Abstract
The mechanisms of bone and blood formation have traditionally been viewed as distinct, unrelated processes, but compelling evidence suggests that they are intertwined. Based on observations that hematopoietic precursors reside close to endosteal surfaces, it was hypothesized that osteoblasts play a central role in hematopoiesis, and it has been shown that osteoblasts produce many factors essential for the survival, renewal, and maturation of hematopoietic stem cells (HSCs). Preceding these observations are studies demonstrating that the disruption or perturbation of normal osteoblastic function has a profound and central role in defining the operational structure of the HSC niche. These observations provide a glimpse of the dimensions and ramifications of HSC-osteoblast interactions. Although more research is required to secure a broader grasp of the molecular mechanisms that govern blood and bone biology, the central role for osteoblasts in hematopoietic stem cell regulation is reviewed herein from the perspectives of (1) historical context; (2) the role of the osteoblast in supporting stem cell survival, proliferation, and maintenance; (3) the participation, if any, of osteoblasts in the creation of a stem cell niche; (4) the molecules that mediate HSC-osteoblast interactions; (5) the role of osteoblasts in stem cell transplantation; and (6) possible future directions for investigation.
Introduction and historical perspective
Hematopoiesis occurs in unique microenvironments that facilitate the maintenance of hematopoietic stem cells (HSCs) as pluripotent and support the maturation of progenitors. Each of these activities may require different growth factors and microenvironments, the identities of which have yet to be determined. In vitro, bone marrow stromal cells (BMSCs) serve as a rich source of growth factors for a variety of hematopoietic processes. BMSCs are composed of several different populations, including fibroblasts, macrophages, endothelial cells, and adipocytes. Although it is difficult to discern the relative importance of each of these cells, it has been shown that direct stromal cell–blood cell contact, BMSC production of the extracellular bone marrow matrix, and cytokine synthesis are all relevant to the formation and maturation of blood cells in vitro.1-3 The role of BMSCs in vivo is less clear.
Osteoblasts have long been known to play a central role in skeletal development. Derived from pluripotent mesenchymal stem cells (MSCs), they mature along a specific lineage to become highly specialized synthetic cells. As such, osteoblasts respond to many mechanical, local, and systemic stimuli that facilitate mineralization while they orchestrate bone remodeling. Osteoblasts also constitute part of the stromal cell support system in marrow, but little is known about their functional relevance to HSCs. Early attempts to understand this relationship focused on the protective function that bone might serve for the hematopoietic organ.4 Observations in birds of recurrent trabeculation of the medullary cavity during ovulation show that the hematopoietic tissue regresses as bone encroaches the marrow space,5 strongly suggesting that osteogenesis and hematopoiesis are functionally linked. Similarly, during embryogenesis, rapid formation of primitive marrow occurs in bone resorption centers.6
Yet, despite the striking affiliations, surprisingly little is known regarding the impact of osteoblasts on the marrow microenvironment. Is it happenstance that the most active marrow is located in the interstices of cancellous bone and at the periphery of the medullary cavity of cortical bone concentrated on endosteal surfaces? Identification of the hematopoietic stem cell niche has been difficult, if not controversial. Patt and Maloney7 suggest that stroma itself is the principal determinant of the quality of hematopoiesis. Central questions, to which we will return later, such as why medullary cavities in bone become the normal site for definitive hematopoiesis and why new hematopoietic foci arise in close approximation with bone remain unanswered. Specifically, what is the operational structure of one microenvironment relative to another? Does a given microenvironment represent a transient state? Does the stromal cell per se provide HSC proliferative or commitment control, or both? Is there more than one type of regulatory stromal cell, or is a single type with specificity determined by ambient factors? These issues have been difficult to address.7 Several investigators report that a concentration gradient of pluripotent stem cells (spleen colony-forming units [CFU-Ss]) exists and decreases toward the central anteriol of the femoral medullary cavity in mice.8-10 The density of maturing granulocytes, on the other hand, increases with distance from the osseous surface (Figure 1).9 Because it is likely that local control of HSCs is characterized by specific inductive microenvironments,11 hematopoiesis is also likely influenced by the nature and character of the local blood flow.10,12
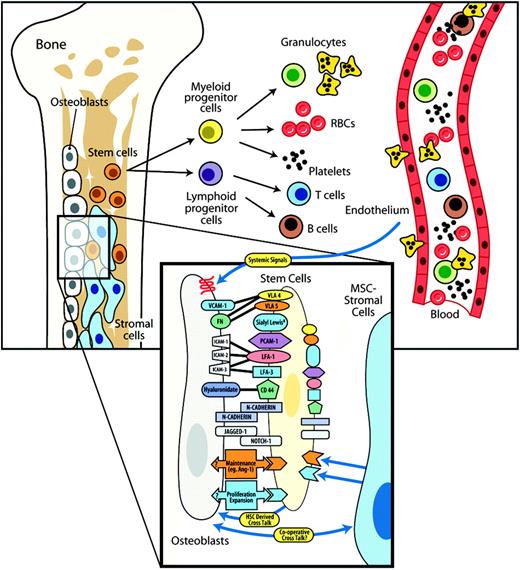
Model of support for hematopoietic stem cells by osteoblasts. The stem cell niche is composed of several members of the BMSC system, all derived from a common mesenchymal stem cell. Recent studies demonstrate that endosteal osteoblasts and their precursors play a critical role in the creation of a stem cell niche and thereby likely regulate stem cell maintenance, proliferation, and maturation. Central to this hypothesis is the demonstration that osteoblast-expressed regulatory components that influence stem cell function are likely to include cell-cell receptors, soluble and cell surface–associated cytokines, and growth factors. Each of these factors—those known and those yet to be determined—are likely influenced by mechanical, systemic (eg, PTH), and local (eg, BMPs, Ang-1) signals that regulate osteoblastic function. Furthermore, reciprocal cooperation between stem cells and osteoblasts and other cell types is likely to play a key role in the establishment and maintenance of the stem cell niche in the bone marrow.
Model of support for hematopoietic stem cells by osteoblasts. The stem cell niche is composed of several members of the BMSC system, all derived from a common mesenchymal stem cell. Recent studies demonstrate that endosteal osteoblasts and their precursors play a critical role in the creation of a stem cell niche and thereby likely regulate stem cell maintenance, proliferation, and maturation. Central to this hypothesis is the demonstration that osteoblast-expressed regulatory components that influence stem cell function are likely to include cell-cell receptors, soluble and cell surface–associated cytokines, and growth factors. Each of these factors—those known and those yet to be determined—are likely influenced by mechanical, systemic (eg, PTH), and local (eg, BMPs, Ang-1) signals that regulate osteoblastic function. Furthermore, reciprocal cooperation between stem cells and osteoblasts and other cell types is likely to play a key role in the establishment and maintenance of the stem cell niche in the bone marrow.
Historically, many investigators have suggested that osteoblasts regulate hematopoiesis because bone houses the marrow and osteoblasts induce the expansion and maturation of osteoclasts from hematopoietic precursors and activate osteoclastic bone resorption.13,14 Osteoclasts are derived from CD34+ hematopoietic cells and are primarily responsible for the resorption of mineralized tissues. Consequently, there may be many similarities in the way osteoblasts affect the behavior of osteoclasts and primitive hematopoietic cells. The specific nature of the osteoblast-derived activities that modulate or expand the osteoclast precursor pool is under extensive investigation and is known to be regulated by several hormones including parathyroid hormone (PTH), 1α,25-dihydroxy-vitamin D3, macrophage–colony-stimulating factor (M-CSF), rank-ligand, osteoprotegerin (OPG), and others. In addition to influencing osteoclast development, osteoblasts are involved in osteoclast activation. Receptors for cytokines and hormones that trigger mineralized tissue resorption are rarely observed on osteoclasts. By expressing receptors for bone-resorbing stimuli such as PTH and prostaglandins, osteoblasts appear to be the direct or primary target for these agents. Osteoblasts may also provide the “secondary” resorption signal(s). For example osteoblasts may express chemotactic signals to attract osteoclasts to mineralized surfaces and may modulate the expression of adhesion molecules to localize osteoclasts to bone resorption sites. From the foregoing, it is clear that hematopoietic precursors and osteoblasts have established communications for the production of osteoclasts or the activation of resorption, or both. However the arguments do not prove a role for osteoblasts in regulating stem cells. Thus, beyond that of the osteoclast, osteoblast participation in hematopoiesis has not yet been fully addressed.
What role do osteoblasts play in supporting stem cell survival, proliferation, and maintenance?
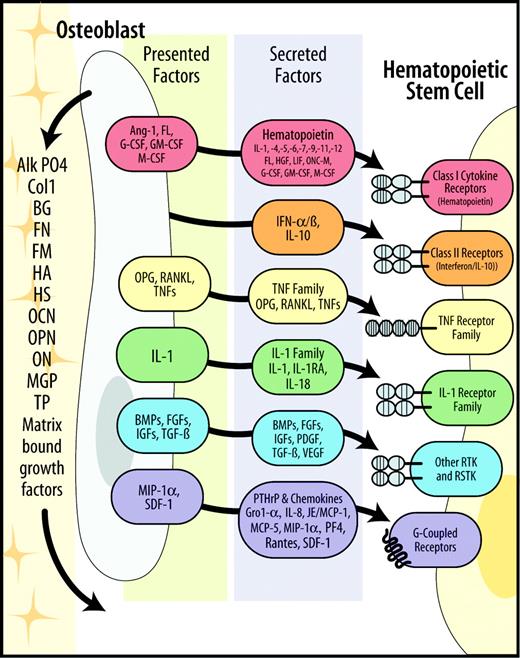
As a first step toward proving that osteoblasts support HSCs, many investigators have demonstrated that primary and transformed murine osteoblast cell lines secrete cytokines that could modulate stem cell function. The list includes granulocyte–colony-stimulating factor (G-CSF), M-CSF, GM-CSF, interleukin-1 (IL-1), IL-6, and others.15 Primary human osteoblasts have been less well characterized, but they express many molecules known to modulate hematopoiesis. For example G-CSF, GM-CSF, M-CSF, IL-1β, IL-6, IL-7, leukemia inhibitory factor (LIF), OPG, receptor activator of NF-κB ligand (RANKL), stromal-derived factor (SDF-1), tumor necrosis factor-α (TNF-α), and vascular endothelial growth factor (VEGF) have all be been detected using human cells (Figure 2).15-18 At present however, none of these cytokines, alone or in combination, appear to account for all the hematopoietic-supportive activities required to maintain and support HSC survival in vitro. Yet, though combinations of cytokines may not fully support HSC activities, long-term bone marrow cultures (LTBMCs) have been extensively used to define the role of stromal cell-derived factors in hematopoiesis (ie, Dexter or Whitlock-Witte cultures).19-22 Because many primary and transformed stromal cell lines themselves were derived from LTBMC cultures that form mineralized matrices in vitro,23,24 the inference has been that osteoblasts must participate in stem cell activities.25,26 An interesting early investigation demonstrated that in vivo nearly 50% of stromal cell–derived clones form bone when transplanted in vivo.27 More important, these same clones recruit circulating host hematopoietic progenitors to reestablish a fully functional marrow.27 Although interactions with other stromal constituents are known, these examples illustrate the potential role that osteogenic cells play in hematopoiesis.
Model of secreted and cell-associated factors produced by osteoblasts that influence HSCs. Stem cell fate is influenced by specialized microenvironments that remain poorly defined. Osteoblast production of soluble hematopoietic supportive–secreted and cell-associated factors work in concert so that hematopoietic stem cells derive regulatory information from bone, accounting for the localization of hematopoiesis in bone marrow. Alk P04 indicates alkaline phosphatase; BG, byglycan; BMPs, bone morphogenic factors; ColI, collagen type I; FGFs, fibroblast growth factors; FL, Flt ligand; FM, fibromodulin; FN, fibronectin; HGF, hepatocyte growth factor; HS, heparin sulfate proteoglycan; IGFs, insulinlike growth factors; IFN, interferon; JE/MCP-1, JE/monocyte chemotactic protein-1; MGP, matrix Gla protein; OC, osteocalcin; ON, osteonectin; ONC-M, oncostatin-M; OP, osteopontin; PDGF, platelet-derived growth factor; PF4, platelet factor 4; RSTK, serine/threonine kinase receptor; RTK, tyrosine kinase receptor; and TP, thrombospondin.
Model of secreted and cell-associated factors produced by osteoblasts that influence HSCs. Stem cell fate is influenced by specialized microenvironments that remain poorly defined. Osteoblast production of soluble hematopoietic supportive–secreted and cell-associated factors work in concert so that hematopoietic stem cells derive regulatory information from bone, accounting for the localization of hematopoiesis in bone marrow. Alk P04 indicates alkaline phosphatase; BG, byglycan; BMPs, bone morphogenic factors; ColI, collagen type I; FGFs, fibroblast growth factors; FL, Flt ligand; FM, fibromodulin; FN, fibronectin; HGF, hepatocyte growth factor; HS, heparin sulfate proteoglycan; IGFs, insulinlike growth factors; IFN, interferon; JE/MCP-1, JE/monocyte chemotactic protein-1; MGP, matrix Gla protein; OC, osteocalcin; ON, osteonectin; ONC-M, oncostatin-M; OP, osteopontin; PDGF, platelet-derived growth factor; PF4, platelet factor 4; RSTK, serine/threonine kinase receptor; RTK, tyrosine kinase receptor; and TP, thrombospondin.
Early work in this field has also focused on the direct effects that human or murine osteoblastlike cell lines have on hematopoiesis in vitro. Initially, several reports suggested that osteosarcoma cell lines do not support progenitor activities in methylcellulose assays. Therefore, by inference, neither do primary cells.24,28 We, too, have found that human osteosarcoma cell lines fail to support the survival of progenitor or long-term culture–initiating cell (LTC-IC) activities derived from bone marrow CD34+ cells, possibly because of the high levels of transforming growth factor-β (TGF-β) produced in these cell lines.29 Others, using the human CAL72 osteosarcoma cell line, demonstrated that a limited expansion of cord blood–derived hematopoietic progenitors similar to human primary osteoblasts is possible30 Yet these studies used CD34+ cells derived from cord blood, and they may not pertain directly to how osteoblasts function on the more restricted bone marrow cells.30 Similarly, other groups have shown that the U2-OS osteosarcoma cell line supports the proliferation of early bone marrow cells but not of progenitor cell activities.31 Together, these investigations suggest on the whole that, although osteosarcoma and transformed osteoblastic cell lines may support proliferation, their capacity to support early HSCs is limited.
During the past several years, a few laboratories, including our own, have specifically addressed the role of primary osteoblasts in hematopoiesis. Our first strategy toward determining the role of osteoblasts in hematopoiesis was to isolate primary osteoblastlike cells from human marrow trabecular/endosteal surfaces and then to determine which hematopoietic-supporting factors they produce. We have shown that primary human osteoblasts produce growth factors that are likely to be essential for the survival of CD34+ bone marrow cells.15,32,33 In so doing, we found that osteoblasts constitutively express G-CSF.34 This observation was exciting because the normal source(s) of G-CSF in human bone marrow was unknown. These findings led us to evaluate whether osteoblasts actually support the growth of CD34+ human bone marrow progenitors.35 Indeed, osteoblasts did stimulate the growth of the hematopoietic cells in vitro. By light microscopy, hematopoietic cells grown in the absence of any cell layers died (osteoblasts or BMSCs).36 Those grown in the presence of exogenous GM-CSF and IL-3 differentiated along the granulocytic pathway into bands/polymorpho-nuclear neutrophils. In the presence of osteoblasts, however, most of the recovered hematopoietic cells maintained an immature morphology.36 We next asked whether osteoblasts could support LTC-ICs. Here human CD34+ bone marrow progenitors were cultured on osteoblast monolayers. In osteoblast cultures, a substantial increase in the number of clonogenic progenitors was observed. CFUs also increased severalfold when cocultured with BMSCs or cytokines, but CFUs could not be detected in the absence of added cytokines. During the same period, a 3- to 4-fold expansion over input in the LTC-IC compartment occurred in the presence of osteoblasts, comparing favorably with BMSCs. As expected, no LTC-ICs were recovered from either cytokine control group.
From these initial observations, we have also observed that HSCs regulate the osteoblastic secretion of IL-6, macrophage inflammatory protein-1α (MIP-1α), and other factors, possibly to direct the formation of a suitable microenvironment for HSC engraftment.33 Osteoblasts also express soluble factors that cannot be detected in the absence of HSCs, again possibly to keep HSCs quiescent.37 The data strongly suggest that osteoblasts may be intimately involved in regulating hematopoietic cell proliferation and survival in vitro. Because osteoblasts and hematopoietic cells are closely associated with each other in the bone marrow, those data also suggest that there is a high likelihood that osteoblasts modulate normal hematopoiesis in vivo. These and other findings strongly suggest a reciprocal relationship between osteoblasts and hematopoietic cells, but the dimension of this interaction has yet to be completely defined (Figure 1).
What is the role of osteoblasts in the creation of a hematopoietic stem-cell niche?
In adults, the formed elements of the blood are produced in the bone marrow. The development of the bone marrow cavity is a coordinated process in which blood precursors migrate and colonize spaces carved out of embryonic bone and cartilage. Thus, an intimate physical association between bone cells and blood cells is established early in life. Several animal models strongly implicate osteoblasts in hematopoiesis by virtue of creating a niche. Among the most interesting, are studies of Cbfa1 or Runx-2, a transcription factor of the runt domain gene family. Cbfa1-deficient mice lack intramembranous and endochondral bone formation because of a maturational arrest of osteoblasts. Homozygous Runx-2–/– animals are dwarfed, are unable to breathe, and die immediately after birth.38,39 The lack of osteoblastic maturation also results in a total lack of bone marrow throughout the entire skeleton. In Runx-2–/– embryos, the number of hematopoietic precursors in the yolk sac at embryonic day 10.5 (E10.5) and in the liver at E12.5 are normal. Runx-2 does not have significant effects on the ontogeny of definitive hematopoietic cells in yolk sac and liver.40 Even as late as E17.5, no significant changes in hematopoietic populations are noted. Just before birth, however, the animals developed excessive extramedullary hematopoiesis in the livers and spleens and large hematopoietic foci in the periportal area. Mature granulocytes are also increased in the livers and spleens of Runx-2–/– embryos on E18.5, along with immature hematopoietic cells in the peripheral blood.40 Similarly, mice deficient in core-binding factor β (Cbfb, or polyomavirus enhancer binding protein 2β[Pebp2b]) die at approximately E11.5 to E13.5 because of an absence of fetal liver hematopoiesis and because of hemorrhage in the central nervous system.41-43 Cbfb plays an essential role in Runx-2–dependent skeletal development by enhancing the DNA binding of Runx-2 and Runx-2–dependent transcriptional activation. As expected, the animals also have poorly developed marrow cavities.44 When Cbfb is introduced into Cbfb–/– animals driven by the Gata1 hematopoietic promoter, the rescued animals exhibit normal fetal liver hematopoiesis and survive until birth. They do, however, show severely delayed bone formation.44
Deguchi et al40 noted that the extramedullary hematopoiesis phenotype observed in the Runx-2–deficient mice is significantly different from the extramedullary hematopoiesis that occurs secondarily to the congenital lack of osteoclasts observed in the osteopetrosis in young Op/Op mice,45,46 c-Fos–deficient mice,47 c-Src–deficient mice,48 and the double-mutant Hck and Src mice.49 Thus, the migration of hematopoietic precursors is apparently perturbed by a lack of bone marrow cavity in Runx-2–/– embryos at a time when the hematopoietic precursors should have migrated to the bone marrow. As do these findings, skeleto-hematopoietic perturbations result from alterations in the condensation/hypertrophy of cartilage precursors. For example, deletion of collagen X or Vegf results in a phenotype in which the animals are unable to replace hypertrophic cartilage by normal mechanisms.50,51 In the collagen X deletion animals, the unsuccessful establishment of the marrow in bone leads to hematopoietic changes, including altered B- or T-cell profiles.50,51 In the absence of VEGF, the animals also exhibit a similar phenotype.52,53 Partly as a result of the essential role of VEGF in the recruitment of vascular precursors required for blood vessel invasion of the bone analog and chondrocyte apoptosis, there are likely direct effects on HSCs themselves.52,53 Thus, with the disruption of VEGF expression, not only do defects in bone length and an expansion of the hypertrophic chondrocyte zone occur, the establishment of a marrow cavity to support the migration of the incoming HSCs is interrupted.52
The creation of a bone marrow cavity carved out of embryonic bone and cartilage is necessary for the establishment of medullary hematopoiesis, but the creation of a cavity may in and of itself be insufficient for the establishment of definitive hematopoiesis in bone. Although the basic helix-loop-helix oncoprotein stem cell leukemia (SCL)/tal-1 (TEL) is required for the formation of all hematopoietic lineages and for the establishment of marrow in bone, it appears to function through a mechanism different from that of Runx-2, collagen X, and Vegf deletions.54,55 TEL is an ets-related factor translocated in a variety of leukemias, and it is necessary for the normal transition of hematopoietic activity from the fetal liver to bone marrow.54,55 Deletion of Tel also results in the absence of medullary hematopoietic activity. However, the mechanism by which Tel–/– HSCs or progenitors fail to migrate or home to the bone marrow or to respond to or survive in the bone marrow microenvironment is unclear. These effects appear to be independent of vascular invasion probably residing, though perhaps not exclusively, in the hematopoietic compartment itself.17
These findings are similar to findings in animals in which stromal derived factor-1 (SDF-1) or its receptor, CXCR4, are deleted, though it is also likely that SDF-1 plays a role in vascular recruitment. SDF-1 and CXCR4 appear to be critical molecular determinants for the establishment of the marrow in bone.56,57 Gene deletion of either of these proteins results in normal fetal liver hematopoiesis, but marrow engraftment by hematopoietic cells is not observed.57-59 In addition, the overexpression of CXCR4 by human hematopoietic progenitor cells and other blood cells enhances, whereas anti-CXCR4 antibodies inhibit, marrow engraftment in nude mice.59 Typical of molecules that regulate cell trafficking, SDF-1 and its receptor have dynamic and complementary expression patterns during organogenesis.60 We recently demonstrated that osteoblasts and marrow endothelial cells express SDF-1 to localize human hematopoietic progenitor cells into the marrow.59,61,62 In the bone marrow, SDF-1 is constitutively produced by osteoblasts, fibroblasts, and endothelial cells. Osteoblast-produced SDF-1 may be a mechanism for the selective attraction of circulating osteoclast precursors to bone and their migration within marrow to appropriate perivascular stromal sites for RANKL differentiation into resorptive osteoclasts.63 Given that the creation of the marrow is likely to require the coordinated action of osteoblasts and osteoclastic precursors, the absence of osteoblasts producing SDF-1 or hematopoietic cells expressing CXCR4 could limit osteoclast, and subsequent HSC, recruitment to the marrow cavity.
A more direct approach regarding the role of osteoblasts in establishing an HSC niche came in 1995 with the development of a transgenic animal in which the osteoblast-specific promoter osteocalcin drove the expression of diphtheria toxin.64 The transgenic mice were growth-retarded and developed osteopenia with decreased numbers of osteoblasts. Although their number was apparently normal, osteoclast precursors failed to induce tartrate-resistant acid phosphate (TRAP) activity. These results suggest that osteoclasts are regulated by osteoblasts, which express receptors for local and systemic factors that regulate bone resorption.13 However, the results also suggest that osteoblasts are unnecessary for the formation of osteoclasts but are required for inducing terminal differentiation of some, but not all, osteoclastic lineage markers. Later, transgenic mice bearing a fusion gene composed of a 1.3-kilobase (kb) fragment of the mouse osteocalcin gene 2 (Og2) promoter to express the herpes simplex virus thymidine kinase (Hsv-Tk) gene were generated.65 The osteoblast-specific gene promoter Og2 is used by fully mature osteoblasts but not by osteoblastic progenitor cells. Elimination of dividing osteocalcin+ osteoblasts expressing Hsv-Tk after treatment with ganciclovir (GCV) permitted the authors to determine whether the loss of osteoblast cells influenced bone resorption. In the presence of GCV, the mice developed inducible, but reversible, osteopenia. Functional analyses of the animals showed that in the absence of bone formation, bone resorption continued at a normal rate that could be prevented with antiresorptive agents. The authors also stated that no other hematopoietic defects, including osteoclast formation or activity, were observed.65 The study established that neither bone formation nor bone mass directly controls the extent of bone resorption in vivo but suggested that osteoblasts have only a limited role, if any, in supporting hematopoiesis.
Other reports have addressed the relationship between osteoblasts and hematopoiesis by using a tissue-targeted transgenic expression of the Hsv-Tk approach to conditionally deplete osteoblast populations.66 Here the thymidine kinase expression was put under control of a 2.3-kb type 1 collagen a1 (Col1a1) promoter fragment. This promoter, like the osteocalcin promoter, has restricted activity in differentiated osteoblasts but is expressed earlier than is the osteocalcin promoter used previously.65 Eight-week-old mice bearing the Col2.3Tk transgene treated with GCV showed extensive ablation of all osteoblasts, a reduction in bone marrow cellularity, and a marked decrease in number of osteoclasts. In marrow, an early reduction in B cells and erythroid progenitors was observed as early as 8 days after GCV treatment. These effects were coupled with a progressive loss of cells with an HSC phenotype in the bone marrow, which ultimately should have led to the death of the mice from hematologic failure. However, the animals survived because of the establishment of an active extramedullary hematopoietic process. The mechanisms regulating this switch to extramedullary hematopoiesis remain to be defined. Extramedullary hematopoiesis, along with an increase in peripheral blood HSCs, was observed in spleens and livers. Withdrawal of the drug results in an exaggerated osteogenic response, with hematopoietic marrow reestablishing itself within the confines of the marrow.67 These findings suggest that the contribution of the osteoblast to the maintenance of other cellular components of the bone marrow is dependent on the level of maturation of the osteoblast lineage.68
Most recently 3 papers, 2 of which appeared simultaneously in Nature, reported the identification of a hematopoietic stem cell niche.69-71 These reports suggest that osteoblasts are critical regulators of hematopoiesis.72 In the first, Zhang et al,69 while examining the roles of the bone morphogenic protein (BMP) signaling pathway in regulating adult HSC development, found that mutant mice with conditional inactivation of BMP receptor type IA (BMPRIA) had nearly twice the number of HSCs of wild-type mice. Fractionation studies determined that only the number of the most primitive long-term HSC (LT-HSC) repopulating cells was altered.69 This finding suggested that a local effect, one that might have been caused by an alteration in the cellular niche supporting LT-HSCs, had occurred. The authors subsequently evaluated a variety of markers to demonstrate that HSCs are attached to “spindle-shaped osteoblasts” lining the inner bone surface. Colocalization histologic analyses of the distribution of the N-cadherin+ osteoblastic cells revealed a similar distribution pattern of LT-HSCs, where N-cadherin was asymmetrically localized to the cell surfaces of LT-HSCs. In the second paper, Calvi et al70 studied the signal transduction of the PTH receptor. Overexpression of its receptor enhanced osteoblastic growth but also increased the number of HSCs in the marrow. Here the increase in LT-HSC populations matched closely with enhanced Notch-1 signaling in HSCs, probably because of the enhanced expression of Jagged-1 receptors on osteoblasts. In vitro cultured bone marrow cells from mutant animals were better able to support HSCs than similar populations derived from wild-type animals, likely because of an expansion of osteoblasts. Treating healthy animals with an anabolic regime of PTH similarly expanded the HSC population in the marrows, again because of the expansion of osteoblast precursors. Administering PTH to wild-type animals before HSC transplantation markedly improved survival. Although the mechanism here remains unclear, an expansion of osteoblast numbers, and hence of the number of available stem cell–supportive niches, is implied.
The third paper implicated Tie2 in the development of the stem cell niche. This study built on the finding that Tie1 and Tie2 receptors are not required for fetal hematopoiesis or for the emergence of definitive HSCs but are required to home to the bone marrow.73 It was also observed that Ang-1 promotes the adhesion of Tie2+ stem cells to fibronectin and collagen and that osteoblasts express Ang-1 and maintain HSCs in vitro. Tie2 was, therefore, a likely candidate for localizing stem cells to the stem cell niche.71 From these observations, Arai et al71 demonstrated that Ang-1 expressed by osteoblasts activates Tie2 on the stem cells and promotes tight adhesion of stem cells to their niche. Presumably this adhesion results in HSC quiescence and survival, resulting in stem cell maintenance and self-renewal.71 This paper, along with the papers of Calvi et al70 and Zhang et al,69 demonstrates that stem cell behavior is influenced by other cells that form the microenvironment74 or niche proposed in 1978 by Schofield.75
What is the role of adhesion in whatever functions osteoblasts have? What molecules mediate HSC-OB adhesion?
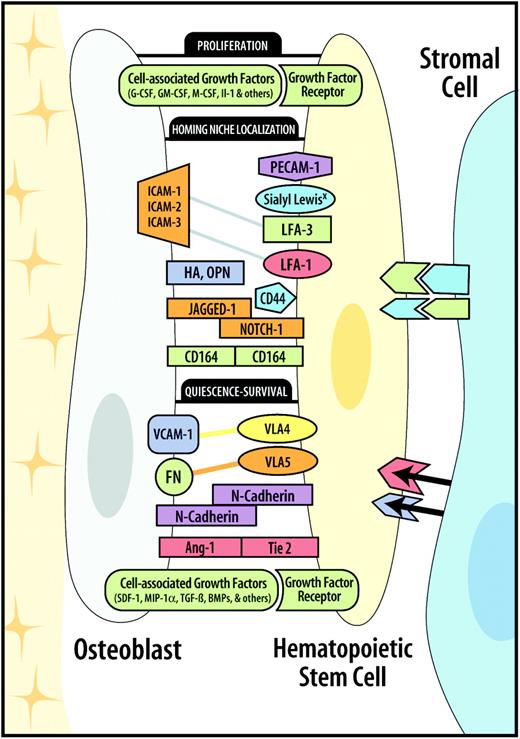
Part of the affiliation between HSCs and endosteal osteoblasts may be a consequence of cell-cell adhesion. In fact, we have observed that HSCs bind tightly to osteoblasts in vitro.76 Osteoblasts express many cell adhesion molecules that may be used during HSC-osteoblast (HSC-OB) adhesions. By far the molecules best characterized to mediate HSC-stromal cell adhesions are VLA-4 (α4β1) receptors expressed on CD34+ cells and vascular cell adhesion molecule-1 (VCAM-1) expressed by BMSCs (Figure 3).77-81 However, other interactions are known, including CD34, CD44, CD164, intracellular cell adhesion molecule-1 (ICAM-1), ICAM-3, lymphocyte function–associated antigen-1 (LFA-1), LFA-3, platelet endothelial cell adhesion molecule-1 (PECAM-1), very late antigen-4 (VLA-4), and VLA-5.82 Furthermore, cell-associated or matrix-bound cytokines, including IL-3, FLT ligand, GM-CSF, stem cell factor (SCF), and TGF-α1, may themselves serve as adhesion molecules.83-86
Model of HSC-OB adhesion-ligand pairs. The homing and tethering of HSCs to the osteoblast–stem cell niche is a rapid and reversible process because HSCs can be released through changes in receptor activation/expression, shedding, or enzymatic cleavage. The mechanisms regulating this 2-way movement of HSCs are beginning to be elucidated. Molecules involved in this regulation include cell-associated growth factors and adhesion molecules. Cell-associated growth factors are known to induce the quiescence or survival, proliferation, and niche localization of HSCs. Similarly, adhesion molecules may be functionally divided into those that localize HSCs to their niches and those that, once engaged, regulate G0 quiescence and survival.
Model of HSC-OB adhesion-ligand pairs. The homing and tethering of HSCs to the osteoblast–stem cell niche is a rapid and reversible process because HSCs can be released through changes in receptor activation/expression, shedding, or enzymatic cleavage. The mechanisms regulating this 2-way movement of HSCs are beginning to be elucidated. Molecules involved in this regulation include cell-associated growth factors and adhesion molecules. Cell-associated growth factors are known to induce the quiescence or survival, proliferation, and niche localization of HSCs. Similarly, adhesion molecules may be functionally divided into those that localize HSCs to their niches and those that, once engaged, regulate G0 quiescence and survival.
How HSCs localize to the endosteal surface remains unclear. It is known that osteoclasts express the vitronectin receptor (αvβ3 integrin) and that this receptor binds to many proteins that are abundant in bone.87 The adhesion of tumor-infiltrating lymphocytes to osteoblasts has been reported to involve LFA-1 and VLA-4.88,89 However, recent reports suggest that N-cadherin, Tie2, and Jagged-1 molecules may be important molecules in the process (detailed in “What is the role of osteoblasts in the creation of a hematopoietic stem-cell niche?”).69-71 Clearly, however, other molecules must be involved, in that the expression of these molecules is likely to be widespread throughout the marrow. Recently, our laboratory has demonstrated that the survival of HSCs in coculture with osteoblasts requires intimate cell-cell contact.76 This suggests that the osteoblast-derived factors that support stem cell activities are produced in small quantities, are rapidly turned over, may be membrane anchored, or may require the engagement of cell-cell adhesion molecules that are yet to be determined. In recent work we demonstrated that the adhesion between stem cells and osteoblasts is mediated by cell-cell rather than cell-matrix contact and is sensitive to trypsin and calcium chelators. Moreover, 2 separate types of adhesive relationships seem to exist. First, there are those that are established immediately on binding. These likely localize stem cells to the osteoblast-supported niche. Here it was observed that rapidly processed N-linked glycosylated proteins constitutively expressed on hematopoietic cells, as detected using selective pretreatment with glycosylation inhibitors, are likely involved.76 In addition, immediately after the establishment of initial contact, osteoblasts are likely to up-regulate cell adhesion molecules rich in sialic acid that limit blood cell adhesion. When these charged terminal ends are lost from the cell surface, either by digestion or by the loss or complex sugar supports, the core cell adhesion molecules on the cell surfaces of the osteoblasts convert from a low-binding form to one that binds CD34+ hematopoietic progenitors to much higher levels.76 The identity of this molecule remains to be determined.
As to the second type of adhesive relationship, we found that the survival of hematopoietic progenitor cells on osteoblasts depends on the engagement of VLA-4 (α4β1) and VLA-5 (α5β1) receptors by using function-blocking antibodies (Figure 1) (R.S.T., manuscript submitted). Surprisingly, cell-cell contact was not absolutely required to support progenitor activity, but receptor-ligand engagement of the VLA-4 and LFA-1 complexes is required. To some extent, recombinant ligands (fibronectin, ICAM-1, VCAM-1) can substitute for direct cell-cell interactions. Moreover, once these receptors were engaged, conditioned medium derived from HSCs grown on osteoblasts supported significantly greater hematopoietic progenitors in vitro than did osteoblast-conditioned or HSC-conditioned medium alone. Here, too, these molecules are unknown but are likely to include those already described, and perhaps they represent novel activities.
What is the role of osteoblasts in transplantation?
Several years ago, a novel method to track individual cells as they lodge in the bone marrow of nonablated recipients was reported.90,91 Using this method, the spatial distribution of various hematopoietic progenitor cells in bone marrow subpopulations in the femur after intravenous infusion was determined. Transplantations of different bone marrow subpopulations demonstrated that once the cells entered the marrow from the central marrow vessels, their subsequent localization within the bone marrow varied according to phenotype. HSC-enriched populations selectively lodged in the endosteal region (Figure 1). In contrast, lineage-committed hematopoietic cells redistributed away from the endosteal region in favor of the central marrow region.90,91 These results further demonstrate that the distribution of transplanted hematopoietic cells within the bone marrow is not random.
Other data that strongly suggest a significant role for osteoblasts in the development/regulation of a hematopoietic marrow are those of several recent reports suggesting that osteoblasts exert immunomodulatory activities during HSC transplantation. For example, lineage-depleted hematopoietic progenitor cells can engraft in lethally irradiated mice when transplanted within, but not across, the major histocompatibility complex (MHC) antigen barriers. El-Badri et al92 hypothesized that progenitor cell preparation required “supportive” cells/factors for successful engraftment across fully allergenic MHC barriers. Osteoblasts, purified from donor murine long bones, were cotransplanted with marrow stem cells into fully allogeneic mouse strains. Mice that underwent transplantation demonstrated excellent long-term survival, were free of disease, and received cells entirely engrafted of donor origin displaying full reconstitution of lymphohematopoietic elements. The authors concluded that bone progenitor cells or osteoblasts may represent an essential component of the stromal cell population that facilitates engraftment of marrow stem cells in an allogeneic environment. Although few reports demonstrate the successful transplantation of bone marrow stromal/mesenchymal cell elements after conventional bone marrow transplantation, engraftment may occur by the direct transplantation of donor cells into bone93 or by the insertion of bone fragments into the peritoneal cavity.94,95 Significant success in the ability to replace the BMSC component in 5 patients with different life-threatening diseases was recently demonstrated. The procedure used a heterogeneous transplantation approach comprised of transplanting bone fragments placed intraperitoneally and directly into bone along with cultured osteoblastlike cells and fully matched marrow grafts.96,97 The protocol included marrow infusion in which 2 biopsy cores obtained from the donors' iliac crests were inserted intraperitoneally and 2 were inserted directly into each recipient's iliac crest on day 0 of the transplantation procedure. Two bone fragments from each donor were used to culture osteoblastlike cells that were subsequently given by intravenous infusion on day +13. At 1 year, significant improvement of clinical parameters was reported for each patient, with adherent cell chimerism ranging from 25% to 100%, as detected by polymerase chain reaction (PCR). This method of using the transplantation of bone fragments and cultured stromal cells from bone appears to have made possible the successful engraftment of donor stem/stromal cells.
Yet how osteoblasts are able to facilitate these events is unclear. Older data show that osteoblasts can present antigen98 and, based on phenotype, may even function as dendritic cells.99 Other reports of sheep and humans using the cotransplantation of umbilical or bone marrow–derived CD34+ cells, along with cultured BMSC cells, have also resulted in significantly higher engraftment levels after transplantation than was observed after transplantation of the hematopoietic cells alone.100 These results do not appear to be dependent on the successful engraftment of stromal cells into the bone marrow, nor does the homing of CD34+ cells appear to be affected by cotransplantation. Yet recent interest in mesenchymal stem cells (MSCs) has focused on the potential use of these cells for therapeutic intervention in a variety of nonmarrow and marrow settings, including the treatment of cardiac infarction and muscle regeneration and a number of metabolic disorders. The homing of MSCs to the marrow during transplantation, which could prove important for the treatment of a number of clinical conditions, probably does occur but at a low rate. Nilsson et al91 have shown that whole marrow grafts may contain sufficient numbers of cells to engraft with the ability to become competent osteoblasts, which produce bone matrix in the presence or absence of myeloablative conditioning. Because MSCs are pluripotent cells that differentiate into a variety of cells, including bone, cartilage, adipose tissue, marrow stroma, and muscle, understanding their roles in transplantation and osteoblast production is becoming increasingly important for a number of clinical settings, including HSC transplantation.
Conclusions and future directions
In spite of the voids in our knowledge, there are now substantial reasons to suspect that osteoblast adhesion molecules play a central role in hematopoietic development in vivo, as do soluble and cell-associated factors. From the studies described, osteoblasts are clearly in a biologically relevant site to transmit information to the developing hematopoietic lineages (Figure 1). In all probability, the hematopoietic activity of osteoblasts helps to define and regulate the hematopoietic stem cell niche. By further identifying the function of osteoblasts with regard to hematopoiesis, we will undoubtedly gain significant insight into the functional relationships of this complex tissue. It remains to be determined what the functional consequences of the proximity of HSCs to osteoblasts are and what, if any, differences these findings make for transplant recipients. Critical questions remain: why do medullary cavities in bone become the normal site for definitive hematopoiesis? What are the distinct differences between how osteoblasts and other nonmedullary sites support stem cells? What is the operational structure of the bone marrow microenvironment? How do osteoblasts and other nonosteoblastic accessory stromal cells interact to regulate normal hematopoiesis, and are these structures/functions altered in leukemia? Do all osteoblasts share the same capacity to support hematopoiesis, or is the creation of the stem cell niche a transient state differing in location and maturation of osteoblasts? Do osteoblasts provide HSC proliferative or commitment control exclusively? What role do the HSCs themselves play in establishing an inductive microenvironment? Does a common bone marrow progenitor give rise to osteoblasts and hematopoietic cells postnatally, and, if so, can similar strategies be used in HSC transplantation to support osteoblastic engraftment? Versions of these questions, first proposed by Patt and Maloney in 1976,7 demonstrate how far we have come and how much further we have to go to fully understand the function of the stem cell niche. In the future, the answers to these questions will provide important tools for study of the early stages of hematopoietic stem cell engraftment and of the long-term outcome of transplantation. To understand the regulation of stem cell renewal, it is critical to determine how the diverse signals resulting from the stem cell niche are regulated and how they maintain the stem cell state.
Prepublished online as Blood First Edition Paper, December 7, 2004; DOI 10.1182/blood-2004-06-2480.
Supported by a grant (DEO13701) from the National Institutes of Health.
I would like to thank members of my laboratory, Dr Paul Krebsbach, Dr S. G. Emerson, and several unnamed reviewers for their help.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal