Abstract
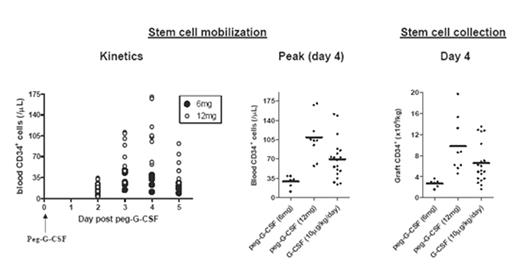
The mobilization of stem cells with pegylated-G-CSF (peg-G-CSF) modulates regulatory T cell and NKT cell function, separating graft-versus-host disease (GVHD) and graft-versus-leukemia (GVL) effects in animal models. We have initiated a phase I/II study to analyse the feasibility of mobilizing stem cells from sibling donors with peg-G-CSF and their ability to restore hematopoiesis in HLA matched transplant recipients who have received myeloablative conditioning. Results were compared to a cohort of donors mobilized with standard G-CSF at 10ug/kg/day (n=19). The administration of 6mg of peg-G-CSF (n=6) resulted in suboptimal stem cell mobilization with a peak peripheral blood CD34+ count of 29 ± 4/uL. Apheresis 4 days after peg-G-CSF administration yielded 2.7 ± 0.3 x106 CD34+ cells/kg recipient ideal body weight and all patients required a second collection on day 5 to yield a total of 4.0 ± 0.5 x106 CD34+ cells/kg recipient weight. Following escalation of the dose to 12mg (n=9), the peak CD34+ count was 109 ± 13/uL and all donors collected sufficient stem cells for transplantation in a single apheresis (9.8 ± 1.7 x106 CD34+ cells/kg recipient weight). The 6mg dose of peg-G-CSF was significantly inferior to standard G-CSF for stem cell mobilization (P<0.01) while the 12mg dose was at least equivalent (P=0.07).
Bone pain was similar between the 6mg and 12mg cohorts and to that seen with standard G-CSF. However, in addition to the expected rises in serum ALP and LDH, transient rises in hepatic transaminases were noted 5 to 12 days after peg-G-CSF administration in 7 of 9 donors receiving the 12mg dose. One donor developed NCI grade 3 hepatic toxicity and splenomegaly. After allogeneic transplantation of peg-G-CSF mobilized grafts (Cy/TBI conditioning in 13 of 14 recipients), median neutrophil and platelet engraftment occurred on days 18 and 14 respectively and was identical to that seen with grafts mobilized by standard G-CSF. With a median follow up of 165 days (range 55–532), the incidence of grade II-IV and grade III/IV acute GVHD is 50% and 21% respectively. No patients have relapsed to date and overall survival is 86%. The mobilization of stem cells with peg-G-CSF in normal donors is feasible and 12mg appears the optimal dose. Further data are required to more closely analyse the effect of peg-G-CSF on donor liver function and the ability of stem cell grafts to separate GVHD and GVL effects.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal