Abstract
Epstein-Barr virus (EBV)–specific immunologic memory is not transferred from mother to child. In vitro infection of cord blood cells can therefore readily lead to the outgrowth of transformed B lymphocytes. We found that the immunomodulator polysaccharide K (PSK) or the mitogenic cytokine truncated thioredoxin (Trx80) inhibited the EBV-induced B-cell proliferation. Using signaling lymphocytic activation molecule (SLAM)–associated protein (SAP) induction as a sign for T- and natural killer (NK) cell activation, we could follow it without any need for cell separation because neither macrophages nor B lymphocytes express SAP. The results suggest the following scenario: EBV infected and activated B lymphocytes. Upon interacting with these cells, T cells became posed for responding to cytokines produced by monocytes. Both PSK and Trx80, which is a secreted C-terminally truncated thioredoxin, activated the monocytes, which then produced cytokines in the presence of the primed T cells. PSK induced interleukin-15 (IL-15), while Trx80 induced IL-12 production. Both cytokines activated the T cells for function. Phosphatidylinositol 3–(PI 3)–kinase and reactive oxygen species (ROSs) were involved in the PSK-induced activation of monocytes. Restimulation of the cultures with EBV-transformed B cells generated specific cytotoxic activity.
Introduction
Epstein-Barr virus (EBV) is ubiquitous in the human population.1 More than 90% of the individuals are virus carriers. The virus persists in spite of EBV-specific humoral and cellular immunity, directed against viral components and against virus-induced cellular proteins.2-4
The outcome of the first encounter with the virus is highly variable. It can occur unnoticed, but if infection is delayed until adolescence it causes the infectious mononucleosis (IM) syndrome in about half of the cases. The IM syndrome is complex, with wide variation in severity, but it is always self-limiting. The decisive mechanism that arrests EBV-induced B-cell proliferation is attributed to both innate and EBV-specific cellular immunity.
EBV-specific immunity is not transferred from mother to child. Therefore, cord blood mononuclear cells (CBMCs) are well suited for analysis of cellular interactions in primary infection. Earlier reports showed induction of both natural killer (NK) and CD4 T-cell–mediated cytotoxic activities5,6 and interleukin-2 (IL-2)–producing CD4 T cells7 responding to EBV-infected B lymphocytes in cord blood cultures.
We have studied previously the events following EBV infection of CBMCs in vitro. We decided to use the immunomodulator polysaccharide K (PSK), based on our earlier results in mixed lymphocyte-tumor cell culture in which it potentiated the cell-mediated response.8 PSK is a protein-bound polysaccharide, extracted from the mycelium of Coriolus versicolor. PSK has been used as a immunostimulant for treating cancer patients in Japan for more than 20 years.9 Its antitumor activity has been documented in experimental animal models, and beneficial therapeutic effects have been shown in the clinical studies.9 We reported earlier that in CBMC cultures, the T cells were activated and the outgrowth of EBV-transformed B cells was inhibited if PSK was added. The EBV-infected cultures contained mainly CD4 T cells that acquired cytotoxic function upon restimulation with autologous EBV-transformed B cells.10
The present work was directed to the analysis of the PSK-induced effects in the EBV-infected CBMC cultures. We assumed that the T cells were activated by encounter with the EBV-infected B lymphocytes, and subsequently they responded to PSK or to factors induced by PSK. We show here that the monocytes became activated by PSK and produced cytokines that acted on T and NK cells.11,12
Truncated thioredoxin (Trx80), a 10-kDa form of thioredoxin secreted from cells and present in plasma, has been shown to stimulate a T helper 1 (Th1) response in human peripheral blood mononuclear cell (PBMC) cultures through induction of IL-12 production in monocytes.13-15 Based on these earlier findings, we have added Trx80 to the EBV-infected CBMC cultures.
We found that T cells were activated in the presence of Trx80, and the EBV-induced B-cell growth was inhibited. Similarly to the effect of PSK, the Trx80-induced growth inhibition was also initiated by the activation of monocytes, which then produced cytokines. In both cases, the cytokine production required the presence of activated T cells. While the details of the early events leading to inhibition of the EBV-induced B-cell transformation were similar, PSK and Trx80 differed in that PSK induced IL-15 while Trx80 induced IL-12.
Materials and methods
Reagents and Abs
Ficoll-paque was purchased from Pharmacia Biotec (Uppsala, Sweden); and PSK, from Kureha Chemical (Tokyo). Recombinant human Trx80 was prepared and purified as described previously.15 Interferon γ (IFN-γ) was purchased from R&D System (Minneapolis, MN); IL-2, from Ajinomoto (Tokyo); monensin, from Sigma-Aldrich (St Louis, MO); phosphatidylinositol 3 (PI 3)–kinase–specific inhibitor LY294002, from Cell Signaling (Beverly, MA); the antioxidant N-acetyl-l-cysteine (NAC), from Sigma-Aldrich; reactive oxygen species (ROS) prober dye 2′,7′-dichlorofluorescin diacetate (H2DCFDA), from Molecular Probes (Eugene, OR); anti-CD19 antibody (Ab)–conjugated beads (Dynabeads M-450), from Dynal (Oslo, Norway); 3H-thymidine, from Amersham Pharmacia Biotech (Uppsala, Sweden); and purified mouse human and anti–human IL-12 (p40/p70) monoclonal antibody (mAb, C8.6) used for neutralization of human IL-12, from BD PharMingen (San Diego, CA). Monoclonal antibody to human IL-15 (146B7), used for neutralization of human IL-15, was a kind gift from GenMab (Copenhagen, Denmark). Mouse monoclonal fluorescein isothiocyanate (FITC)–conjugated anti-CD3, anti-CD19, phycoerythrin (PE)–conjugated anti-CD4, anti-CD8, and anti-CD14 rabbit antimouse FITC-conjugated antibodies for flow cytometry were purchased from Dako (Glostrup, Denmark); PE–cyanin 5 (Cy5)–conjugated anti-CD56, from BD PharMingen; IL-15 and IL-12 enzyme-linked immunosorbent assay (ELISA) antibodies, from R&D System; and the mAb anti–HLA class I (mAb W6/32) or II (mAb CR3/43), from Dako. Affinity-purified rabbit anti–signaling lymphocytic activation molecule (SLAM)–associated protein (SAP) antiserum was a kind gift from Dr J. Sümegi, Cincinnati Medical Center (Cincinnati, OH). Horseradish peroxidase (HRP)–conjugated donkey anti–rabbit immunoglobulin (Ig) antibody, enhanced chemiluminescence (ECL) + Plus detection reagent, and Hyperfilm-ECL film were purchased from Amersham (Arlington Heights, IL).
Preparation and culture of cells
Cord blood samples were obtained from Karolinska University Hospital. The study was approved by the Ethics Committee of the Karolinska Institutet and the Karolinska Hospital. Informed consent was provided according to the Declaration of Helsinki.
Mononuclear cells were isolated from heparinized cord blood by Ficoll-paque density centrifugation. For isolation of B cells, cord blood mononuclear cells (CBMCs) were incubated with anti-CD19 Ab-conjugated beads. The attached cells were recovered from the beads using DETACHaBEADs (Dynal). The cells were cultured at a density of 106/mL in RPMI 1640 supplemented with 10% fetal calf serum (FCS), 100 U/mL penicillin, and 100 μg/mL streptomycin at 37°C, 5% CO2.
EBV infection
CBMCs or separated B cells were exposed to B95-8 virus containing supernatant for 1.5 hours in a humidified 37°C, 5% CO2 incubator. The cells were washed and resuspended in complete RPMI at 1 × 106/mL concentration.
Monocyte isolation on gelatin- and plasma-coated dishes
Monocytes were isolated as described earlier with minor modifications.16 Cell culture dishes (6 cm Φ) with 2% gelatin were kept for 2 hours at 37°C. Then the gelatin solution was removed and the dishes were dried. Before the cell suspension was added, the dishes were incubated with autologous plasma for 1 hour at 37°C followed by 2 rinses with phosphate-buffered saline (PBS). CBMCs (1 × 107) were seeded in each dish and incubated for 40 minutes at 37°C. The floating cells were collected and the dishes were rinsed 3 times with prewarmed medium. The adherent monocytes were collected after 5 mM EDTA (ethylenediaminetetraacetic acid) treatment, centrifuged, and washed twice with PBS; according to the analysis by flow cytometry, the proportion of CD14+ monocytes was more than 85%.
Outgrowth inhibition of EBV-infected B cells
Outgrowth inhibition of EBV-infected B cells was assayed on day 12 of culture. The efficiency of the inhibition is known to depend on the cell density in the cultures.17 Therefore the infected cells were seeded in several concentrations: 1 × 106, 2 × 105, 4 × 104, and 8 × 103 per mL. The cultures were established in 96-well plates containing 200 μL of these suspensions. To parallel cultures, 25 μg/mL PSK, 100 nM Trx80, and 20 U/mL IL-2 were added as indicated. To test the involvement of IL-15 or IL-12, neutralizing antibodies to human IL-15 or to IL-12 (p40/p70), respectively, were added at a concentration of 10 μg/mL. Each sample was represented by triplicate cultures. On day 12, 1 μCi (0.037 MBq) 3H-thymidine was added, and 14 hours later the cells were harvested onto glass fiber filters. Radioactivity was measured in a liquid scintillation counter. At this time, the results reflect the number of transformed B cells that established in the cultures.10
EBV-infected cord blood B cells were adjusted to 1 × 106/mL, and 200 μL of cells was cultured in 96-well plates. Parallel cultures contained 100 nM Trx80. Each sample was represented by triplicates. 3H-thymidine (1 μCi [0.037 MBq]) was present in the wells for the final 14 hours of the indicated periods.
Flow cytometric analysis
The cell surface markers CD3, CD4, CD8, CD14, CD19, and CD56 were detected with FITC-, PE-, or PE-Cy5–conjugated mouse antihuman monoclonal antibodies. The cells were harvested and washed once with PBS/1% FCS, incubated for 30 minutes at 4°C with indicated antibodies, washed once with PBS/1% FCS, and resuspended in 500 μL PBS. Events (10 000) were collected on a FACScan flow cytometer, and the results were analyzed using Cell Quest software (Becton Dickinson, San Jose, CA). Dead cells were excluded by cell size or by staining with propidium iodide.
Detection of intracellular cytokines
EBV-infected CBMCs were cultured as indicated for 48 hours. During the final 10 hours, monensin (2 μM) was added. The cells were then washed once with PBS; incubated for 30 minutes with the PE- or PE-Cy5–conjugated mAb against CD14, CD3, CD56, and CD19; washed once with PBS; treated with 4% paraformaldehyde for 30 minutes at 4°C; washed once with PBS; and permeabilized with PBS/0.2% saponin buffer. This was followed by incubating for one hour with mouse anti–human IL-12 mAb or IL-15 mAb, thereafter washed once with PBS/0.2% saponin buffer and incubated for 30 minutes with FITC-conjugated rabbit antimouse antibodies. The cells were then washed twice with PBS/0.2% saponin and resuspended in 500 μL PBS. The incubation with the Abs was performed at 4°C. The cells were analyzed in a FACSCalibur, and the results were analyzed using Cell Quest software (Becton Dickinson).
Detection of cytokines in the culture medium
EBV-infected CBMCs or monocyte-depleted populations were cultured in 24-well plates as indicated.
Isolated monocytes were exposed for 20 hours with PSK, Trx80, or PSK plus Trx80, and then reintroduced to the monocyte-depleted cultures. Supernatants of the cultures were collected 3 and 6 days later, and analyzed in duplicate wells using sandwich ELISA for IL-15 and IL-12 according to the manufacturer's instructions. The sandwich ELISA for IL-12 detected the IL-12 p70 heterodimer. The detection limit of the IL-15 and IL-12 was 10 pg/mL.
Immunoblotting
The cells were lysed directly in sodium dodecyl sulfate (SDS) gel-loading buffer. Aliquots corresponding to 1 × 105 cells were electrophoresed on 12% SDS–polyacrylamide gel electrophoresis gel and transferred to polyvinylidenefluoride membranes at 75 V for 2 hours. After blocking for one hour with 5% nonfat dried milk in PBS–Tween 20, the membranes were incubated with the anti-SAP antibody overnight at 4°C. The blots were then incubated with HRP-conjugated donkey anti–rabbit Ig antibody and developed with ECL + Plus detection reagent. Hyperfilm-ECL film was exposed to the developed membranes for visualization.
Cytotoxic function generated in the cultures
Viable cells collected from the cultures were stimulated on days 7 and 14, at 10:1 ratio, with irradiated (50 Gy) autologous EBV-infected B cells. At each stimulation, half of the medium was replaced with fresh medium containing 100 nM Trx80 or 100 nM Trx80 plus 25 μg/mL PSK. From the 9th day, 20 U/mL IL-2 was added every third day. On the 19th day, B cells were depleted from the populations using anti-CD19 Ab-conjugated beads. The remaining cells were used as effectors in 51Cr-release cytotoxicity assay. Autologous EBV-infected B cells, allogeneic lymphoblastoid cell lines (LCLs), autologous B cells activated with CD40 ligand (CD40L) and IL-4, and K562 were used as targets.
Autologous target cells were used also after 30-minute incubation with the mAb W6/32 (anti–HLA class I) or with the mAb CR3/43 (anti–HLA class II).
The specific lysis of triplicate cultures was calculated as follows: specific release = [(experimental release – spontaneous release)/(maximum release – spontaneous release)] × 100.
Measurement of intracellular ROS generation
Monocytes were incubated with PSK (25 μg/mL) or Trx80 (100 nM) for 12 hours. In order to test the role of PI 3-kinase and ROSs, aliquots of monocytes were pretreated for one hour with the PI 3-kinase–specific inhibitor LY294002 (10 μM) or with the antioxidant NAC (5 mM). ROS prober dye 2′,7′-dichlorofluorescin diacetate (H2DCFDA; 5 μM) was added to the final one-hour incubation. The cells were removed by trypsin and analyzed immediately. Determination of intracellular oxidant production was based on the oxidation of H2DCFDA by intracellular ROSs, resulting in the formation of the fluorescent compound 2′, 7′-dichlorofluorescin (DCF). DCF fluorescence was monitored in FACSCalibur (excitation wavelength, 488 nm; emission wavelength, 515-545 nm), and the results were analyzed using Cell Quest software (Becton Dickinson).
Statistical analysis
The data are expressed as the mean ± SEM or ± SD. Statistical significance was determined using paired 2-tailed Student t test. Differences were considered statistically significant for P values less than .05. Significance is presented for individual experiments (*P < .05; **P < .01).
Results
PSK and Trx80 potentiate T-cell activation in EBV-infected cord blood cell cultures
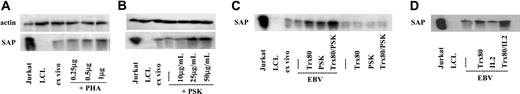
We have shown earlier that activated T and NK cells, but not B cells and macrophages, express SAP protein.18 Therefore we could use SAP detection by immunoblot for indication of the presence of activated T and NK cells in a mixed population. The intensity of the SAP band was taken to reflect the level of T- and NK cell activation. The use of SAP expression as a sign for activation was validated in the T-cell–enriched CMBC fraction exposed to phytohemagglutinin (PHA) for 3 days. A small proportion of T cells in CBMCs is known to be in an activated state. In line with this, SAP protein bands of variable intensity were detected in the immunoblots of the ex vivo samples. The dose response of the PHA-induced T-cell activation could be followed by the intensity of the SAP band (Figure 1A).
SAP expression reflects the presence of activated T cells. Immunoblot of lysates corresponding to 1 × 105 cells. In all experiments, Jurkat and LCLs were used as positive and negative controls, respectively. (A) T-enriched cells from cord blood were exposed to PHA for 3 days. Dose response. (B) EBV-infected CBMCs cultured with 10 μg/mL, 25 μg/mL, and 50 μg/mL PSK. (C) Cultures of CBMCs were initiated with or without EBV infection. Trx80 (100 nM), PSK (25 μg/mL), or Trx80 + PSK were added as indicated. The results show 1 of 4 experiments. (D) To the EBV-infected CBMC cells Trx80, IL-2 (20 U/mL), or both were added as indicated. Panels B-D represent results of 6-day-old cultures.
SAP expression reflects the presence of activated T cells. Immunoblot of lysates corresponding to 1 × 105 cells. In all experiments, Jurkat and LCLs were used as positive and negative controls, respectively. (A) T-enriched cells from cord blood were exposed to PHA for 3 days. Dose response. (B) EBV-infected CBMCs cultured with 10 μg/mL, 25 μg/mL, and 50 μg/mL PSK. (C) Cultures of CBMCs were initiated with or without EBV infection. Trx80 (100 nM), PSK (25 μg/mL), or Trx80 + PSK were added as indicated. The results show 1 of 4 experiments. (D) To the EBV-infected CBMC cells Trx80, IL-2 (20 U/mL), or both were added as indicated. Panels B-D represent results of 6-day-old cultures.
In our previous study, we added 50 μg/mL PSK to EBV-infected CBMCs.8 The dose response of PSK (Figure 1B) showed that 25 μg/mL PSK is sufficient to induce SAP. Therefore we used this dose throughout the present experiments. The proliferation of separated EBV-infected B cells was not influenced by this dose (not shown).
The SAP band became weaker in the 6-day-old EBV-infected cultures compared with the initial samples. Since the samples were analyzed on the basis of cell numbers, the lower intensity of the SAP band can be ascribed to the EBV-induced proliferation and the increase of the proportion of SAP-negative B blasts. We could confirm our previous finding that introduction of PSK to the culture enhanced SAP expression. Similarly, addition of Trx80 to the EBV-infected culture resulted in stronger SAP protein band (Figure 1C). The intensity of the SAP band increased only in the EBV-infected cultures and only when PSK or Trx80 was added. Presence of both PSK and Trx80 in the infected culture led to higher SAP expression.
Trx80 was shown to induce IL-12 secretion and to stimulate IFN-γ production in synergy with low doses of IL-2 (20 U/mL) in PBMC cultures.13 We therefore added both IL-2 (20 U/mL) and Trx80 to the infected cultures (Figure 1D) and found that SAP induction became potentiated. This low dose of IL-2 (20 U/mL) alone had no detectable effect.
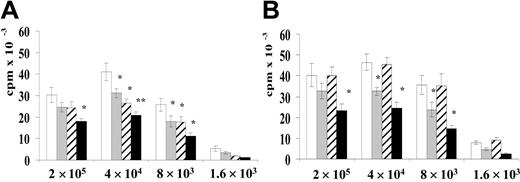
PSK and Trx80 inhibit EBV-induced B-cell transformation
EBV-infected CBMC cultures were initiated with 4 different cell numbers without or with Trx80 or PSK, separately and together. B-cell transformation by EBV was assessed by measuring the thymidine incorporation on the 12th day (Figure 2A). The results reflect the size of the B-cell population and show the efficiency of B-cell transformation.10 The outgrowth of B cells was inhibited as shown by lower values when Trx80 or PSK was added to the cultures.
Outgrowth of B cells in EBV-infected CBMC cultures. The outgrowth of B cells was detected by thymidine incorporation of the 12-day-old cultures. 3H-thymidine was present during the final 14 hours. The cultures initiated with the indicated cell numbers were cultured (A) without (□), or with Trx80 (▦), PSK (▨), or Trx80 + PSK (▪). (B) Cultures without (□), or with Trx80 (▦), IL-2 alone (▨), or Trx80 + IL-2 (▪). The results represent the mean ± SEM of 3 independent experiments. *P < .05 and **P < .01 compared with untreated cultures.
Outgrowth of B cells in EBV-infected CBMC cultures. The outgrowth of B cells was detected by thymidine incorporation of the 12-day-old cultures. 3H-thymidine was present during the final 14 hours. The cultures initiated with the indicated cell numbers were cultured (A) without (□), or with Trx80 (▦), PSK (▨), or Trx80 + PSK (▪). (B) Cultures without (□), or with Trx80 (▦), IL-2 alone (▨), or Trx80 + IL-2 (▪). The results represent the mean ± SEM of 3 independent experiments. *P < .05 and **P < .01 compared with untreated cultures.
In accordance with the synergy of PSK and Trx80 on T-cell activation, as indicated by the intensity of the SAP band in Figure 1B, inhibition of B-cell outgrowth was also more efficient in the cultures that received both PSK and Trx80. The potentiation of Trx80 effect by IL-2 was seen in the outgrowth inhibition test as well (Figure 2B).
The decrease in B-cell growth could be ascribed to the potentiation of the T- and NK cell–mediated inhibition. During a 6-day culture period, Trx80 did not inhibit the EBV-induced proliferation of isolated B cells (not shown).
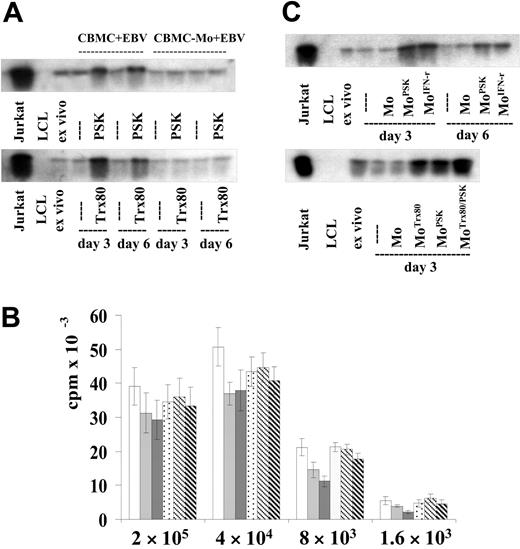
The effect of PSK and Trx80 is mediated by monocytes
Activation of T cells by PSK or Trx80 in the culture required the presence of monocytes (Figure 3A). SAP protein was not induced in cultures that did not contain monocytes. The outgrowth inhibition test showed similar results. In the absence of monocytes, PSK and Trx80 did not inhibit B-cell outgrowth (Figure 3B).
Requirement of monocytes for the effect of PSK and Trx80. In panels A and C, T-cell activation was detected by SAP expression, as in Figure 1. (A) EBV-infected CBMC total and monocyte-depleted populations were cultured with PSK (25 μg/mL) or Trx80 (100 nM) as indicated. Cells from 3- and 6-day-old cultures were tested. The results show 1 of 4 experiments. (B) B-cell outgrowth was determined as in Figure 2. EBV-infected CBMC total and monocyte-depleted populations were cultured with Trx80 or with PSK. The results are shown in the following order: total population without, with Trx80, or with PSK; monocyte-depleted population without, with Trx80, or with PSK. Error bars indicate SD of triplicate cultures. One further experiment showed similar results. (C) Monocyte-depleted CBMCs were infected with EBV. Aliquots of the isolated monocytes were treated for 20 hours with PSK, IFN-γ (500 U/mL), Trx80, or Trx80 + PSK. They were reintroduced to the monocyte-depleted cultures. The results show 1 of 5 experiments.
Requirement of monocytes for the effect of PSK and Trx80. In panels A and C, T-cell activation was detected by SAP expression, as in Figure 1. (A) EBV-infected CBMC total and monocyte-depleted populations were cultured with PSK (25 μg/mL) or Trx80 (100 nM) as indicated. Cells from 3- and 6-day-old cultures were tested. The results show 1 of 4 experiments. (B) B-cell outgrowth was determined as in Figure 2. EBV-infected CBMC total and monocyte-depleted populations were cultured with Trx80 or with PSK. The results are shown in the following order: total population without, with Trx80, or with PSK; monocyte-depleted population without, with Trx80, or with PSK. Error bars indicate SD of triplicate cultures. One further experiment showed similar results. (C) Monocyte-depleted CBMCs were infected with EBV. Aliquots of the isolated monocytes were treated for 20 hours with PSK, IFN-γ (500 U/mL), Trx80, or Trx80 + PSK. They were reintroduced to the monocyte-depleted cultures. The results show 1 of 5 experiments.
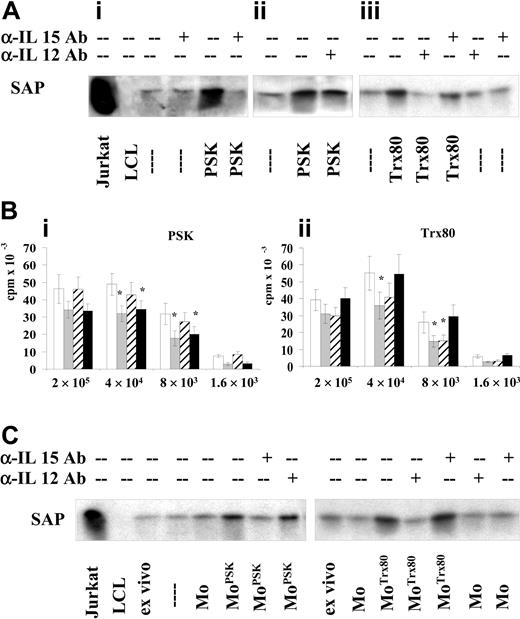
Antibodies against IL-15 or IL-12 inhibit PSK- or Trx80-induced T-cell activation, respectively
The effect of PSK-activated monocytes was mediated by IL-15 (Figure 4A), because antibodies against IL-15 prevented the induction of SAP band in the EBV-infected cells when PSK was added. Antibodies against IL-12 reduced slightly the intensity of the SAP band. In a parallel experiment, when the culture contained the Trx80, antibodies against IL-12 but not against IL-15 inhibited the induction of SAP (Figure 4Aiii).
Antibodies against IL-15 or IL-12 abrogated the effect of PSK and Trx80, respectively. (A) EBV-infected CBMCs were cultured with PSK or Trx80 in the presence of antibodies against IL-15 (10 μg/mL) or IL-12 (10 μg/mL). SAP expression was assayed on the sixth day. Panels Ai-iii are results from different experiments. Cultures containing PSK (i) without and with antibodies against IL-15, and (ii) without and with antibodies against IL-12; and (iii) cultures containing Trx80 without and with antibodies against IL-15 or IL-12. The results show 1 of 3 experiments. (B) 3H-thymidine incorporation of the cells in 12-day-old cultures containing neutralizing antibodies of IL-15 or IL-12. (i) Cultures without (□), or with PSK (▦), PSK and anti–IL-15 Ab (▨), or PSK and anti–IL-12Ab (▪); (ii) cultures without (□), or with Trx80 (▦), Trx80 and anti–IL-15Ab (▨), or Trx80 and anti–IL-12 Ab (▪). The results represent the mean ± SEM of 3 independent experiments. *P < .05 compared with untreated cultures. (C) EBV-infected monocyte-depleted populations were cultured. The monocytes without pretreatment or with PSK or Trx80 for 20 hours were reintroduced as indicated. To parallel IL-15 or IL-12, neutralizing antibodies were added. SAP expression was assayed in cells of 3-day-old cultures.
Antibodies against IL-15 or IL-12 abrogated the effect of PSK and Trx80, respectively. (A) EBV-infected CBMCs were cultured with PSK or Trx80 in the presence of antibodies against IL-15 (10 μg/mL) or IL-12 (10 μg/mL). SAP expression was assayed on the sixth day. Panels Ai-iii are results from different experiments. Cultures containing PSK (i) without and with antibodies against IL-15, and (ii) without and with antibodies against IL-12; and (iii) cultures containing Trx80 without and with antibodies against IL-15 or IL-12. The results show 1 of 3 experiments. (B) 3H-thymidine incorporation of the cells in 12-day-old cultures containing neutralizing antibodies of IL-15 or IL-12. (i) Cultures without (□), or with PSK (▦), PSK and anti–IL-15 Ab (▨), or PSK and anti–IL-12Ab (▪); (ii) cultures without (□), or with Trx80 (▦), Trx80 and anti–IL-15Ab (▨), or Trx80 and anti–IL-12 Ab (▪). The results represent the mean ± SEM of 3 independent experiments. *P < .05 compared with untreated cultures. (C) EBV-infected monocyte-depleted populations were cultured. The monocytes without pretreatment or with PSK or Trx80 for 20 hours were reintroduced as indicated. To parallel IL-15 or IL-12, neutralizing antibodies were added. SAP expression was assayed in cells of 3-day-old cultures.
In accordance with the results on T-cell activation, the effect of PSK on B-cell growth inhibition was substantially reduced by addition of anti–IL-15 antibodies at the initiation of the cultures (Figure 4Bi), while antibodies against IL-12 counteracted the inhibitory effect of Trx80 (Figure 4Bii).
The specific effect of the antibodies against the cytokines was also shown in the monocyte-reconstituted cultures. Monocytes exposed to the stimulators and treated with the relevant antibodies did not induce activation of the effector cells; the level of SAP expression did not increase in the cultures (Figure 4C).
IL-15 and IL-12 are detected in the culture media
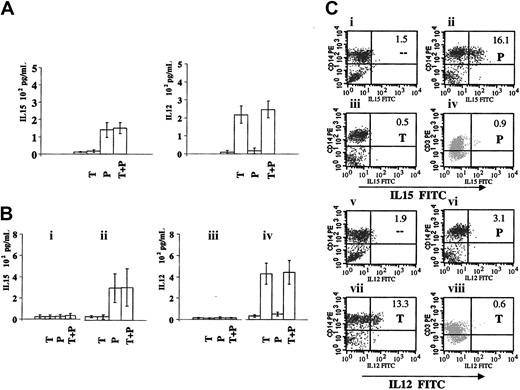
The cytokines were detected in the culture media. PSK-containing cultures produced IL-15, while Trx80-containing cultures produced IL-12 (Figure 5A).
Cytokine production in the PSK- or Trx80-containing CBMC cultures. (A-B) IL-15 and IL-12 content in the supernatant of 3-day-old cultures tested by ELISA. Cultures with Trx80, PSK, or Trx80 + PSK are marked as T, P, and T + P, respectively. (A) EBV-infected CBMCs. The results represent mean ± SD of 3 independent experiments. (B) The monocyte-depleted population was infected with EBV. (i,iii) Cultured without or with Trx80, PSK, or Trx80 + PSK. (ii,iv) The isolated monocytes were exposed for 20 hours without or with Trx80, PSK, or Trx80 + PSK and reintroduced to the cultures. The results represent mean ± SD of 4 independent experiments. (C) Intracellular expression of IL-15 and IL-12 detected by flow cytometry. EBV-infected CBMCs were cultured alone or with Trx80 or PSK for 48 hours. During the final 10 hours, monensin was added. Panels Ci-iii and Cv-vii show IL-15 or IL-12 expression of the CD14+ monocytes in the gated large cell population. Panels Civ and Cviii show IL-15 or IL-12 expression of the CD3+ T cells in the gated small populations. The results show 1 of 3 independent experiments with similar results.
Cytokine production in the PSK- or Trx80-containing CBMC cultures. (A-B) IL-15 and IL-12 content in the supernatant of 3-day-old cultures tested by ELISA. Cultures with Trx80, PSK, or Trx80 + PSK are marked as T, P, and T + P, respectively. (A) EBV-infected CBMCs. The results represent mean ± SD of 3 independent experiments. (B) The monocyte-depleted population was infected with EBV. (i,iii) Cultured without or with Trx80, PSK, or Trx80 + PSK. (ii,iv) The isolated monocytes were exposed for 20 hours without or with Trx80, PSK, or Trx80 + PSK and reintroduced to the cultures. The results represent mean ± SD of 4 independent experiments. (C) Intracellular expression of IL-15 and IL-12 detected by flow cytometry. EBV-infected CBMCs were cultured alone or with Trx80 or PSK for 48 hours. During the final 10 hours, monensin was added. Panels Ci-iii and Cv-vii show IL-15 or IL-12 expression of the CD14+ monocytes in the gated large cell population. Panels Civ and Cviii show IL-15 or IL-12 expression of the CD3+ T cells in the gated small populations. The results show 1 of 3 independent experiments with similar results.
Similar results were obtained when pretreated monocytes were reintroduced to the depleted cell population. Only very low levels of IL-12 and IL-15 were detected in the cultures to which untreated monocytes (Mos) were added. The supernatants of 3-day-old cultures with reintroduced PSK-treated monocytes contained IL-15, while IL-12 was detected in cultures that received the Trx80-treated monocytes (Figure 5Bii,iii).
In the absence of monocytes, the supernatants did not contain these cytokines (Figure 5Bi,iii). The Trx80- or PSK-treated monocytes did not produce IL-12 and IL-15 (not shown).
IL-15 or IL-12 is expressed in the monocytes
EBV-infected CBMCs were cultured for 48 hours with PSK or with Trx80. CD14+ cells were analyzed for the expression of IL-12 or IL-15 (Figure 5C). No IL-12– and IL-15–expressing cells could be recorded in the gated small cell population that consisted of CD3+ T, CD19+ B, and CD56+ NK cells (Figure 5Civ,viii and not shown). Analysis of the gated large cells showed that 1.5% of the CD14+ cells expressed IL-15 and 1.9% expressed IL-12 in the EBV-infected cultures, which did not receive the immunomodulators. When the population was cultured with PSK, 16.1% of the CD14+ cells expressed IL-15, and 3.1% expressed IL-12. In the Trx80-containing cultures, 13.3% were IL-12 positive, and 0.5% were IL-15 positive.
EBV-specific cytotoxic cells can be generated in the cultures
The cultures were stimulated twice with autologous EBV-infected B cells, in the presence of 20 U/mL IL-2 and 100 nM Trx80 or 100 nM Trx80 and 25 μg/mL PSK. The composition of the populations in the 19-day-old cultures showed that B cells did not proliferate and the population consisted mainly of CD4+ T cells (Table 1).
Composition of the populations in 19-day-old cultures initiated with EBV-infected CBMCs
Cells . | CBMC + EBV, % . | CBMC + EBV + Trx80, % . | CBMC + EBV + Trx80 + PSK, % . |
|---|---|---|---|
| CD19 B | 93.1 | 18.9 | 5.6 |
| CD4 T | 4.9 | 63.1 | 54.3 |
| CD8 T | 0.7 | 6.2 | 7.8 |
| CD56 NK | 1.9 | 6.9 | 18.6 |
| CD3 T | 5.3 | 70.7 | 62.6 |
Cells . | CBMC + EBV, % . | CBMC + EBV + Trx80, % . | CBMC + EBV + Trx80 + PSK, % . |
|---|---|---|---|
| CD19 B | 93.1 | 18.9 | 5.6 |
| CD4 T | 4.9 | 63.1 | 54.3 |
| CD8 T | 0.7 | 6.2 | 7.8 |
| CD56 NK | 1.9 | 6.9 | 18.6 |
| CD3 T | 5.3 | 70.7 | 62.6 |
The cultures were restimulated twice, on the 7th and 14th days with irradiated (50 Gy) autologous EBV-infected B cells. Half of the culture medium was replaced with fresh medium containing 100 nM Trx80 or 100 nM Trx80 and 25 μg/mL PSK. From the ninth day, 20 U/mL IL-2 was added every third day.
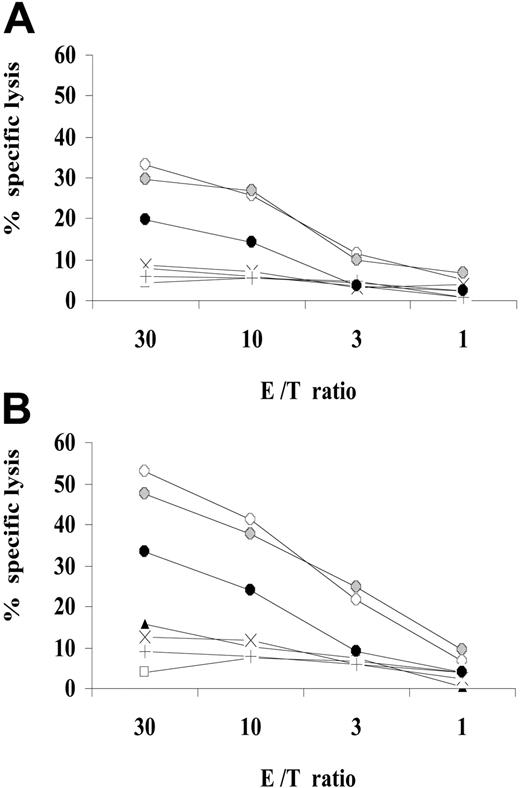
At this time, B lymphocytes were removed and the cytotoxic function of the remaining cells was tested against the following: autologous EBV-infected B cells, autologous B cells activated with CD40L and IL-4, and allogeneic LCLs and K562 cells. The cells of the Trx80-containing cultures had appreciable cytotoxicity to the autologous EBV-infected B cells (26% at 10 of effector-target [E/T] ratio; Figure 6A). The activity was stronger in Trx80/PSK cultures, indicating a synergism of activation (41% at 10 of E/T ratio; Figure 6B). The lysis of autologous target was reduced by HLA class II mAbs CR3/43.
Cytotoxic function generated after restimulation of the Trx80- and PSK-containing EBV-infected CBMC cultures. The EBV-infected cultures containing Trx80 or Trx80 and PSK were restimulated on the days 7 and 14 with irradiated (50 Gy) autologous EBV-infected B cells, at a ratio of 10:1, in the presence of Trx80 or Trx80 plus PSK. Beginning on day 9, 20 U/mL IL-2 was added every third day. On day 19, B lymphocytes were depleted. The remaining cells were tested for cytotoxic function. (A) Effector cells from Trx80-containing cultures. (B) Effector cells from Trx80 + PSK–containing cultures. Targets: autologous EBV-infected B cells (○), preincubated with mAb W6/32 (⬡), preincubated with mAb CR3/43 (•); autologous CD40L- and IL-4–activated B cells (□); K562 (▴); allogeneic LCLs: CBM1 (X); LS-LCL (+).
Cytotoxic function generated after restimulation of the Trx80- and PSK-containing EBV-infected CBMC cultures. The EBV-infected cultures containing Trx80 or Trx80 and PSK were restimulated on the days 7 and 14 with irradiated (50 Gy) autologous EBV-infected B cells, at a ratio of 10:1, in the presence of Trx80 or Trx80 plus PSK. Beginning on day 9, 20 U/mL IL-2 was added every third day. On day 19, B lymphocytes were depleted. The remaining cells were tested for cytotoxic function. (A) Effector cells from Trx80-containing cultures. (B) Effector cells from Trx80 + PSK–containing cultures. Targets: autologous EBV-infected B cells (○), preincubated with mAb W6/32 (⬡), preincubated with mAb CR3/43 (•); autologous CD40L- and IL-4–activated B cells (□); K562 (▴); allogeneic LCLs: CBM1 (X); LS-LCL (+).
Earlier we have reported similar results in this system when the cultures contained PSK. K562, the classical NK target, was also lysed by effector cells originating from the Trx80/PSK cultures, but the effect was weaker than against the specific target. The lysis of K562 cells reflected enrichment of NK cells. The composition of the populations indicated also the elevated proportion of CD56+ NK cells in the Trx80/PSK cultures (Table 1). Autologous CD40L-activated B cells were not lysed.19,20 It is therefore likely that EBV-specific T-cell cytotoxicity was generated in the cultures.
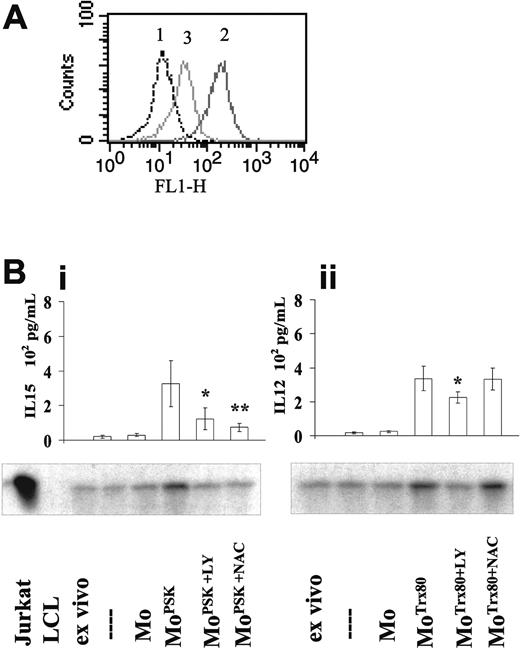
PI 3-K and ROSs are involved in PSK-induced monocyte activation
Activation of monocytes involves the phosphatidylinositol 3 (PI 3)–kinase pathway and is accompanied by the induction of reactive oxygen species (ROSs).21,22 Monocytes treated with PSK for 12 hours produced ROSs (Figure 7A). The DCF fluorescence increased 9-fold in the treated cells, and the mean fluorescence intensity changed from 14 to 134, which was substantially counter-acted by pretreatment with the antioxidant NAC.
PI 3-kinase and ROS involvement in the activation and cytokine production of monocytes. Aliquots of monocytes were incubated for one hour with the PI 3-kinase inhibitor LY294002 (10 μM), or with the antioxidant NAC (5 mM), and thereafter exposed to PSK or Trx80 for 12 hours. DCFH-DA (5 μM) was added during the final 1-hour incubation to 1 aliquot of the PSK-treated monocytes. (A) Flow cytometry FACS analysis of DCFH-DA, which indicates ROS production. Monocytes without treatment, PSK treated, NAC + PSK treated are indicated by 1, 2, and 3, respectively. The results show 1 of 4 experiments. (B) The treated monocytes were reintroduced to the EBV-infected monocyte-depleted cultures. (i) PSK-exposed monocytes. (ii) Trx80-exposed monocytes reintroduced to the cultures. After 48 hours, the culture media were collected and analyzed for IL-15 and IL-12 content. *P < .05 and **P < .01 as compared with cultures to which PSK-exposed (i) or Trx80-exposed (ii) monocytes were re-introduced. The results represent mean ± SD of 3 independent experiments; the cell populations were tested for SAP expression. The results show 1 of 3 experiments.
PI 3-kinase and ROS involvement in the activation and cytokine production of monocytes. Aliquots of monocytes were incubated for one hour with the PI 3-kinase inhibitor LY294002 (10 μM), or with the antioxidant NAC (5 mM), and thereafter exposed to PSK or Trx80 for 12 hours. DCFH-DA (5 μM) was added during the final 1-hour incubation to 1 aliquot of the PSK-treated monocytes. (A) Flow cytometry FACS analysis of DCFH-DA, which indicates ROS production. Monocytes without treatment, PSK treated, NAC + PSK treated are indicated by 1, 2, and 3, respectively. The results show 1 of 4 experiments. (B) The treated monocytes were reintroduced to the EBV-infected monocyte-depleted cultures. (i) PSK-exposed monocytes. (ii) Trx80-exposed monocytes reintroduced to the cultures. After 48 hours, the culture media were collected and analyzed for IL-15 and IL-12 content. *P < .05 and **P < .01 as compared with cultures to which PSK-exposed (i) or Trx80-exposed (ii) monocytes were re-introduced. The results represent mean ± SD of 3 independent experiments; the cell populations were tested for SAP expression. The results show 1 of 3 experiments.
The functional tests substantiated the results (Figure 7Bi). IL-15 was produced and the T cells were activated in the EBV-infected cultures to which PSK-treated monocytes were added. But in the cultures that received monocytes treated with the antioxidant and PSK, the level of IL-15 was lower and the SAP band became weaker.
The same experimental strategy with monocytes activated by Trx80 showed similar results (Figure 7Bii). The response of monocytes to Trx80 was not abrogated by pretreatment with the antioxidant NAC, however.
When the inhibitor-treated monocytes were reintroduced into the PSK- or Trx80-containing cultures, EBV-transformed B cells grew and dominated the population. Cytotoxic cells were not generated in these cultures.
Discussion
EBV-specific cellular immunity is not transmitted from mother to child. Therefore cord blood lymphocyte populations infected with EBV in vitro can yield transformed B-cell cultures without the necessity to remove or to inhibit the T cells. Previously we and others have demonstrated T and/or NK responses in EBV-infected cord blood lymphocyte populations. We detected this response with the help of the immunomodulator PSK. When PSK was added, B-cell transformation was inhibited and CD4 T cells and NK cells were enriched in the cultures. Restimulation of the cultures generated specific cytotoxicity against autologous EBV-infected B cells.10 The latter results were similar to those reported earlier by Sun et al5 who showed that stimulation of cord blood cells with autologous LCLs generated CD4 T-cell–mediated cytotoxic function. They obtained similar results with lymphocytes collected from seronegative individuals. Subsequently Wilson and Morgan reported CD4 T and CD16 CD56 NK cell response in EBV-infected cord blood samples.6 In analysis of the early phase EBV-induced B-cell proliferation, Nikiforow et al showed that CD4 T cells inhibited the outgrowth of B cells and helped the CD8 T-cell response.23 In comparative experiments on the cytotoxic T lymphocyte (CTL) generation in lymphocyte cultures derived from seronegative children and adults, Savoldo et al24 found also predominantly class II–restricted CD4 responses. Interestingly, in order to obtain EBV-specific CTL cultures, the experimental strategy with the cells of children needed the selection of CD25+ T cells from the cultures stimulated with autologous LCLs. Our results suggest that addition of PSK or Trx80 to the lymphocyte population may be used for this goal and thus simplify the procedure for generation of a primary response.
We have now confirmed the PSK-induced inhibition of EBV-induced B-cell growth in cord blood cell cultures and showed that it was mediated by activation of monocytes by PSK. We also found that Trx80 acted similarly, in that it inhibited B-cell transformation and its effect was also mediated by monocytes. Both PSK and Trx80 activated monocytes to produce cytokines, if activated T cells were in the culture. While the outcome of both treatments was similar, in that B-cell transformation was inhibited, the monocytes mediated their effects by different cytokines. Under the same conditions, PSK induced predominantly IL-15, while Trx80 induced IL-12. Both cytokines induced functional activation of the T cells. The contribution of the 2 cytokines was clearly shown by specific antibody-mediated abrogation of the T-cell activation and its impact on B-cell outgrowth.
Identification of the effector cells with regard to specificity requires further analysis. In the first step, the T and NK cells were exposed to B blasts, which could have led to their activation. According to our previous results, inhibition of B-cell outgrowth was an early effect, therefore it is unlikely that T cells with specific cytotoxicity were the mediators. Later, repeated stimulation of the effector cells with autologous EBV-transformed cells may have selected and enriched the antigen-specific CD4 cells.
The experiments with EBV-infected cord blood mononuclear cells revealed consecutive steps in the T-cell activation. We monitored T-cell activation by SAP expression. The cord blood lymphocyte population is known to contain activated T cells. Accordingly, a SAP band was detected in the immunoblot, with variation of intensity in the individual samples. However the SAP level did not increase after EBV infection unless IL-15 or IL-12 was produced by monocytes under the influence of PSK or Trx80, and helped by activated T cells. In similar experiments performed with blood-derived mononuclear populations from adult individuals, SAP expression was elevated in the EBV-infected sample without the addition of the immunomodulators.18 It seems therefore that in cell populations collected from adults, the EBV-specific memory T cells recognized the EBV-infected B cells and became activated for SAP expression. In such cultures, the T cells are known to inhibit B-cell outgrowth. Thus, comparison of our earlier and present experiments with cell populations collected from adult and cord blood shows a difference depending on the existence of EBV-specific cellular memory.
Interaction of activated T cells and activated monocytes is known to occur through their surface CD40L-CD40, respectively. We envisage the following scenario: Recognition of EBV-infected B cells induced CD40L expression in a proportion of the T cells. Preliminary results obtained in 2 experiments with 3-day-old cultures showed CD40L expression in the CD3 population as follows: CBMC 2%, 2%; CBMCs + EBV 18%, 11%; CBMCs + EBV + PSK 24%, 27%; CBMCs + EBV + Trx80, 24% in one experiment.
This stage of T-cell activation was not accompanied by SAP expression. Activation of monocytes is known to up-regulate their surface CD40. This has been induced by both PSK and Trx80. As a consequence of the positive feedback between T cells and monocytes, mediated in part by CD40 ligation, the monocytes produced IL-15 or IL-12, respectively. These cytokines triggered the T cells for functional activity, in this case inhibiting B-cell transformation. SAP expression in the T and NK cells increased concurrently. The mechanism by which SAP contributes to the activation of T and NK cells is not known. Its importance in cellular immunity is suggested by the development of serious, often fatal disease induced by the first encounter with EBV in patients who lack or have a mutated SAP gene.
The events induced by the Trx80 treatment of the monocytes in the EBV-infected CBMCs corresponded to earlier findings in uninfected adult blood mononuclear cells, with regard to IL-12 production and the requirement of contact with T lymphocytes.13 Trx80 was shown to induce monocyte differentiation with increased expression of CD14, CD40, CD54, and CD86.13,14 In our cord blood system, IL-15 and IL-12 production was not induced in the culture unless the T cells were activated by the presence of EBV-infected B cells. Activated T cells were probably present in the cell population of adult blood.
CD40L ligation synergizes with IL-12 in enhancing IFN-γ production of T cells.25,26 CD40 ligation was shown to require the presence of T-cell–derived costimulatory signals, such as IFN-γ or IL-4, for maximum induction of IL-12 (p70) in adult monocyte-derived dendritic cells (DCs).27,28 Through the interaction between the CD40L on activated T cells, induced by their contact with EBV-infected B cells, and the CD40 molecule on the Trx80-treated monocytes, the positive feedback for IFN-γ and IL-12 production is initiated.
The immunomodulator PSK has been shown to elevate the expression of CD40 and CD86 on dendritic cells.29 In this report, IL-12 production was measured and detected on day 7 after the dendritic cells were twice exposed to PSK. Production of IL-15 was not tested. This result differs from our experiments in which PSK induced IL-15 in the monocytes. This difference can be attributed to the different experimental conditions and to the different cell populations used. We studied the early effects on T-cell activation, and antibodies against IL-15, but not against IL-12, showed marked inhibition. The fact that introduction of PSK and Trx80 acted in synergy suggests that the cytokines acted at least in part on different lymphocyte subsets.
IL-15 has been shown to inhibit EBV-induced transformation in blood lymphocyte cultures.30 It activated NK cells and generated cytotoxic NK T cells. The enhanced T-cell activation and B-cell growth inhibition by PSK and Trx80 are in line with the demonstration that IL-15 and IL-12 synergize for IFN-γ production by T cells and induce NK-mediated cytotoxicity.11,31,32
We have thus shown that EBV-infected B lymphocytes could be recognized by T and NK cells in experimentally infected cord blood mononuclear cell populations. The EBV-induced outgrowth of B lymphocytes was inhibited when the resident monocytes were activated with immunomodulators. Feedback between the activated T cells and activated monocytes has led to IL-15 or IL-12 production, and the T cells acquired functional capacity. Importantly, the monocytes could be activated with Trx80, a natural 10-kDa fragment of thioredoxin. It exists in plasma and is secreted from activated cells together with full-length thioredoxin.13-15,33 Trx80 has unique functions in activating monocytes, an activity thioredoxin lacks. Furthermore Trx80 immunomodulation is not dependent on the redox active cysteine residues in thioredoxin,34,35 since a recombinant mutant Trx80 protein with serine residues is still active.36 Truncated thioredoxin was previously shown to be strongly expressed on the cell surface of monocytic cell lines such as U937, whereas it was only weakly expressed in other cell lines of B cells, T cells, and granulocytes.37 Thioredoxin, which is released upon oxidative stress, infection, and inflammation is a chemoattractant for neutrophils, monocytes, and T cells.38 Furthermore, thioredoxin acts as a cocytokine for T and B cells.39-41 Agents inducing secretion of Trx80 and thioredoxin may find applications in cancer immunotherapy.
Prepublished online as Blood First Edition Paper, October 26, 2004; DOI 10.1182/blood-2004-06-2406.
Supported by the Swedish Cancer Society and by the Cancer Research Institute (New York, NY)/Concern Foundation (Los Angeles, CA).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank the Department of Obstetrics and Gynecology, Karolinska University Hospital, for the provision of cord blood samples.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal