Abstract
We have selectively depleted host-reactive donor T cells from peripheral blood stem cell (PBSC) transplant allografts ex vivo using an anti-CD25 immunotoxin. We report a clinical trial to decrease graft-versus-host disease (GVHD) in elderly patients receiving selectively depleted PBSC transplants from HLA-identical sibling donors. Sixteen patients (median age, 65 years [range, 51-73 years]), with advanced hematologic malignancies underwent transplantation following reduced-intensity conditioning with fludarabine and either cyclophosphamide (n = 5), melphalan (n = 5), or busulfan (n = 6). Cyclosporine was used as sole GVHD prophylaxis. The allograft contained a median of 4.5 × 106 CD34 cells/kg (range, 3.4-7.3 × 106 CD34 cells/kg) and 1.0 × 108/kg (range, 0.2-1.5 × 108/kg) selectively depleted T cells. Fifteen patients achieved sustained engraftment. The helper T-lymphocyte precursor (HTLp) frequency assay demonstrated successful (mean, 5-fold) depletion of host-reactive donor T cells, with conservation of third-party response in 9 of 11 cases tested. Actuarial rates of acute GVHD were 46% ± 13% for grades II to IV and 12% ± 8% for grades III to IV. These results suggest that allodepletion of donor cells ex vivo is clinically feasible in older patients and may reduce the rate of severe acute GVHD. Further studies with selectively depleted transplants to evaluate graft-versus-leukemia (GVL) and survival are warranted.
Introduction
Graft-versus-host disease (GVHD) remains one of the most frequent and severe complications of allogeneic stem cell transplantation (SCT). Following SCT between HLA-identical pairs, minor histocompatibility antigen (mHA) disparities and especially female donor responses to recipient Y chromosome–derived antigens can cause lethal GVHD. Nevertheless, the allograft can confer a powerful graft-versus-leukemia (GVL) response, as illustrated by the success of donor lymphocyte infusions to treat leukemic relapse after transplantation.1 The GVL effect is closely but not inseparably linked with the development of GVHD.2,3 The occurrence of GVL without evidence of GVHD in some patients indicates that, at least clinically, GVHD is separable from GVL. Further support for this comes from in vitro studies demonstrating that T cells, at the clonal level, can preferentially recognize either ubiquitous (GVHD) alloantigens or leukemia-restricted (GVL) antigens.4,5
Although there has been a general trend to reduce transplantation-related mortality in the past 2 decades, there has been no clear reduction in disease relapse, which still surpasses 50% in high-risk patients. Harnessing the GVL effect and separating it from GVHD reactions remain, therefore, an important goal for improving transplantation success. While removal of most donor T lymphocytes from the graft prior to transplantation effectively prevents severe GVHD, the impairment in immune function predisposes the recipient to disease relapse, graft rejection, and posttransplantation infections. A better approach would be to selectively remove the T cells responsible for mediating GVHD, while conserving cells mediating GVL and antimicrobial immune responses. If effective, such a strategy could be used to enhance GVL by eliminating the need for immunosuppressive agents to prevent GVHD and by permitting the safe transfusion of large numbers of GVL-reactive, GVHD-nonreactive lymphocytes.
We and others have achieved the goal of separating GVHD from GVL effects in vitro by coincubating donor lymphocytes with host allogeneic stimulator cells. Under these conditions, alloreactive donor cells can be selectively identified by their surface phenotype (ie, CD25, CD69), proliferative potential, or preferential retention of photoactive dyes, and can be subsequently targeted for elimination using an immunotoxin,6,7 immunomagnetic bead separation,8-11 fluorescence-activated cell sorting,12-14 or photodynamic purging.15,16 Using standard proliferation assays, such as the mixed lymphocyte reaction (MLR) and the helper T-lymphocyte precursor (HTLp) frequency assay, we have shown that alloreactivity can be substantially depleted in both the HLA-mismatched17 and HLA-matched setting,18 while maintaining third-party responses. Responder cells obtained after allodepletion also maintain antitumor19-21 and antiviral activity.22-24 This promising approach has been validated in a number of centers in animal models,25-29 and results of a trial in haploidentical peripheral blood stem cell transplantation (PBSCT) in pediatric patients suggest that the concept is feasible.30,31
Encouraged by these preliminary findings, we tested the hypothesis that selective depletion (SD) of donor lymphocytes from the transplant ex vivo can reduce the risk of clinically significant GVHD. We chose to use expanded T lymphocytes from the recipient as the stimulator cells because of the ease of obtaining sufficient numbers of stimulators potentially free of myeloid and B-cell–derived antigens that might later induce a GVL effect.24 In this study, we investigated the SD approach in a cohort of older patients with hematologic malignancies who had HLA-identical sibling donors and received reduced-intensity conditioning and cyclosporine alone for GVHD prophylaxis. Earlier experience at our institution demonstrated that with this regimen, cyclosporine alone provided insufficient GVHD control following unmanipulated PBSCT, and resulted in significant morbidity and mortality in patients older than 50 years.32 Using SD to remove alloreactive donor lymphocytes from the transplant, we aimed to reduce GVHD while conserving beneficial donor immune function. Here we report clinical outcomes of SD transplantation in 16 patients (median age, 65 years) with advanced hematologic malignancies.
Patients and methods
Study population
Between November 2001 and June 2004, 16 patients (12 male, 4 female) 51 to 73 (median, 65) years of age with advanced hematologic malignancies and an HLA-identical sibling donor were treated under an NHLBI (National Heart, Lung, and Blood Institute) institutional review board–approved protocol (01-H-0162). Informed consent was provided by patients and donors according to the Declaration of Helsinki. Analysis was based on data available as of December 2004. Table 1 outlines the demographics of the patients and the transplantation procedure. For comparison, a historical control group of older patients with hematologic malignancies and an HLA-identical sibling donor were also evaluated (n = 17). These patients all underwent an unmanipulated PBSCT at our institution following reduced-intensity conditioning and cyclosporine monotherapy as GVHD prophylaxis.
Demographics of the patients (n = 16)
. | Value . |
|---|---|
| Transplantation date | 11/01-06/04 |
| Sex, no | M, 12; F, 4 |
| Age, y (range) | 65 (52-73) |
| Disease, no. | |
| High-risk MDS | 9 |
| Refractory AML | 4 |
| AL-CR2 | 2 |
| Resistant NHL | 1 |
| Preparative regimen, no. | |
| Flu/Cy | 5 |
| Flu/Mel | 5 |
| Flu/Bu | 6 |
| F-to-M transplanations, no. | 11 |
| CMV+ recipients, no. | 14 |
| Graft (range) | |
| CD34 dose, × 106/kg | 4.5 (3.4-7.3) |
| CD3 dose, × 108/kg | 1.0 (0.2-1.5) |
| Engraftment, d | |
| ANC more than 500/μL (range) | 13 (10-22) |
| Graft rejection (time) | 1 (day +24) |
| Day +30 donor chimerism, % (range) | |
| T cell | 100 (14-100) |
| Myeloid | 100 (4-100) |
. | Value . |
|---|---|
| Transplantation date | 11/01-06/04 |
| Sex, no | M, 12; F, 4 |
| Age, y (range) | 65 (52-73) |
| Disease, no. | |
| High-risk MDS | 9 |
| Refractory AML | 4 |
| AL-CR2 | 2 |
| Resistant NHL | 1 |
| Preparative regimen, no. | |
| Flu/Cy | 5 |
| Flu/Mel | 5 |
| Flu/Bu | 6 |
| F-to-M transplanations, no. | 11 |
| CMV+ recipients, no. | 14 |
| Graft (range) | |
| CD34 dose, × 106/kg | 4.5 (3.4-7.3) |
| CD3 dose, × 108/kg | 1.0 (0.2-1.5) |
| Engraftment, d | |
| ANC more than 500/μL (range) | 13 (10-22) |
| Graft rejection (time) | 1 (day +24) |
| Day +30 donor chimerism, % (range) | |
| T cell | 100 (14-100) |
| Myeloid | 100 (4-100) |
MDS indicates myelodysplastic syndrome; AML, acute myelogenous leukemia; AL, acute leukemia; CR, complete remission; NHL, non-Hodgkin lymphoma; Flu, fludarabine; Cy, cyclophosphamide; Mel, melphalan; Bu, busulfan; and ANC, absolute neutrophil count.
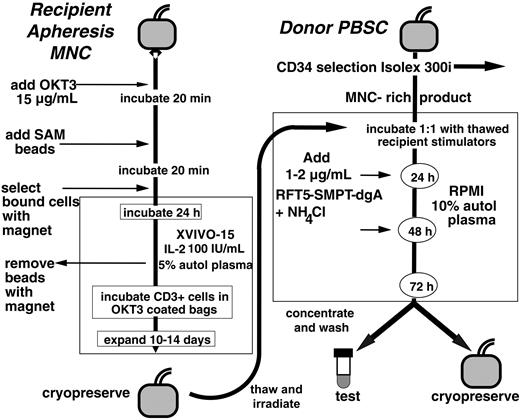
Process schema for generation of selectively depleted (SD) donor lymphocytes. Starting with recipient peripheral blood mononuclear cells collected by leukapheresis, CD3+ lymphocytes were immunomagnetically selected with OKT3 and sheep antimouse (SAM) beads and expanded to generate a stimulator T-cell population of high purity. The unadsorbed donor mononuclear cell (MNC)–rich fraction (responders) from CD34+ selection of G-CSF–mobilized PBSCs was cocultured with irradiated, expanded recipient CD3+ T lymphocytes (stimulators), and then subjected to 2 cycles of selective depletion with the anti-CD25 immunotoxin (RFT5-SMPT-dgA) before harvest of the final SD cells.
Process schema for generation of selectively depleted (SD) donor lymphocytes. Starting with recipient peripheral blood mononuclear cells collected by leukapheresis, CD3+ lymphocytes were immunomagnetically selected with OKT3 and sheep antimouse (SAM) beads and expanded to generate a stimulator T-cell population of high purity. The unadsorbed donor mononuclear cell (MNC)–rich fraction (responders) from CD34+ selection of G-CSF–mobilized PBSCs was cocultured with irradiated, expanded recipient CD3+ T lymphocytes (stimulators), and then subjected to 2 cycles of selective depletion with the anti-CD25 immunotoxin (RFT5-SMPT-dgA) before harvest of the final SD cells.
Preparative regimen
All patients received a preparative regimen consisting of fludarabine (125-180 mg/m2) and one of the following alkylating agents: cyclophosphamide (120 mg/kg), melphalan (140 mg/m2), or infusional busulfan (6.4 mg/kg).
Peripheral blood stem cell (PBSC) collection and processing
Selective depletion was performed as previously described24 (Figure 1). Donors received granulocyte colony-stimulating factor (G-CSF) 10 μg/kg per day subcutaneously. Mobilized PBSCs were collected by leukapheresis on day 5, and again on days 6 and 7 if necessary, to obtain a target dose of at least 3 × 106 CD34+ cells/kg. The Isolex 300i immunomagnetic system (version 2.5; Baxter Healthcare, Vienna, Austria) was used to perform a combined positive CD34+ cell selection and negative selection of T cells, according to the manufacturer's instructions, which results in a PBSC product with approximately 5 logs of T-cell depletion (residual T-cell doses were 0.1-1.5 × 105 CD3 cells/kg recipient weight). The PBSC product was washed, concentrated, and cryopreserved.
The unadsorbed, T-cell–rich fraction remaining after CD34 selection was the source of donor lymphocytes for the SD procedure. Recipient stimulator cells were generated from immunomagnetically selected and expanded T lymphocytes as previously described.24 Stimulator cells were thawed, gamma irradiated (2500 cGy), and added to responder cells at a ratio of 1:1 to a final concentration of 5 × 106 cells/mL. Responder and irradiated stimulator cells were cocultured for 72 hours at 37°C in 7% CO2. Alloreactive responder cells expressing the activation marker CD25 were targeted by the addition of the immunotoxin RFT5-SMPT-dgA, which consists of the anti-CD25 murine monoclonal antibody (MAb) RFT5 (immunoglobulin G1 [IgG1]) coupled to the deglycosylated ricin A chain (dgA) (prepared at University of Texas Southwestern Medical Center, Dallas, TX) via the heterobifunctional cross-linker 4-succinimidyl-oxycarbonyl-α-methyl-α-(2-pyridyldithio-toluene) (SMPT) (Pierce, Rock-ford, IL). RFT5-SMPT-dgA was added to the culture at 24 (2 μg/mL) and 48 (1 μg/mL) hours, along with the enhancing agent, ammonium chloride (10 mM; Sigma, St Louis, MO). At the completion of the 72-hour coculture, cells were harvested and cryopreserved. On day 0 following the preparative regimen, the PBSC and SD products were consecutively thawed and infused (Figure 1).
Posttransplantation management
Patients received cyclosporine alone for GVHD prophylaxis starting on day -5. In the absence of acute GVHD, immunosuppression was tapered off by day +100. Patients with disease progression or donor T-cell chimerism of less than 100% following withdrawal of immunosuppression received unmanipulated donor lymphocytes (DLIs) at 4-week or longer intervals until 100% donor T-cell chimerism and/or disease regression was achieved. No unmanipulated DLIs were administered prior to day +100 after transplantation. An SD DLI at a dose of 1 × 107 CD3+ cells/kg was cryopreserved for patients requiring DLI prior to day +100. All patients received fluconazole for antifungal prophylaxis, valacyclovir for antiviral prophylaxis, and trimethoprim/sulfamethoxazole for pneumocystis prophylaxis. Blood was tested weekly for cytomegalovirus (CMV) phosphoprotein 65 (pp65) antigen until day +100, and ganciclovir was initiated when there was evidence of CMV reactivation. Acute GVHD was treated with high-dose corticosteroids (1-2 mg/kg per day) and tapered according to response. Chronic GVHD was treated with low-dose prednisone (10-30 mg/d) and cyclosporine, daily or on alternate days.
Determination of donor-recipient chimerism
A quantitative polymerase chain reaction (PCR)–based analysis of short tandem repeats (STRs) was used to measure donor-recipient chimerism separately in lymphoid and myeloid lineages.33 DNA was extracted from donor and pretransplantation patient blood samples, and PCR using fluorescent primer sets flanking 8 different STRs and amelogenin was performed using the manufacturer's conditions (Powerplex 1.2; Promega, Madison, WI) to identify an informative allele. Ficoll-hypaque–fractionated mononuclear cells were collected on posttransplantation days +14, +30, +60, and +100 and sorted into CD14+/CD15+ myeloid and CD3+ T cells using immunomagnetic beads (Dynal, Oslo, Norway). DNA was extracted and lineage-specific chimerism was performed by PCR using fluorescent primers flanking a single STR previously identified as polymorphic between the patient and donor. Predetermined mixtures of pretransplantation patient and donor DNA were run in conjunction with test samples as quantitative controls (sensitivity for minor populations, 2%-3%). The PCR products were analyzed with a 310 ABI PRISM sequencer with the chimerism percentage determined by comparing the ratio of donor and patients DNA bands (Genescan software; both from PE Applied Biosystems, Foster City, CA).
HTLp frequency assay
The degree of alloreactivity in donor-recipient pairs was determined using the HTLp frequency assay in 11 of the 16 allografts where sufficient cellular material was available for analysis. This assay determines the frequency at limiting dilution of T-cell progenitors capable of generating an interleukin-2 (IL-2)–producing (T-helper) clone in response to a given stimulator. After a 3-day culture, any well in which a T-helper lymphocyte precursor (HTLp) has responded to the stimulator by clonal expansion contains sufficient IL-2 to be detected by its ability to stimulate proliferation and tritiated 3H-thymidine uptake in the IL-2–sensitive murine cell line 9.12 (generously provided by Dr Charles Shih, Medical College of Wisconsin). Stimulators used were either recipient-derived expanded lymphocytes or pooled third-party peripheral blood mononuclear cells (from 5 random volunteer donors). Responder cells were either G-CSF–mobilized lymphocytes, collected prior to the SD procedure, or SD lymphocytes reserved from the SD clinical product. Stimulator cells were irradiated to 50 Gy, adjusted to a concentration of 106/mL, and plated in 100 μL/well in 96-well round-bottomed microtiter plates. Responders were added in 24 replicates of 6 dilutions at concentrations of 10, 8, 6, 4, 2, and 1 × 104 cells/well for HLA-matched pairs and 4, 2, 1, 0.5, 0.25, and 0.125 × 104 cells/well for HLA-mismatched stimulators. Stimulators alone were plated in 24 replicates. Plates were incubated for 64 hours at 37°C in 5% CO2, frozen at 80°C to stop further proliferation, and then thawed. The prepared IL-2–dependent line was added at 2 × 103 cells/well in 25-μL volumes and the plates were incubated for a further 20 hours. Then 3H-thymidine was added at 1 μCi per well. Cells were harvested after 12 to 18 hours and 3H-thymidine uptake was measured. The background was defined as the mean control value plus 3 standard deviations of the 3H-thymidine uptake of the 24 control (stimulator only) wells. Test wells greater than this value were considered positive for IL-2 production. From the fraction of negative wells at each dilution, the frequency of IL-2–producing lymphocytes was calculated using the maximum likelihood method.
Statistical analysis
Summary statistics, such as proportions, means, standard deviations, medians, and ranges, were used to describe the patients' characteristics, pretransplantation variables, and posttransplantation outcomes. Standard techniques in survival analysis, including Kaplan-Meier estimates, were used to estimate the time-to-event distributions of GVHD, relapse-free survival (RFS), and relapse risk. Differences in HTLp frequency before and after SD, as well as calculation of P values, were made using the Student t test for paired samples assuming unequal variances.
Results
Patient and transplantation characteristics
Characteristics of 16 patients who underwent transplantation are summarized in Table 1. The study group was at high risk for transplant-related mortality, with a median age of 65 years (range, 51-73 years). All patients had advanced disease: 9 with high-risk myelodysplastic syndrome (MDS; excess blasts, high-risk cytogenetics, or evidence of transformation to acute leukemia); 4 with chemorefractory acute myeloid leukemia (AML); 2 with acute leukemia in second remission (AML [1], acute lymphoblastic leukemia [ALL, 1]); and 1 with a chemoresistant non-Hodgkin lymphoma. Other high-risk features included female-to-male transplantations in 11 (69%) of 16 patients, and CMV seropositivity in 14 (88%) of 16 patients.
Characteristics of the SD allograft
SD allografts were successfully generated for all patients, meeting release criteria for cell numbers, viability, and sterility. SD cells contained a broad profile of CD4+ and CD8+ T lymphocytes, B lymphocytes, natural killer (NK) cells, and monocytes, closely resembling the starting G-CSF–mobilized peripheral blood apheresis product (Table 2). Nevertheless SD lymphocytes had decreased reactivity against HLA-matched recipient-derived stimulator cells as measured by the HTLp frequency assay. Successful depletion of alloreactivity (mean, 5-fold; range, 2- to 11-fold) was observed in 9 of the 11 allografts tested by HTLp frequency, while responses against pooled third-party stimulator cells were conserved (Figure 2).
Final cellular graft composition (n = 16)
. | Stem cell product . | . | SD product . | . | . | . | . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Dose . | . | Dose . | Fraction* . | . | . | . | |||||
| Patient ID . | CD34+, × 106/kg . | CD3+, × 104/kg . | CD3+, × 108/kg . | CD4+, % . | CD8+, % . | CD56+, % . | Other cells, %† . | |||||
| 1 | 6.7 | 5.0 | 1.1 | 32.3 | 11.8 | 2.2 | 53.7 | |||||
| 2 | 3.6 | 5.0 | 0.8 | 27.3 | 12.3 | 5.8 | 54.6 | |||||
| 3 | 3.8 | 5.0 | 1.4 | 28.9 | 13.6 | 3.2 | 54.3 | |||||
| 4 | 6.1 | 5.0 | 0.7 | 16.1 | 12.0 | 2.5 | 69.4 | |||||
| 5 | 7.3 | 0.3 | 1.5 | 29.8 | 17.4 | 2.5 | 50.3 | |||||
| 6 | 4.9 | 0.2 | 1.4 | 34.0 | 20.7 | 3.4 | 41.9 | |||||
| 7 | 4.5 | 0.3 | 0.5 | 22.1 | 14.8 | 1.9 | 61.2 | |||||
| 8 | 6.9 | 0.2 | 1.0 | 16.3 | 15.3 | 1.7 | 66.7 | |||||
| 9 | 4.3 | 0.2 | 0.2 | 15.5 | 6.5 | 2.1 | 75.9 | |||||
| 10 | 3.4 | 0.2 | 1.1 | 29.8 | 10.0 | 4.3 | 55.9 | |||||
| 11 | 5.9 | 0.1 | 1.0 | 20.2 | 19.5 | 1.8 | 58.5 | |||||
| 12 | 4.5 | 0.2 | 1.4 | 32.0 | 10.2 | 8.1 | 49.7 | |||||
| 13 | 4.1 | 0.2 | 0.7 | NA | NA | 3.7 | 61.4 | |||||
| 14 | 3.8 | 0.3 | 0.7 | 31.4 | 12.1 | 1.9 | 54.6 | |||||
| 15 | 3.5 | 0.1 | 0.9 | 41.7 | 18.5 | 6.0 | 33.8 | |||||
| 16 | 4.5 | 0.1 | 1.2 | 26.9 | 8.7 | 5.0 | 59.4 | |||||
| Median | 4.5 | 0.2 | 1.0 | 28.9 | 12.3 | 2.8 | 55.3 | |||||
. | Stem cell product . | . | SD product . | . | . | . | . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Dose . | . | Dose . | Fraction* . | . | . | . | |||||
| Patient ID . | CD34+, × 106/kg . | CD3+, × 104/kg . | CD3+, × 108/kg . | CD4+, % . | CD8+, % . | CD56+, % . | Other cells, %† . | |||||
| 1 | 6.7 | 5.0 | 1.1 | 32.3 | 11.8 | 2.2 | 53.7 | |||||
| 2 | 3.6 | 5.0 | 0.8 | 27.3 | 12.3 | 5.8 | 54.6 | |||||
| 3 | 3.8 | 5.0 | 1.4 | 28.9 | 13.6 | 3.2 | 54.3 | |||||
| 4 | 6.1 | 5.0 | 0.7 | 16.1 | 12.0 | 2.5 | 69.4 | |||||
| 5 | 7.3 | 0.3 | 1.5 | 29.8 | 17.4 | 2.5 | 50.3 | |||||
| 6 | 4.9 | 0.2 | 1.4 | 34.0 | 20.7 | 3.4 | 41.9 | |||||
| 7 | 4.5 | 0.3 | 0.5 | 22.1 | 14.8 | 1.9 | 61.2 | |||||
| 8 | 6.9 | 0.2 | 1.0 | 16.3 | 15.3 | 1.7 | 66.7 | |||||
| 9 | 4.3 | 0.2 | 0.2 | 15.5 | 6.5 | 2.1 | 75.9 | |||||
| 10 | 3.4 | 0.2 | 1.1 | 29.8 | 10.0 | 4.3 | 55.9 | |||||
| 11 | 5.9 | 0.1 | 1.0 | 20.2 | 19.5 | 1.8 | 58.5 | |||||
| 12 | 4.5 | 0.2 | 1.4 | 32.0 | 10.2 | 8.1 | 49.7 | |||||
| 13 | 4.1 | 0.2 | 0.7 | NA | NA | 3.7 | 61.4 | |||||
| 14 | 3.8 | 0.3 | 0.7 | 31.4 | 12.1 | 1.9 | 54.6 | |||||
| 15 | 3.5 | 0.1 | 0.9 | 41.7 | 18.5 | 6.0 | 33.8 | |||||
| 16 | 4.5 | 0.1 | 1.2 | 26.9 | 8.7 | 5.0 | 59.4 | |||||
| Median | 4.5 | 0.2 | 1.0 | 28.9 | 12.3 | 2.8 | 55.3 | |||||
NA indicates no T-cell subpopulation was available; the total T-cell fraction was 34.9%.
Each individual cell fraction is expressed as percentage of all viable cells in the SD product
Includes granulocytes, monocytes, and B cells (not presented separately)
Hematologic recovery, engraftment, chimerism, and immune reconstitution
An absolute neutrophil count (ANC) of .5 × 109/L (500/μL) was achieved in all patients at a median of 13 days (range, 10-22 days) after transplantation. The median time to achieve an untransfused platelet count of more than 20 × 109/L was 11 days (range, 10-20 days). One patient developed secondary graft failure on day +24, requiring a second transplantation. Median donor T-cell chimerism at day +30 after transplantation was 100% (range, 14%-100%). Median donor myeloid cell chimerism at day +30 after transplantation was 100% (range, 4%-100%). On day +100 after transplantation, 8 (73%) of 11 evaluable patients had complete donor T-cell chimerism, while 9 (82%) of 11 patients had complete donor myeloid cell chimerism. Myeloid and T-cell chimerism between days +14 to +100 after transplantation are displayed in Table 3. T-cell reconstitution was measured in 8 evaluable patients on day +100, with a median absolute CD3 count of 1306/μL (range, 311-4610/μL) and a median absolute CD4 count of 392/μL (range, 113-1601/μL).
Serial donor chimerism data of all patients at 14, 30, 60, and 100 days after transplantation (n = 16)
. | Day +14 . | . | Day +30 . | . | Day +60 . | . | Day +100 . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient ID . | T, % . | M, % . | T, % . | M, % . | T, % . | M, % . | T, % . | M, % . | ||||
| 1 | 68 | 2 | 97 | 4 | 94 | 0 | 91 | 0 | ||||
| 2 | 48 | 78 | 68 | 26 | N/A | N/A | 100 | 14 | ||||
| 3 | 100 | 44 | 99 | 86 | 100 | 41 | 100 | 100 | ||||
| 4 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 5 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 6 | 91 | 100 | 97 | 100 | 93 | 100 | 99 | 100 | ||||
| 7 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 8 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 9 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 10 | 14 | 90 | 22 | 100 | 15 | 100 | 28 | 99 | ||||
| 11 | 100 | 86 | 100 | 100 | 99 | 99 | 99 | 100 | ||||
| 12 | 15 | 95 | 100 | 100 | 37 | 100 | 30 | 67 | ||||
| 13 | 27 | 100 | 82 | 100 | 94 | 100 | N/A | N/A | ||||
| 14 | 7 | 92 | 15 | 100 | 32 | 100 | 81 | 100 | ||||
| 15 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 16 | 22 | 69 | 27 | 63 | 60 | 74 | 75 | 84 | ||||
| Median | 96 | 98 | 100 | 100 | 99 | 100 | 100 | 100 | ||||
. | Day +14 . | . | Day +30 . | . | Day +60 . | . | Day +100 . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient ID . | T, % . | M, % . | T, % . | M, % . | T, % . | M, % . | T, % . | M, % . | ||||
| 1 | 68 | 2 | 97 | 4 | 94 | 0 | 91 | 0 | ||||
| 2 | 48 | 78 | 68 | 26 | N/A | N/A | 100 | 14 | ||||
| 3 | 100 | 44 | 99 | 86 | 100 | 41 | 100 | 100 | ||||
| 4 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 5 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 6 | 91 | 100 | 97 | 100 | 93 | 100 | 99 | 100 | ||||
| 7 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 8 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 9 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 10 | 14 | 90 | 22 | 100 | 15 | 100 | 28 | 99 | ||||
| 11 | 100 | 86 | 100 | 100 | 99 | 99 | 99 | 100 | ||||
| 12 | 15 | 95 | 100 | 100 | 37 | 100 | 30 | 67 | ||||
| 13 | 27 | 100 | 82 | 100 | 94 | 100 | N/A | N/A | ||||
| 14 | 7 | 92 | 15 | 100 | 32 | 100 | 81 | 100 | ||||
| 15 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | ||||
| 16 | 22 | 69 | 27 | 63 | 60 | 74 | 75 | 84 | ||||
| Median | 96 | 98 | 100 | 100 | 99 | 100 | 100 | 100 | ||||
T indicates CD3+ T cells; M, CD14+/CD15+ myeloid cells; and N/A, no data available.
Functional activity of SD lymphocytes. Donor lymphocytes from the allograft, before and after SD, were tested for alloreactivity in the HTLp frequency assay (n=11) against (A) the HLA-identical recipient stimulator cells and (B) an HLA-mismatched pooled third-party stimulator. Results are reported as the calculated frequency of alloreactive HTLp (1/x). Mean HTLp frequency for the group is indicated by gray horizontal bars (values given in graphs), and statistical significance calculated by the paired Student t test.
Functional activity of SD lymphocytes. Donor lymphocytes from the allograft, before and after SD, were tested for alloreactivity in the HTLp frequency assay (n=11) against (A) the HLA-identical recipient stimulator cells and (B) an HLA-mismatched pooled third-party stimulator. Results are reported as the calculated frequency of alloreactive HTLp (1/x). Mean HTLp frequency for the group is indicated by gray horizontal bars (values given in graphs), and statistical significance calculated by the paired Student t test.
Acute and chronic GVHD
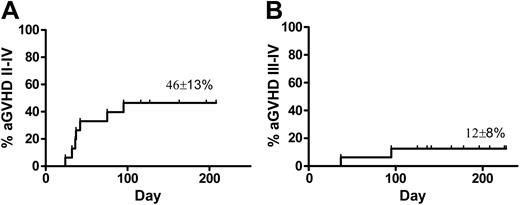
Acute GVHD occurred in 8 patients. GVHD was mild in 4 cases (skin only, grade I or II, treated with topical and/or low-dose oral steroids), moderate in 2 cases (skin + visceral involvement, grade II, responsive to intravenous steroids), and severe in 2 cases (grade III/IV, steroid refractory). One case of severe GVHD (grade IV gastrointestinal involvement) arose early after transplantation (day +37) in a patient with unsuccessful allodepletion by HTLp analysis (Table 4). The second case (grade III gastrointestinal involvement) occurred on day 80 in a patient with preexisting grade I skin GVHD, following rapid withdrawal of cyclosporine to treat early AML relapse. The actuarial rate of grades II to IV acute GVHD was 46% ± 13% (Figure 3A), while grades III to IV GVHD was observed in 12% ± 8% (Figure 3B). Two of 11 patients tested for HTLp developed acute GVHD affecting gut and requiring intravenous steroids. They had post-SD HTLp frequencies of 206 000 or lower (339/kg and 1091/kg). In the other 9 patients, HTLp frequency was reduced to between 1/384 000 to 1/1 800 000 (49 to 248/kg) (Table 4). Selective depletion efficiency as measured by HTLp frequency assay was associated with GVHD severity (Table 2). Allografts from patients with visceral GVHD (gastrointestinal and/or hepatic) demonstrated higher post-SD HTLp frequencies, compared with patients without GVHD or with mild skin-only involvement. Chronic GVHD occurred in 7 of 14 evaluable patients, 6 with limited and 1 with extensive involvement (following chemotherapy and unmanipulated DLI for relapse).
Infused alloreactive T cell dose and clinical outcome (n = 11)
Patient ID . | Disease . | HTLp (1/x) before SD . | HTLp (1/x) after SD . | SD CD3+ dose, × 108/kg . | HTLp dose/kg* . | aGVHD†grade . | aGVHD type . | aGVHD treatment‡ . | Survival status . | COD . | Survival days . | Comments . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 | NHL | 217 547 | 128 378 | 1.4 | 1091 | 2 | Gut only | High dose | D | NRM | 227 | Steroid-responsive gut and liver GVHD, died 8 months after transplantation of a myocardial infarction |
| 13 | RAEB | 141 844 | 206 625 | 0.7 | 339 | 4 | Gut, liver | High dose | D | NRM | 67 | Steroid refractory GVHD |
| 4 | RAEB-T | 166 082 | 603 994 | 0.7 | 248 | 0 | NR | NR | A | NR | 642 | Alive in CR |
| 16 | AML ref | 316 636 | 605 261 | 1.2 | 198 | 1 | Skin only | Low dose | A | 164 | Relapse day +95, developed grade III gut GVHD after abruptly stopping CSA for relapse | |
| 10 | AML ref | 122 560 | 563 013 | 1.1 | 195 | 0 | NR | NR | D | Relapse | 164 | Relapse day +100, developed extensive cGVHD following unmanipulated DLI |
| 5 | sAML (CR1) | 119 332 | 518 786 | 1.5 | 135 | 2 | Skin only | Low dose | A | NR | 550 | Alive in CR |
| 3 | RAEB | 398 085 | 1 219 886 | 1.4 | 115 | 2 | Skin only | Low dose | A | NR | 792 | Alive in CR |
| 8 | AML ref | 110 306 | 918 713 | 1.0 | 109 | 0 | NR | NR | D | Relapse | 208 | Relapse death (day +208) |
| 7 | tMDS | 69 978 | 737 977 | 0.5 | 68 | 1 | Skin only | Low dose | D | Relapse | 136 | Relapse death (day +136) |
| 9 | sAML (CR1) | 171 883 | 383 470 | 0.2 | 52 | 0 | NR | NR | A | NR | 317 | Alive in CR |
| 15 | sAML (CR1) | 163 945 | 1 850 089 | 0.9 | 49 | 0 | NR | NR | A | NR | 177 | Alive in CR |
Patient ID . | Disease . | HTLp (1/x) before SD . | HTLp (1/x) after SD . | SD CD3+ dose, × 108/kg . | HTLp dose/kg* . | aGVHD†grade . | aGVHD type . | aGVHD treatment‡ . | Survival status . | COD . | Survival days . | Comments . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 | NHL | 217 547 | 128 378 | 1.4 | 1091 | 2 | Gut only | High dose | D | NRM | 227 | Steroid-responsive gut and liver GVHD, died 8 months after transplantation of a myocardial infarction |
| 13 | RAEB | 141 844 | 206 625 | 0.7 | 339 | 4 | Gut, liver | High dose | D | NRM | 67 | Steroid refractory GVHD |
| 4 | RAEB-T | 166 082 | 603 994 | 0.7 | 248 | 0 | NR | NR | A | NR | 642 | Alive in CR |
| 16 | AML ref | 316 636 | 605 261 | 1.2 | 198 | 1 | Skin only | Low dose | A | 164 | Relapse day +95, developed grade III gut GVHD after abruptly stopping CSA for relapse | |
| 10 | AML ref | 122 560 | 563 013 | 1.1 | 195 | 0 | NR | NR | D | Relapse | 164 | Relapse day +100, developed extensive cGVHD following unmanipulated DLI |
| 5 | sAML (CR1) | 119 332 | 518 786 | 1.5 | 135 | 2 | Skin only | Low dose | A | NR | 550 | Alive in CR |
| 3 | RAEB | 398 085 | 1 219 886 | 1.4 | 115 | 2 | Skin only | Low dose | A | NR | 792 | Alive in CR |
| 8 | AML ref | 110 306 | 918 713 | 1.0 | 109 | 0 | NR | NR | D | Relapse | 208 | Relapse death (day +208) |
| 7 | tMDS | 69 978 | 737 977 | 0.5 | 68 | 1 | Skin only | Low dose | D | Relapse | 136 | Relapse death (day +136) |
| 9 | sAML (CR1) | 171 883 | 383 470 | 0.2 | 52 | 0 | NR | NR | A | NR | 317 | Alive in CR |
| 15 | sAML (CR1) | 163 945 | 1 850 089 | 0.9 | 49 | 0 | NR | NR | A | NR | 177 | Alive in CR |
HTLp indicates helper T-lymphocyte precursor; SD, selective depletion; aGVHD, acute graft-versus-host disease; COD, cause of death; D, dead; NRM, nonrelapse mortality; RAEB, refractory anemia and excess of blasts; RAEB-T, RAEB transformed; A, alive; CR, complete remission; ref, refractory; CSA, cyclosporine; cGVHD, chronic graft versus host disease; sAML, secondary AML (arising from MDS); tMDS, therapy-related MDS; and NR, not relevant.
HTLp dose/kg determined by product of CD3 dose in SD allograft per kilogram recipient weight and the frequency of alloreactive HTLp (1/x) after SD
GVHD before day +100
Low-dose treatment defined by oral steroid dose equal to 0.5 mg/kg, high-dose therapy defined by oral steroid use of more than 0.5 mg/kg or need for intravenous steroids
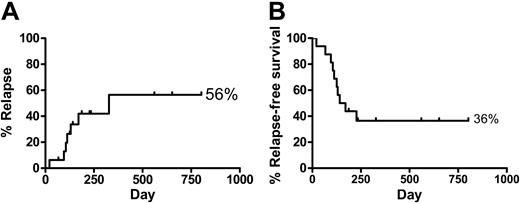
Toxicity, NRM, relapse, and relapse-free survival (RFS)
Infusion of the SD lymphocyte product did not result in any immediate adverse reactions and did not result in delayed side effects such as autoimmune or alloimmune reactions. Nonrelapse mortality (NRM) occurred in 4 patients (GVHD [1], graft failure [1], fungal pneumonia [1], and myocardial infarction after 8 months [1]), giving an actuarial risk of NRM of 6% at day +100 and 25% at 1 year. There were 5 relapse deaths in this high-risk cohort, including 3 patients who underwent transplantation with chemorefractory AML and 1 with treatment-related MDS and complex cytogenetics. The 2-year actuarial probabilities of relapse and RFS were 56% and 36%, respectively (Figure 4).
Acute GVHD. Actuarial probability of (A) grades II to IV and (B) grades III to IV GVHD in SD patients (n=16).
Acute GVHD. Actuarial probability of (A) grades II to IV and (B) grades III to IV GVHD in SD patients (n=16).
Discussion
Ex vivo SD is a strategy designed to prevent GVHD by specifically removing host-reactive donor lymphocytes while conserving useful donor immune function. This promising approach has been tested by a number of investigators in animal models and with human cells in vitro, and the results of a trial in haploidentical transplantations suggest that the concept is feasible.34,35 Given these preclinical and early clinical findings, we undertook a pilot clinical study to test the hypothesis that ex vivo SD could reduce the severity of GVHD in high-risk patients. Based on the high morbidity and mortality associated with GVHD in elderly patients undergoing a matched related donor PBSCT at our institution,32 we performed transplantations on 16 older patients (median age, 65 years) with SD allografts following reduced-intensity conditioning and compared their results with a historical cohort of older transplant recipients receiving unmanipulated allografts. Our results demonstrate that ex vivo SD of alloreactive T cells from PBSC allografts, using an anti-CD25 immunotoxin, is feasible and safe and that GVHD severity may be diminished in patients treated by this approach. Furthermore, we showed that the severity of GVHD related with the efficiency of SD, as measured by the HTLp frequency assay. Finally, unlike other methods of T-cell depletion, engraftment, GVL, and immune recovery were not adversely affected in these patients. A concern with this approach is a theoretical possibility of autoimmune phenomena including more chronic GVHD due to the probable depletion of CD4+CD25+ regulatory T cells.36-38 Currently 7 of 14 patients have developed chronic GVHD, but larger patient numbers will be required to evaluate this further.
Relapse and relapse-free survival. Actuarial probability of (A) relapse and (B) relapse-free survival in SD patients (n=16).
Relapse and relapse-free survival. Actuarial probability of (A) relapse and (B) relapse-free survival in SD patients (n=16).
The clinical-scale SD process we used was based on earlier experiments that suggested that GVL-reactive T cells were spared following SD.24,39,40 Donor lymphocytes from mobilized peripheral blood were stimulated with irradiated recipient cells, followed by the elimination of alloresponding donor cells with an immunotoxin directed against the α-chain of the IL-2 receptor (CD25). Stimulator cells from the recipient consisted of selected and expanded T lymphocytes collected by apheresis, a reliable method for obtaining sufficient numbers of nonmalignant cells for allogeneic stimulation. SD was not achieved in 2 of the 11 patients tested, due to variability in either generating or depleting CD25+ alloreactive cells. Comparison of clinical outcomes showed an association between the depletion of alloreactive T cells to HTLp frequencies approaching 1/1000 000 and absent or skin-only GVHD. While these results are preliminary, they appear to support studies on HLA-matched transplantations, suggesting that the donor versus recipient HTLp frequency must exceed a threshold of around 1/100 000 for severe GVHD to occur.41-45 Interestingly, the degree of depletion achieved did not correlate with the starting HTLp frequency (Table 4), and SD appeared to be efficient in several instances where predepletion donor alloreactive HTLp frequency was high. While further work is clearly required to make SD a more efficient and reproducible procedure, the association we found here between GVHD severity and degree of SD provides a proof of principle for the technique.
In previous studies in older patients receiving unmanipulated reduced-intensity PBSC transplants and comparable posttransplantation immunosuppression (cyclosporine alone), we encountered a 58% incidence of grades II to IV and a 34% incidence of grades III to IV GVHD that was associated with a high mortality.46 The current patient group was older and included only high-risk diseases and 11 of 16 female-into-male transplants. Nevertheless the outcome compared favorably with our previous experience. The results support the hypothesis that reduction of GVHD in reduced-intensity transplants in older patients can improve overall transplant outcome. However a therapeutic benefit of SD for GVL and survival will require further evaluation.
In conclusion, these results indicate promise for this strategy because they provide preliminary evidence of a therapeutic benefit from SD PBSCT. Nevertheless our findings now require further validation in a large patient cohort using more effective ways to deplete alloreactive lymphocytes. Our group is therefore exploring both large-scale magnetic and photodynamic depletion approaches as an alternative strategy, as recently summarized.47
Prepublished online as Blood First Edition Paper, April 7, 2005; DOI 10.1182/blood-2005-01-0393.
Supported by a grant from the Dr. Mildred Scheel Stiftung für Krebshilfe, Germany (S.M.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal