-promoting effect of thyroid hormones (in particular T3) on human erythroid progenitors merits further mechanistic exploration. Although thyroids are required for normal development, differentiation and metabolism of many cell types,79,80 little is known about their role in normal erythropoiesis. In mice lacking TRα, TRβ, or both, standard hematopoiesis appears unaffected.81-83 Primary chicken erythroblasts overexpressing TRα variants (gag-c-ErbA) in the absence of T3 underwent sustained proliferation in cooperation with liganded c-Kit.13 In contrast, T3 accelerated differentiation of normal avian erythroid progenitors and even promoted differentiation under proliferation conditions.49,84 Thus, in this avian model, TRα appeared as a ligand-operated “switch,” modulating the balance between renewal and differentiation.13 So far we could not reproduce these results in the mouse (H.B., unpublished observations, 2003). It was thus interesting to find clear evidence for a function of T3 in human erythroid progenitor maturation, operating efficiently at the endogenous TR without requiring overexpression.
Our data show profound effects of steroids and thyroid hormones on renewal, proliferation, and differentiation of long-term proliferating, immature human erythroid progenitors, leading to several additional considerations. On the medical side, it may be worthwhile to re-evaluate and eventually adjust the hormone status in some forms of (mild) anemia, for example, in postmenopausal women, which although not life-threatening reduce the quality of life. The protocol for cell expansion reported here can also be applied to cells from peripheral blood. In preliminary tests, we not only expanded erythroid progenitors but also cells of other hematopoietic lineages in factor combinations used for multipotent progenitors (C.L. and Daniel Genz; manuscript in preparation). With respect to molecular mechanisms, our cells are ideal for expression-profiling approaches, aimed at identifying target genes specifically modulated in their expression by the hormones used in this study.
Taken together, the advances in long-term expansion of hematopoietic (erythroid) cells described here can facilitate extensive biochemical analyses of cells from patients with hereditary hematopoietic disorders (eg, thalassemias), which were technically demanding so far due to lack of material. Our system will also be ideal to address novel pathways modulating the balance between renewal and erythroid maturation in vitro.
Prepublished online as Blood First Edition Paper, September 9, 2004; DOI 10.1182/blood-2004-03-1002.
Supported by the Austrian Science Foundation (“Fonds zur Förderung der wissenschaftlichen Forschung” [FWF]; H.B. and E.W.M.) and the Herzfelder-Family Foundation (E.W.M.).
C.L. and F.B. contributed equally to the work.
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank G. Fritsch, D. Prinz (Children's Cancer Research Institute, Vienna) and P. Steinlein (Research Institute of Molecular Pathology, Vienna, Austria) for their initial introduction to flow cytometry of human cells as well as T. Sauer (Institute of Molecular Biology, Jena, Germany) for excellent technical assistance.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal