Abstract
We have studied conversion of marrow cells to skeletal muscle in cardiotoxin-injured anterior tibialis muscle in a green fluorescent protein (GFP) to C57BL/6 transplantation model and ascertained that total body irradiation (TBI) with establishment of chimerism is a critical factor. Local irradiation has little effect in lower doses and was detrimental at higher doses. Whole body (1000 cGy) with shielding of the leg or a combination of 500 cGy TBI and 500 cGy local radiations was found to give the best results. In non-obese diabetic-severe combined immunodeficient (NOD-SCID) recipients, we were able to show that conversion could occur without radiation, albeit at relatively lower levels. Within 3 days of cardiotoxin injury, GFP-positive mononuclear cells were seen in the muscle, and within 2 weeks GFP-positive muscle fibers were identified. Conversion rates were increased by increasing donor-cell dose. Timing of the cardiotoxin injury relative to the transplantation was critical. These studies show that variables in transplantation and injury are critical features of marrow-to-muscle conversions. Irradiation primarily effects conversion by promoting chimerism. These data may explain the differences in the literature for the frequency of marrow-to-skeletal muscle conversion and can set a platform for future models and perhaps clinical protocols. (Blood. 2005;106:1488-1494)
Introduction
Muscle stem-cell selection can be achieved by a variety of immunostaining or differential culture techniques. These discoveries have reinvigorated the interest in muscle transplantation and raised the hope that clinically relevant degrees of muscle replacement may be achievable in human patients with congenital muscular diseases such as muscular dystrophies. Muscle stem-cell transplantation has been performed in animal models as well as human clinical trials, but with only small percentages of muscle mass replacement. Furthermore, the cells useful for transplantation have to be obtained from the same limited supply of organ donors. This makes clinical applications difficult. Thus, it would be highly desirable to have a readily available alternate source of cells. Several recent reports have highlighted the broad developmental potential of bone marrow-derived stem cells, and the term “stem-cell plasticity” has been coined.
Bone marrow contains hematopoietic as well as mesenchymal stem cells. It has been reported that these cells not only produce all of the blood lineages but also bone,1 cartilage,2 endothelial,3,4 lung,5 hepatic,6,7 neuronal,8 cardiac,9 and skin cells,10 to cite a noninclusive list. The conversion of bone marrow-derived cells into skeletal muscle cells was first described in vitro by Wakitani et al,11 followed by reports for in vivo conversion of those cells into a dystrophin-deficient (mdx) model.12 Using a model of cardiotoxin injury and subsequent regeneration of skeletal muscle, we and other investigators were able to demonstrate that bone marrow transplantation could participate in muscle regeneration by conversion of marrow cell into muscle fibers.13-16 It has been suggested that marrow cells will differentiate into muscle satellite cells17 before fusing into existing recipient muscle cells.13 It has also been recently demonstrated that isolated single hematopoietic stem cells can convert into skeletal muscle.18,19 This suggested that the hematopoietic stem cells may indeed be plastic and be capable of producing both blood and muscle fibers. The incidence of these events, however, has remained relatively low.
Despite great enthusiasm, there is a paucity of information on the kinetics of the conversion process and experimental details that will lead to high levels of conversion. This is probably responsible for the significant differences in the literature regarding the presence and the robustness of the phenomenon. Review of the literature indicates that the process of marrow-to-muscle conversion by mere reconstitution of hematopoietic chimerism is not efficient. Therefore, detailed knowledge regarding the conversion phenomenon will be needed before any human trials can be contemplated. We have previously shown that injury is a critical factor in the process of marrow-to-muscle conversion. We have now examined the effects of radiation, cell dose, and the timing of the injury relative to radiation. The data from these experiments show that manipulating the details of transplantation can result in significant changes in the degree of marrow-to-muscle conversion which can explain differences in the results between other plasticity studies.
Materials and methods
Experimental animals
C57BL/6 (H2Kb) mice were purchased from Jackson Laboratory (Bar Harbor, ME). Mice were certified to be pathogen free, housed in our animal facility, and given ad libitum access to food and acid water. Green fluorescent protein (GFP) transgenic breeding pairs C57BL/6-TgN(ACTbEGFP)1Osb were purchased from Jackson Laboratory. Animals were bred in our animal facility by mating heterozygous GFP-positive animals to C57BL/6 for GFP transgenic animals. Heterozygote GFP animals were separated by using a UV light source.
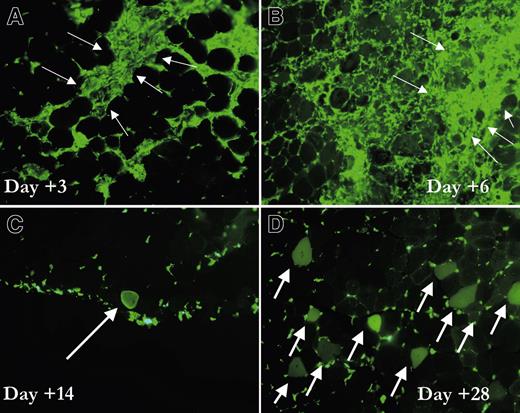
Timing of conversion of marrow cells to skeletal muscle. Digital photomicrographs of frozen sections of muscle. C57BL/6 mice that received a transplant of tibialis anterior GFP marrow were injured with cardiotoxin. (A-B) Frozen sections of the muscle 3 and 6 days after injury demonstrate a massive infiltration of hematopoietic cells in the area of injury (arrows). (C). At 2 weeks after injury, the first GFP-positive myocytes appear, and, at 4 weeks after injury (D), many GFP-positive fibers can be identified (arrows). Pictures were taken with a FITC filter. Magnification, × 20.
Timing of conversion of marrow cells to skeletal muscle. Digital photomicrographs of frozen sections of muscle. C57BL/6 mice that received a transplant of tibialis anterior GFP marrow were injured with cardiotoxin. (A-B) Frozen sections of the muscle 3 and 6 days after injury demonstrate a massive infiltration of hematopoietic cells in the area of injury (arrows). (C). At 2 weeks after injury, the first GFP-positive myocytes appear, and, at 4 weeks after injury (D), many GFP-positive fibers can be identified (arrows). Pictures were taken with a FITC filter. Magnification, × 20.
Bone marrow transplantation
Six- to 8-week-old mice were used as donors or recipients. After killing the mice and dissecting the femur, tibia, and pelvic bones, bone marrow was obtained by flushing the bones with Hanks balanced salt solution (HBSS) with 2% heat-inactivated fetal calf serum (HI-FCS) using a syringe and a 22-gauge needle. After resuspension in HBSS without fetal calf serum (FCS) with a 5-mL pipette, cells were passed through a 40-μm cell strainer. Cell numbers were counted in crystal violet, and viability was assessed by trypan blue staining. Approximately 4 hours after radiation, unselected bone marrow cells were injected intravenously by tail vein into each recipient. In most of the experiments 20 to 25 million marrow cells were infused at the time of transplantation with the exception of cell-dose experiments where a dose range between 5 and 100 million GFP-positive marrow cells were infused. A photon-producing linear accelerator (Elekta, Stockholm, Sweden) was used for radiation of animals 4 hours before each transplantation. Radiation was given at a dose rate of 85 cGy per minute.
Importance of timing of injury. After 500 cGy TBI and 500 cGy lower-extremity radiation, C57BL/6 mice received transplants of 25 million bone marrow cells. Cardiotoxin was injected intramuscularly at different time points before or after transplantation into the animal (days - 2, - 1, + 2, + 7, and + 21 relative to the day of transplantation). Animals were killed 4 weeks after the last injury, and their tibialis anterior muscles were analyzed for the presence of GFP-positive fibers. Data represents mean ± standard error from a total of 6 mice per time point from 2 separate experiments. *P < .05, compared with other time points.
Importance of timing of injury. After 500 cGy TBI and 500 cGy lower-extremity radiation, C57BL/6 mice received transplants of 25 million bone marrow cells. Cardiotoxin was injected intramuscularly at different time points before or after transplantation into the animal (days - 2, - 1, + 2, + 7, and + 21 relative to the day of transplantation). Animals were killed 4 weeks after the last injury, and their tibialis anterior muscles were analyzed for the presence of GFP-positive fibers. Data represents mean ± standard error from a total of 6 mice per time point from 2 separate experiments. *P < .05, compared with other time points.
Muscle injury
We evaluated the dose of cardiotoxin (Naja mossambica mossambica; Sigma, St Louis, MO) appropriate to induce a visible lysis of muscle fibers in 48 hours. Hematoxylin and eosin (H&E) staining of frozen sections of injected muscle showed that 10 mM cardiotoxin in 100 μL phosphate-buffered saline (PBS) will induce 80% to 90% lysis of muscle fibers in the area of injection. The left tibialis anterior muscle, either uninjected or injected with 100 μL PBS, was used as control for each experiment. Cardiotoxin diluted in 100 μL PBS was injected into the anterior tibialis muscle using a 27-gauge needle and a 1-mL syringe. Animals were first anesthetized by halothane. The needle was inserted deep into the anterior tibial muscle longitudinally toward the knee from the ankle. Cardiotoxin was injected along the length of the muscle. Left tibialis anterior muscle was used as control.
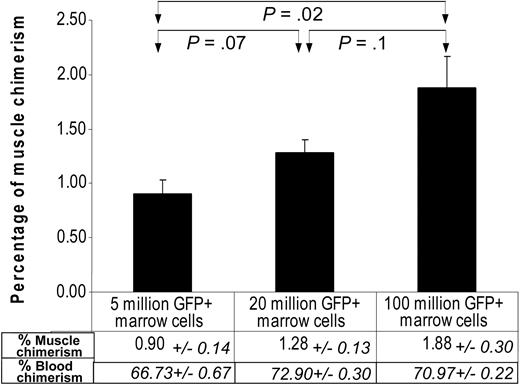
Effect of marrow-cell dose on marrow-to-muscle conversion. C57BL/6 mice underwent transplantation with 3 different doses (5, 20, and 100 million) of bone marrow cells after 900 cGy whole-body radiation. Seven days later cardiotoxin was injected into the tibialis anterior muscle. Four weeks after injury animals were killed, and muscle samples were analyzed for the incidence of GFP-positive muscle fibers. There was a graded increase in the incidence of GFP-positive muscle fibers as the doses of infused GFP marrow cells increased, whereas the level of peripheral blood chimerism changed minimally. The results represent data from a total of 6 mice per cell level from 2 separate experiments. Error bars indicate mean ± standard error.
Effect of marrow-cell dose on marrow-to-muscle conversion. C57BL/6 mice underwent transplantation with 3 different doses (5, 20, and 100 million) of bone marrow cells after 900 cGy whole-body radiation. Seven days later cardiotoxin was injected into the tibialis anterior muscle. Four weeks after injury animals were killed, and muscle samples were analyzed for the incidence of GFP-positive muscle fibers. There was a graded increase in the incidence of GFP-positive muscle fibers as the doses of infused GFP marrow cells increased, whereas the level of peripheral blood chimerism changed minimally. The results represent data from a total of 6 mice per cell level from 2 separate experiments. Error bars indicate mean ± standard error.
Immunofluorescent staining
To evaluate cells included in the regenerating muscle, specimens were collected after killing mice by cervical dislocation after halothane anesthesia. Excised muscle specimens were placed in freshly prepared PLP fixative solution (balanced phosphate solution with 2% paraformaldehyde, sodium m-periodate, and l-lysine) for 2 hours at 4°C, with frequent agitation. Samples were then washed in 7% sucrose buffer at 4°C overnight followed by 15% sucrose buffer for 2 to 3 hours and then 25% sucrose plus 10% glycerol buffer at 4°C for another 2 hours. They were then rinsed in HBSS and embedded in optimum cutting temperature compound (OCT), frozen, and stored at - 70°C until sectioning. Immunofluorescent staining was performed on 10- to 16-μm cryosections. In the case of intracellular antigens, permeabilization was performed with 0.2% Triton-X for 20 minutes. Sections were then blocked for 30 minutes with normal serum. In the case of antidystrophin antibody, mouse on mouse (MOM) kit (Vector Laboratories, Burlingame, CA) was used for blocking. Sections were then incubated with antidesmin and antidystrophin, biotinylated anti-mouse CD45, or Alexa Flour 488-conjugated anti-GFP antibodies (Molecular Probes, Eugene, OR) for 2 hours at room temperature, followed by 1-hour incubation with respective secondaries (Alexa Fluor antirabbit for desmin, rhodamine antimouse for dystrophin, and Alexa Fluor streptavidin for CD45). Either GFP expression or antigens stained by different fluorescence-conjugated antibodies were visualized under an Axioplan 2 135 fluorescence microscope (Carl Zeiss, Oberkochen, Germany). To rule out the possibility of autofluorescence mistaken for GFP, presence of a true green signal was checked by using a dual filter for fluorescein isothiocyanate (FITC) and rhodamine. Alexa Fluor 594-conjugated anti-GFP antibody was also used to confirm that the presumed GFP signals colocalized with anti-GFP antibody staining.
Images in Figures 1 and 5 were acquired using an Axiocam HR digital camera and processed with Axiovision 3 software (Zeiss, Oberkochen, Germany). The objective lens used to obtain images was a 20×/0.5 Plan-NeoFlur.
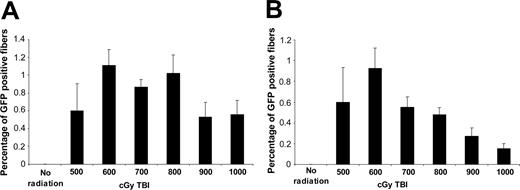
Increasing the dose of total body radiation does not increase marrow-to-muscle conversion. One month after transplantation of GFP-positive marrow cells and cardiotoxin injury of tibialis anterior muscle, the percentage of GFP-positive muscle fibers was evaluated. (A-B) Each bar shows average ± standard error from 5 to 6 animals from 2 separate experiments. (B) The percentage of GFP-positive muscle fibers were corrected for muscle weight (see “Materials and methods”).
Increasing the dose of total body radiation does not increase marrow-to-muscle conversion. One month after transplantation of GFP-positive marrow cells and cardiotoxin injury of tibialis anterior muscle, the percentage of GFP-positive muscle fibers was evaluated. (A-B) Each bar shows average ± standard error from 5 to 6 animals from 2 separate experiments. (B) The percentage of GFP-positive muscle fibers were corrected for muscle weight (see “Materials and methods”).
Flow cytometry
Blood chimerism was determined by obtaining peripheral blood from each mouse by tail vein bleeding. Blood (50 μL) was incubated for 10 minutes at room temperature with 1.5 mL ice-cold erythrocyte-lysing solution (150 mM NH4Cl, 10 mM NaHCO3, 1 mM EDTA [ethylenediaminetetraacetic acid], pH 7.4), washed with PBS, and resuspended in PBS and 1% paraformaldehyde (Sigma) and kept at 4°C until analysis. Peripheral donor chimerism was assessed by fluorescence-activated cell sorting (FACS). The percentage of GFP-positive cells was calculated by the total number of GFP-positive cells over total number of negative cells, after subtracting the background.
Cell separation
Bone marrow was isolated from iliac bones, femur, and tibiae of GFP transgenic mice 6 to 8 weeks of age. Bone marrow cells were incubated with anti-CD45-APC (allophycocyanin), anti-c-Kit APC and anti-stem-cell antigen 1 (Sca-1)-biotin (followed by streptavidin APC), all from Pharmingen (San Diego, CA), for 30 minutes. Cells positive and negative for individual markers were then sorted into different tubes with a high-speed MoFlow cell sorter. For lineage-negative separation, a low-density fraction (< 1.077 g/cm2) was isolated on Nycoprep 1.077A (Accurate Chemical and Scientific Corporation, Westbury, NY). These cells were lineage depleted using magnetic beads from Lineage Depletion Kit (Miltenyi Biotec. Auburn, CA). Cells were washed and counted after depletion, and equal numbers of lineage-positive and -negative cells were injected intravenously into the animals.
Counting and statistics
To count GFP-positive muscle fibers, at least 8 sections of 16 μm, each 200 μm apart, were made in each muscle specimen, and the number of GFP-positive muscle fiber was counted. GFP-positive muscle fibers were previously defined by our group by their characteristic morphology and double staining for antidesmin and antidystrophin antibodies.13 These fibers were negative for CD45. We also counted 3 random high-power fields (HPFs) in each section and counted the total number of HPFs for each section and then calculated a ratio between GFP-positive muscle fibers and total estimated muscle fibers (ie, average of cell number in HPFs multiplied by the number of HPFs per section). We used the nonparametric Wilcoxon rank-sum test for comparison, and the trend test developed by Cuzick for testing trend.20 The level of significance is set at .05 (2-sided). Data are presented as mean ± 1 standard error of the mean.20 Corrected percentage of muscle chimerism was calculated according to the following formula: Corrected percentage of muscle chimerism = true percentage of chimerism × (weight of the injured tibialis anterior / average weight of uninjured tibialis anterior muscle).
Results
Timeline for conversion
C57BL/6 mice received transplants of 25 million bone marrow cells after 900 cGy whole-body radiation. Seven days later cardiotoxin was injected directly into the right tibialis anterior. Animals were killed at 1, 3, 6, 14, 21, 28, and 60 days after injury, and their muscle were analyzed for GFP-positive myoblasts and muscle fibers. The first GFP-positive myocytes appeared 14 days after transplantation, and their numbers were maximized by 4 weeks (Figure 1). There was very little change in the incidence of positive fibers between 1 and 2 months after injury; therefore, 1 month after the injury time point was chosen for analysis of future experiments.
Timing of cell transplantation relative to injury
We next examined whether a particular time for cardiotoxin injury before or after transplantation influenced the percentage of marrow-derived muscle cells. C57BL/6 mice received transplants of 25 million bone marrow cells after 500 cGy whole-body and 500 cGy lower-extremity radiation (day 0). Cardiotoxin was injected intramuscularly at different time points before or after irradiation and transplanted to cohorts of animal (days - 2, - 1, + 2, + 7, and + 21 relative to the day of transplantation). Animals were killed 4 weeks after the last injury, and their tibialis anterior muscles were analyzed for the presence of GFP-positive fibers. Animals that received cardiotoxin 1 or 2 days before transplantation or 2 days after transplantation had atrophied muscle with an average weight of 28.7 ± 2.4 g. There were very few GFP-positive fibers in the animals in these groups. However, muscle fibers in the animals that received cardiotoxin 7 or 21 days after transplantation were not atrophied and had an average weight of 44.4 ± 3.17 g. They showed significantly higher percentage of GFP-positive fibers (Figure 2). This was even more significant when the results were corrected for the weight of muscle.
Dose of transplanted cells
We evaluated the effect of dose of infused marrow cells at the time of transplantation on marrow-to-muscle conversion. C57BL/6 mice were transplanted with 3 different doses (5, 20, and 100 million) of bone marrow cells after 900 cGy whole-body radiation. Radiation (900 cGy) was chosen to achieve high levels of hematopoietic conversion and to eliminate blood chimerism as a confounding factor on marrow-to-muscle conversion. Seven days after transplantation, cardiotoxin was injected into tibialis anterior muscle, and, 4 weeks after injury, animals were killed and muscle samples were analyzed for the incidence of GFP-positive muscle fibers. There was a graded increase in the incidence of GFP-positive muscle fibers as the doses of infused GFP marrow cells increased, while the level of hematopoietic chimerism reflected by percentage of donor-derived cells in peripheral blood changed minimally between the groups (Figure 3). The magnitude of increase, however, was not linear, and it showed only slightly more than a 2-fold increase between 5 × 106 and 100 × 106 dose groups where 20 times more cells were infused. The weight of the muscles remains similar between the groups.
Local radiation is not a critical factor in marrow-to-muscle chimerism. C57BL/6 animals underwent transplantation with GFP-positive marrow cells from transgenic mice after 500 or 1000 cGy local, systemic, or systemic radiation with shielding of the right leg followed by injection of cardiotoxin intramuscularly. (A-B) The percentage of GFP-positive fibers in the right tibialis anterior muscle is shown. Each bar shows average ± standard error from 5 to 6 animals from 2 separate experiments. *P < .05 between the groups. (C) The results of panels A and B are corrected for the average weight of muscles. (D-F) Photomicrographs of frozen sections of the tibialis anterior muscle in animals that received 1000 cGy local radiation (D), 1000 cGy TBI (E), or 1000 cGy TBI with shielding of the lower extremity (F). Arrows point to the GFP-positive muscle fibers.
Local radiation is not a critical factor in marrow-to-muscle chimerism. C57BL/6 animals underwent transplantation with GFP-positive marrow cells from transgenic mice after 500 or 1000 cGy local, systemic, or systemic radiation with shielding of the right leg followed by injection of cardiotoxin intramuscularly. (A-B) The percentage of GFP-positive fibers in the right tibialis anterior muscle is shown. Each bar shows average ± standard error from 5 to 6 animals from 2 separate experiments. *P < .05 between the groups. (C) The results of panels A and B are corrected for the average weight of muscles. (D-F) Photomicrographs of frozen sections of the tibialis anterior muscle in animals that received 1000 cGy local radiation (D), 1000 cGy TBI (E), or 1000 cGy TBI with shielding of the lower extremity (F). Arrows point to the GFP-positive muscle fibers.
Radiation dose
We have previously shown that radiation is critical in the marrow-to-muscle conversion phenomenon, and in the absence of radiation no GFP-positive muscle fibers were identified.13 We have now conducted a series of experiments to find the optimal dose of radiation and to explore the role of local or systemic radiation. C57BL/6 mice received transplants of 25 million GFP-positive marrow cells from transgenic mice after levels of whole-body radiation varying from 0 to 1000 cGy. One week later, the anterior tibialis muscles were injured by injection of cardiotoxin directly into the muscle. Analysis was performed 1 month after injury by calculating the percentage of GFP-positive fibers to the total number of fibers. Animals that had zero radiation did not have any GFP-positive muscle fibers, but doses from 500 cGy up to 1000 cGy radiation resulted in significant increase in the incidence of GFP-positive muscle fibers (Figure 4A; Table 1). However, the difference between the number of GFP-positive cells in the cohort that received between 500 and 1000 cGy radiation was not statically significant (Figure 4A). Despite the presence of GFP-positive fibers, higher doses of radiation were detrimental to muscle regeneration, and there was a significant atrophy of regenerating muscles especially in doses of 900 to 1000cGy TBI in C57BL/6 recipients. The lack of regeneration was clearly demonstrated by the lack of central nuclei in the remaining muscles. Because of the significant atrophy in higher doses of radiation, we corrected the percentage of GFP-positive muscle fibers in individual tibialis anterior muscles for the degree of the atrophy (see “Materials and methods”). The results show that there is now a significant stepwise decrease of GFP-positive fibers as the dose of radiation increases from 500 to 600 cGy up to 1000 cGy (Figure 4B).
Percentage of peripheral blood chimerism and muscle weight of the tibialis anterior at time of analysis
. | . | TBI . | . | . | . | . | . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
. | No radiation . | 500 cGy . | 600 cGy . | 700 cGy . | 800 cGy . | 900 cGy . | 1000 cGy . | |||||
| Peripheral blood chimerism, % | 0.00 | 50.6 ± 2.0 | 54.0 ± 2.0 | 61.4 ± 3.1 | 65.0 ± 1.4 | 59.6 ± 1.9 | 74.1 ± 0.8 | |||||
| Muscle weight* | 75.9 ± 5.3 | 63.4 ± 7.9 | 61.8 ± 2.9 | 46.8 ± 4.0 | 38 ± 3.4 | 38.2 ± 2.9 | 27 ± 5.0 | |||||
. | . | TBI . | . | . | . | . | . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
. | No radiation . | 500 cGy . | 600 cGy . | 700 cGy . | 800 cGy . | 900 cGy . | 1000 cGy . | |||||
| Peripheral blood chimerism, % | 0.00 | 50.6 ± 2.0 | 54.0 ± 2.0 | 61.4 ± 3.1 | 65.0 ± 1.4 | 59.6 ± 1.9 | 74.1 ± 0.8 | |||||
| Muscle weight* | 75.9 ± 5.3 | 63.4 ± 7.9 | 61.8 ± 2.9 | 46.8 ± 4.0 | 38 ± 3.4 | 38.2 ± 2.9 | 27 ± 5.0 | |||||
Gram ± standard error.
Effect(s) of local versus systemic radiation
The effects of radiation on the incidence of GFP-positive muscle fibers can be explained by either the local effect of radiation on muscle or a systemic effect of radiation. Therefore, extending the data presented in Figure 4, we tested whether the same doses of local or systemic radiation produce similar muscle chimerism levels. Animals received 0, 500 cGy, or 1000 cGy radiation to their right lower extremities with shielding of the rest of the body. Their tibialis anterior muscles were injured 7 days later by injection of cardiotoxin. The incidence of GFP-positive muscle fibers was determined 1 month after injury, and the results were compared with the animals that received the same levels of systemic radiation. Rare GFP-positive cells were seen at 500cGy and 1000 cGy local radiation. In contrast with the local radiation, the incidences of GFP muscle fibers were higher in both groups of 500 cGy and 1000 cGy whole-body radiation (Figure 5A-B; Table 2). To further dissect the effect of local versus systemic radiation, animals were exposed to whole-body radiation while their right lower extremities were shielded from radiation. Analysis of the samples demonstrated that shielding of the leg in the lower dose of radiation (500 cGy) did not affect the incidence of GFP-positive muscle fiber and in the higher levels significantly improved marrow-to-muscle conversion (Figure 5A-B). In the group that received 1000 cGy TBI, shielding of the leg prevented muscle atrophy. It was of interest that the combination of 500 cGy whole-body and 500 cGy lower-extremity radiation resulted in minimal atrophy and many GFP fibers (Figure 6; Table 3) and gave similar results to those seen in mice that received 1000 cGy and had limb shielding. In general the percentage of hematopoietic chimerism correlated with the incidence of muscle fiber chimerism (Figure 5; Table 2).
Peripheral blood hematopoietic chimerism of GFP-positive cells, 1 month after transplantation with different doses of radiation
. | . | Local radiation . | . | TBI . | . | TBI with shielding of legs . | . | |||
|---|---|---|---|---|---|---|---|---|---|---|
. | No radiation . | 500 cGy . | 1000 cGy . | 500 cGy . | 1000 cGy . | 500 cGy . | 1000 cGy . | |||
| Peripheral blood chimerism, % | 0.0 | 0.5 ± 0.0 | 3.3 ± 1.7 | 50.6 ± 2.8 | 74.1 ± 0.8 | 19.2 ± 3.2 | 51.0 ± 0.7 | |||
| Muscle weight* | 75.9 ± 5.3 | 77.6 ± 6.4 | 53 ± 4.8 | 63.4 ± 7.9 | 27 ± 5.0 | 81.5 ± 4.5 | 57.4 ± 4.3 | |||
. | . | Local radiation . | . | TBI . | . | TBI with shielding of legs . | . | |||
|---|---|---|---|---|---|---|---|---|---|---|
. | No radiation . | 500 cGy . | 1000 cGy . | 500 cGy . | 1000 cGy . | 500 cGy . | 1000 cGy . | |||
| Peripheral blood chimerism, % | 0.0 | 0.5 ± 0.0 | 3.3 ± 1.7 | 50.6 ± 2.8 | 74.1 ± 0.8 | 19.2 ± 3.2 | 51.0 ± 0.7 | |||
| Muscle weight* | 75.9 ± 5.3 | 77.6 ± 6.4 | 53 ± 4.8 | 63.4 ± 7.9 | 27 ± 5.0 | 81.5 ± 4.5 | 57.4 ± 4.3 | |||
Gram ± standard error.
Peripheral blood GFP chimerism and the weight of injured tibialis anterior muscles in each group
. | No radiation . | 500 cGy TBI . | 600 cGy TBI . | 700 cGy TBI . | 800 cGy TBI . | 900 cGy TBI . | 1000 cGy TBI . | 500 local radiation and 500 cGy TBI . | 1000 cGy TBI and shielding of legs . |
|---|---|---|---|---|---|---|---|---|---|
| Peripheral blood chimerism, % | 0.00 | 50.6 ± 2.0 | 54.0 ± 2.0 | 60.4 ± 3.1 | 65.0 ± 1.4 | 59.6 ± 1.9 | 74.1 ± 0.8 | 58.6 ± 6.4 | 51.0 ± 0.7 |
| Muscle weight* | 75.9 ± 5.3 | 63.4 ± 7.9 | 61.8 ± 2.9 | 46.8 ± 4.0 | 38 ± 3.4 | 38.2 ± 2.9 | 27 ± 5.0 | 68 ± 6.7 | 57.4 ± 4.3 |
. | No radiation . | 500 cGy TBI . | 600 cGy TBI . | 700 cGy TBI . | 800 cGy TBI . | 900 cGy TBI . | 1000 cGy TBI . | 500 local radiation and 500 cGy TBI . | 1000 cGy TBI and shielding of legs . |
|---|---|---|---|---|---|---|---|---|---|
| Peripheral blood chimerism, % | 0.00 | 50.6 ± 2.0 | 54.0 ± 2.0 | 60.4 ± 3.1 | 65.0 ± 1.4 | 59.6 ± 1.9 | 74.1 ± 0.8 | 58.6 ± 6.4 | 51.0 ± 0.7 |
| Muscle weight* | 75.9 ± 5.3 | 63.4 ± 7.9 | 61.8 ± 2.9 | 46.8 ± 4.0 | 38 ± 3.4 | 38.2 ± 2.9 | 27 ± 5.0 | 68 ± 6.7 | 57.4 ± 4.3 |
Gram ± standard error.
The best dose of radiation for marrow-to-muscle conversion. The pooled result is shown for corrected conversion percentage of marrow-to-muscle fibers based on muscle weight after different doses or combination of radiation. Each bar shows average ± standard error from 5 to 6 animals from 2 separate experiments. *P < .05, comparing these 2 groups with the group that received 1000 cGy TBI.
The best dose of radiation for marrow-to-muscle conversion. The pooled result is shown for corrected conversion percentage of marrow-to-muscle fibers based on muscle weight after different doses or combination of radiation. Each bar shows average ± standard error from 5 to 6 animals from 2 separate experiments. *P < .05, comparing these 2 groups with the group that received 1000 cGy TBI.
Hematopoietic versus muscle chimerism
We have previously shown that engraftment of up to 100 million GFP-positive marrow cells into nonirradiated C57BL/6 mice followed by cardiotoxin injury resulted in minimal if any GFP-positive muscle fibers. Analysis of the peripheral blood of these animals demonstrated less than 1% GFP-positive cells (data are not shown). Furthermore, multiple references in the past have demonstrated that GFP is immunogenic.21-23 Both antibody and cytotoxic responses to the GFP after transplantation of GFP-positive bone marrow cells have been demonstrated.21 An immune response to expressed GFP might explain the failure to achieve engraftment, in nonirradiated transplants, both in hematopoietic and in skeletal muscle. To test this hypothesis we used a NOD/SCID model in which immunologic reactivity is not present. NOD/SCID mice received transplants of lineage-negative GFP-positive bone marrow cells. Lineage-negative cells were chosen to avoid graft-versus-host effect that is seen in this transplantation model. Tibialis anterior muscles were injured with cardiotoxin 7 days after transplantation. One month later, in contrast with transplants in the nonirradiated immunocompetent recipients, injured muscle showed significant numbers of GFP-positive muscle fibers. As expected there was also hematopoietic chimerism demonstrated by peripheral blood analysis. Adding either local or systemic radiation to the transplantation protocol resulted in the improvement in the incidence of GFP-positive muscle fiber but at the expense of increasing atrophy of the regenerated muscles (Figure 7). We observed that the sensitivity to radiation was species specific; that is, only 350 cGy TBI in NOD/SCID mice resulted in significant atrophy. These data demonstrate that marrow can convert to muscle without any irradiation when immunologic barriers are removed and in the presence of blood chimerism.
Radiation is not essential for marrow-to-muscle conversion. Male NOD/SCID mice received transplants of 12 million GFP lineage-negative, GFP-positive marrow cells from transgenic mice after different doses of lower-extremity and/or whole-body radiation. One week later, anterior tibialis muscles were injured with injection of cardiotoxin directly into the muscle. Analyses were performed 1 month after injury by calculating the percentage of GFP-positive fibers to the total number of fibers. Charts represent the average for peripheral blood chimerism of GFP-positive cells, weight of right tibialis anterior muscle, the percentage of muscle GFP-positive fibers, and the percentage of muscle GFP-positive fibers corrected for their weight, in each group. In this model of regeneration, at higher doses of local or systemic radiation, peripheral blood and muscle chimerism increases but the muscle weight decreases. Three mice in each group were evaluated. Error bars indicate mean ± standard error.
Radiation is not essential for marrow-to-muscle conversion. Male NOD/SCID mice received transplants of 12 million GFP lineage-negative, GFP-positive marrow cells from transgenic mice after different doses of lower-extremity and/or whole-body radiation. One week later, anterior tibialis muscles were injured with injection of cardiotoxin directly into the muscle. Analyses were performed 1 month after injury by calculating the percentage of GFP-positive fibers to the total number of fibers. Charts represent the average for peripheral blood chimerism of GFP-positive cells, weight of right tibialis anterior muscle, the percentage of muscle GFP-positive fibers, and the percentage of muscle GFP-positive fibers corrected for their weight, in each group. In this model of regeneration, at higher doses of local or systemic radiation, peripheral blood and muscle chimerism increases but the muscle weight decreases. Three mice in each group were evaluated. Error bars indicate mean ± standard error.
Cells with stem-cell characteristics are responsible for marrow-to-muscle conversion
The type of the cells responsible for marrow-to-muscle conversion is not clear. Whole bone marrow contains heterogeneous populations of cells, such as hematopoietic stem cells and mesenchymal stem cells. Recently, it has been claimed that mesenchymal cells have the in vivo capability of differentiating into muscle fibers. Furthermore, it is always difficult to exclude contamination of the transplanted cells with rare mesenchymal stem cells. To address this question we separated bone marrow cells based on their surface markers and were infused intravenously by tail vein injection after radiation. Tibialis anterior muscles were injected with cardiotoxin 7 days after transplantation, and they were analyzed for the presence of GFP-positive fibers 4 weeks later. Figure 8 demonstrates the results of these experiments and shows that most of the marrow-to-muscle conversion occurs in groups with high hematopoietic stem-cell potential such as CD45+, Lineage-, Sca+, or c-Kit+ populations. Equal numbers of positive and negative cells were injected for each population. GFP-positive muscle fibers were found only in CD45+ and c-Kit+ populations, compared with CD45- and c-Kit- groups, which mostly excludes mesenchymal stem cells as the cell type responsible for this phenomenon.
GFP-positive muscle fibers are from stem-cell populations of marrow cells. Different populations of marrow cells were infused into C57BL/6 mice after 500 cGy whole-body and 500 cGy lower-extremity radiation. Animals received cardiotoxin injury to their right tibialis anterior muscle 1 week after transplantation, and their muscles were analyzed for the presence of GFP-positive muscle fibers. The numbers of cells injected for whole bone marrow (WBM) were 3 × 106 cells; CD45- and CD45+, 2 × 106 cells; Lineage- and Lineage+, 1.4 × 106 cells; c-Kit+ and c-Kit-, 2.16 × 106 cells; and Sca-1+ and Sca-1-, 8 × 105 cells each. Data represent average ± SE from 3 to 6 animals in each group. All the differences between the positive and negative groups in each population were statistically significant (P < .05). Error bars indicate mean ± standard error.
GFP-positive muscle fibers are from stem-cell populations of marrow cells. Different populations of marrow cells were infused into C57BL/6 mice after 500 cGy whole-body and 500 cGy lower-extremity radiation. Animals received cardiotoxin injury to their right tibialis anterior muscle 1 week after transplantation, and their muscles were analyzed for the presence of GFP-positive muscle fibers. The numbers of cells injected for whole bone marrow (WBM) were 3 × 106 cells; CD45- and CD45+, 2 × 106 cells; Lineage- and Lineage+, 1.4 × 106 cells; c-Kit+ and c-Kit-, 2.16 × 106 cells; and Sca-1+ and Sca-1-, 8 × 105 cells each. Data represent average ± SE from 3 to 6 animals in each group. All the differences between the positive and negative groups in each population were statistically significant (P < .05). Error bars indicate mean ± standard error.
Discussion
Recently, there has been excitement about the potential of bone marrow-derived cells to differentiate to nonhematopoietic cells, a phenomenon that could be used for the treatment of a variety of human diseases. One of the targeted diseases is muscular dystrophy. In animal models, it has been shown that phenotypic correction of about 20% of myofibers could ameliorate the pathologic features of congenital muscle disorders.24,25 Unfortunately, most of the current literature on marrow-to-muscle plasticity has reported very low levels of conversion (from < 1% to a maximum of 3%). We have been able to achieve higher levels of marrow-derived muscle chimerism (up to 12%) after intramuscular injection of lineage-negative marrow cells in regenerating muscle of animals previously given transplants of GFP marrow.13 We further demonstrated that radiation and injury were both critical for such a high conversion rate.13 This illustrates the importance of details of transplantation in the incidence of marrow-to-muscle conversion. In this study, we have now addressed several other critical aspects of marrow-to-muscle conversion. These aspects include the role of timing of injury relative to transplantation, the effect of cell dose, the types of cells involved in the process, the kinetics of muscle conversion, the immunologic effect of GFP, and the role of systemic and/or local radiation. We have shown that lack of attention to any of these details would result in significant changes in outcome of the experiments and critical misinterpretation of the whole phenomenon. We have focused on the role of radiation, the relative importance of local irradiation versus systemic irradiation, and the effect of hematopoietic chimerism, showing that marrow-to-muscle conversion can be obtained without irradiation when immunologic barriers (GFP immunoresponse) are eliminated.
We have demonstrated the kinetics of marrow-to-muscle conversion, showing the presence of GFP-positive fibers by 2 weeks and a plateau in the incidence of these fibers by 4 weeks. The delayed appearance of GFP-positive muscle fibers supports the work by LaBarge and Blau,17 showing the transition of marrow cells into satellite cells without any fusion before their inclusion in muscle fibers. The resulting satellite cells then fuse to other myoblasts or to existing muscle fibers.
We have documented that cell dose is important with increasing number of transplanted marrow cells resulting in increasing GFP-positive fibers. It is of interest that this was not linear, suggesting the presence of an interaction between different marrow cell populations and possibly to endogenous muscle-regenerating cells.
Timing relative to injury is also important and may relate partly to the degree of perturbance in the regenerating environment with regard to a radiation and cardiotoxin injection interaction. Tibialis anterior muscles that were injected immediately before or after radiation all showed significant atrophy. Marrow cells may need to home to the skeletal muscle first and before injury to be able to participate in regeneration. However, it has been suggested that marrow cells may need to transit through the bone marrow environment and then be recruited to the injured muscle.26
In our studies, irradiation influences marrow to skeletal muscle fiber conversion by establishing chimerism and not by local effects. There is a progressive increase in atrophy with increasing radiation doses from 500 to 1000 cGy, and the studies comparing 500 cGy TBI plus 500 cGy local radiation showed much less atrophy than 1000 cGy TBI even though the muscles received the same total dose of irradiation. This suggests that higher systemic doses of radiation increased muscle atrophy through long-range mechanisms such as cytokine effects. The presence of atrophy is not surprising, since a high dose of radiation is known to damage satellite cells and to prevent regeneration. It may also affect the microenvironment of the muscle that is important for stimulation of myoblasts and repair of the damaged muscle. In such an abnormal environment bone marrow cells may not have the opportunity to differentiate to myoblasts. Since the ultimate goal of these and other similar experiments are to increase the percentage of marrow-derived muscle fibers for future clinical application, presence of muscle atrophy would have a negative outcome. Therefore, we presented the percentage of GFP-positive fibers in both a raw form and a form corrected for muscle weight. The percentage of the GFP-positive fibers were corrected for muscle weight since the few GFP-positive fibers in an atrophied muscle would have given us a skewed high percentage of GFP positivity, suggesting incorrectly that higher doses of radiation may have a similar or even better outcome.
In this model, radiation at 1000 cGy of whole body with shielding of the legs or radiation at 500 cGy of whole body and 500 cGy of the lower extremity consistently resulted in the highest number of conversion events with the least amount of atrophy, allowing us the choice to use either model for our future experiments. It is puzzling that the 500 cGy TBI and 500 cGy local radiation resulted in minimal atrophy, although the total radiation to the limb was 1000 cGy. This result remains unexplained and may be due to an abscopal effect of higher doses of whole-body radiation, possibly cytokine related on muscle regeneration.
Whole bone marrow is a very heterogenous population. The 2 predominant cell types in the marrow are hematopoietic and stromal cells. In this study we have shown that only lineage-, CD45+, c-Kit+, and Sca-1+ cells, that are typical hematopoietic stem cells, comprise the population with skeletal muscle conversion potential. This indicates that under the conditions of our experiments, mesenchymal stem cells, which are generally CD45- and c-Kit-, are probably not the origin of marrow-derived GFP muscle fiber.
These results in addition to our previous work13 indicate that there are multiple variables involved in the conversion of marrow cells to muscle fibers and demonstrate the growing complexity of optimization for marrow-to-muscle conversion (Table 4). These data indicate that the most efficient model for obtaining higher levels of conversion involves either 1000 cGy TBI with shielding of the lower leg or 500 cGy local radiation and 500 cGy TBI followed by marrow engraftment with injury delayed to 1 week after cell infusion. Higher cell levels clearly improve results. Attention to these details will be critical for obtaining robust levels of muscle-cell formation from marrow. By applying some of these variables we have obtained up to 12% conversion. The future key to an optimum conversion rate may be the appropriate combination of these variables.
Proposed critical variable in marrow-to-muscle conversion
Factor . | Effects . |
|---|---|
| Presence of injury | Minimal conversion without any injury.13 |
| Mobilization | Type and the number of mobilization cycles are important.13 |
| Timing of cell delivery from injury | Injection of cells after injury increase the conversion rate. |
| Cell dose | Increasing the number of the transplanted cells improves the conversion but a plateau may exist. |
| Systemic irradiation with hematopoietic chimerism | Lower doses are beneficial and higher doses are detrimental. |
| Local irradiation | Minimal improvement if any. |
| Typ of transplanted cell | Lineage negative cells and cKit positive and Sca-1 cells are enriched for cells producing GFP + skeletal muscles. |
| Mode of cell delivery | Direct cell delivery by percutaneous injection improves the outcome.13 |
| Cell tracking system/immune status of host | Immunologic reaction to GFP may decrease the conversion because of immunologic rejection. |
Factor . | Effects . |
|---|---|
| Presence of injury | Minimal conversion without any injury.13 |
| Mobilization | Type and the number of mobilization cycles are important.13 |
| Timing of cell delivery from injury | Injection of cells after injury increase the conversion rate. |
| Cell dose | Increasing the number of the transplanted cells improves the conversion but a plateau may exist. |
| Systemic irradiation with hematopoietic chimerism | Lower doses are beneficial and higher doses are detrimental. |
| Local irradiation | Minimal improvement if any. |
| Typ of transplanted cell | Lineage negative cells and cKit positive and Sca-1 cells are enriched for cells producing GFP + skeletal muscles. |
| Mode of cell delivery | Direct cell delivery by percutaneous injection improves the outcome.13 |
| Cell tracking system/immune status of host | Immunologic reaction to GFP may decrease the conversion because of immunologic rejection. |
Prepublished online as Blood First Edition Paper, May 3, 2005; DOI 10.1182/blood-2005-01-0264.
Supported by the National Institutes of Health (grants P01-HL-56 920, PO1-DK-5022, RO1-DK-49650, R01-DK2742 and 1 P22 RR18757-01) and the Center of Biomedical Research Excellence (COBRE) Program of the National Center for Research Resources (grant P20 RR018757).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Nicola Kouttab and his laboratory staff for their assistance in flow cytometry analysis.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.






This feature is available to Subscribers Only
Sign In or Create an Account Close Modal