Comment on Hanash and Levy, page 1828
BMT is potentially a cure for hematopoietic disorders; however, the beneficial effects are accompanied by the presence of GVHD. Hanash and Levy have proposed an innovative approach of injection of CD4+CD25+ T cells to prevent GVHD and facilitate donor engraftment while maintaining immune competence.
Graft-versus-host disease (GVHD) remains the main complication after bone marrow transplantation. While T-cell depletion of the graft can eliminate GVHD, this results in poor engraftment and increased incidence of leukemia relapse. An alternative strategy is the functional inactivation of T cells with the use of immunosuppressive drugs. However, this strategy leads as well to an increased risk of tumor relapse. Exploiting regulatory mechanisms within the immune system might provide a new tool to control GVHD.
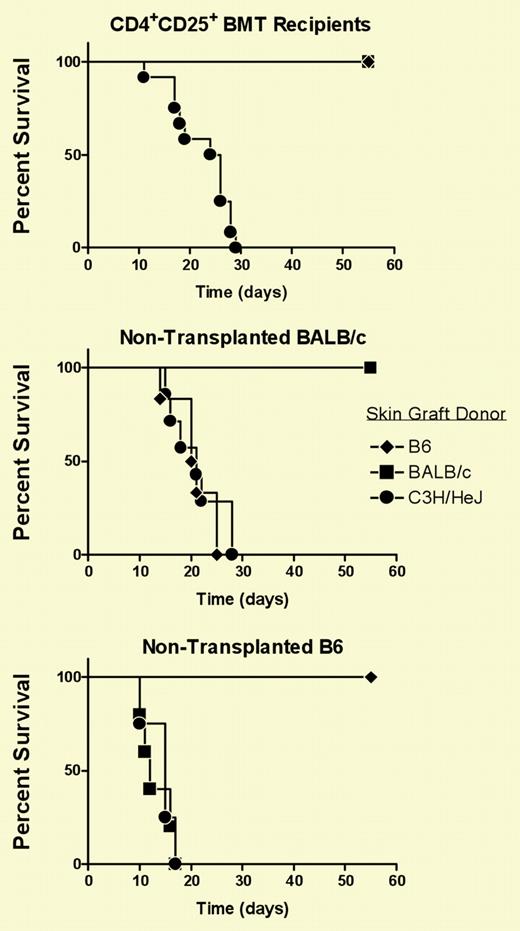
In this issue of Blood, Hanash and Levy report the use of CD4+CD25+ T cells as an alternative to unfractionated T cells in a murine fully major histocompatibility complex (MHC)–mismatched bone marrow transplantation (BMT) model. The results obtained in this paper suggest that CD4+CD25+ T cells facilitate donor engraftment in the absence of GVHD. These events were associated with tolerance induction to both donor and recipient antigens but not to third-party antigens (see figure).
CD4+CD25+ T cells are essential for the induction and maintenance of tolerance to self-antigen and for the prevention of autoimmune disease. Sakaguchi et al found that the development of autoimmune disease in nude mice could be prevented by the transfer of CD4+CD25+ T cells. Their role is not limited to the regulation of responses to autoantigens, in that CD4+CD25+ T cells have also been shown to mediate transplantation tolerance in murine models of skin and solid organ transplantation. In addition, donor CD4+CD25+ T cells have been previously shown to efficiently inhibit rapid lethal GVHD when they are infused following BMT.1-3 In these reports, freshly isolated or ex vivo–expanded CD4+CD25+ T cells were injected at the same time as freshly purified CD4+ T cells. Other reports have investigated the ability of CD4+CD25+ T cells to regulate the graft-versus-tumor (GVT) response. The results obtained have shown that while the inhibitory effect of CD4+CD25+ T cells on GVHD is maintained, the ability of T cells to eradicate established tumors was not impaired.4 The novel feature of the study by Hanash and Levy is to demonstrate that transplantation of CD4+CD25+ T cells in the absence of any other CD4+ T cells is an effective strategy.FIG1
Recipients who received transplants of BM and CD4+CD25+ T cells acutely reject third-party skin grafts. See the complete figure in the article beginning on page 1828.
Recipients who received transplants of BM and CD4+CD25+ T cells acutely reject third-party skin grafts. See the complete figure in the article beginning on page 1828.
The question of specificity of CD4+CD25+ T cells is still a matter of debate. The relevance of this point when using CD4+CD25+ T cells in the context of BMT is to be able to maintain an efficient GVT response while GVHD is impaired. Recently, CD4+CD25+ T cells activated in vitro with allogeneic antigen-presenting cells have been shown to mediate antigen-specific T-cell tolerance in BMT.5 In the study by Hanash and Levy, the question as to whether tolerance to GVHD can be separated from the maintenance of GVT has not been addressed. They have demonstrated that the mice are immune competent both in vitro and in vivo; however, the capacity of these mice to eliminate tumors needs to be evaluated.
In a clinical setting, it would be impossible to obtain enough freshly isolated CD4+CD25+ T cells to be transplanted. Antigen-specific human CD4+CD25+ T cells have been successfully expanded in vitro and have been shown to maintain their suppressor phenotype (Shuiping Jiang and Robert I. Lechler, unpublished data, 2004). The next step requires regulatory T cells to be tested in a clinical trial to prevent GVHD and facilitate donor engraftment without interfering with the beneficial GVT effect. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal