N-terminal natriuretic peptide type B (NT-proBNP) is a marker of cardiac dysfunction in light chain amyloidosis (AL) and a powerful prognostic determinant. Serum NT-proBNP and circulating free light chains (FLCs) were measured at enrollment and after 3 cycles of chemotherapy in 51 patients with cardiac AL. In patients (n = 22, 43%) in whom FLCs decreased by more than 50% (hematologic response), NT-proBNP concentration decreased by a median of 48%, whereas in the remaining patients it increased by 47% (P = .01). The reduction of NT-proBNP was greater in patients (n = 9) in whom amyloidogenic FLCs disappeared at immunofixation (median 53%), than in the remaining responding patients (median 31%, P = .04). Left ventricular wall thickness decreased by at least 2 mm in 3 of 20 patients in whom NT-proBNP improved. Fifteen patients died. Thirteen of them, in whom NT-proBNP and FLCs did not improve, died after a median of 1.8 months. The decrease of FLCs translates into a simultaneous decrease of NT-proBNP and improved survival. Patients in whom chemotherapy fails to induce such a decrease are at risk of early death. Cardiac function in AL can rapidly improve due to a reduction of the circulating amyloidogenic precursor, despite the amount of cardiac amyloid deposits remaining apparently unaltered, as measured by echocardiography.
Introduction
The amyloidoses are disorders of protein conformation, in which different unrelated autologous proteins misfold and aggregate into fibrils that deposit in tissues and cause organ dysfunction.1 In light chain amyloidosis (AL) the fibrils are formed by the N-terminal fragment of a monoclonal immunoglobulin light chain. Thus, in AL, an underlying plasma-cell clone is responsible for the production of the amyloidogenic protein and is the target of specific treatment. The heart is involved in approximately 50% of the patients at diagnosis, but virtually all patients with AL eventually die a cardiac-related death.2 The presence of cardiac amyloidosis is by far the major prognostic determinant.3 Moreover, heart failure conditions the therapeutic strategy, limiting the use of high-dose chemotherapy followed by autologous stem cell transplantation4 and of high-intensity dexamethasone-based regimens.5
Our group reported that the serum concentration of N-terminal natriuretic peptide type-B (NT-proBNP) is a sensitive marker of heart dysfunction caused by AL and a powerful prognostic determinant.6 The prognostic value of NT-proBNP was confirmed by the Mayo Clinic group in subsequent studies that considered this marker in association with cardiac troponins.7,8 In our first retrospective study, we observed in some patients in whom serial measurements of NT-proBNP and of monoclonal protein were available that reduction in the concentration of the monoclonal component over time was paralleled by simultaneous reduction in NT-proBNP concentrations and clinical improvement.6 These findings suggested that NT-proBNP could be used to monitor cardiac response to chemotherapy. The rapidity of changes in NT-proBNP levels during therapy, in most cases without any alterations in cardiac wall thickness at echocardiography, led us to hypothesize that myocardial dysfunction could be caused not only by the presence of amyloid deposits but also by cardiac toxicity exerted by critical concentrations of the amyloidogenic precursor. The availability of a quantitative assay for serum amyloidogenic free light chains (FLCs) renders it possible to estimate the concentration of the circulating amyloidogenic precursor.9 The United Kingdom National Amyloidosis Centre group observed that a more than 50% reduction of FLCs induced by chemotherapy translates into regression of amyloid deposits and improvement of survival.10
In the present study, we prospectively evaluated the concentration of serum NT-proBNP and FLCs at study entry and at the time of evaluation of response to chemotherapy in 51 patients with AL with cardiac involvement.
Patients, materials, and methods
Consecutive patients with AL and cardiac involvement who initiated chemotherapy and were monitored for response at the Center for Amyloidosis in Pavia, Italy, between April 2002 and March 2005 were enrolled into the study. All patients had biopsy-proven amyloidosis. A monoclonal component was detected in serum and/or urine by high-resolution agarose gel immunofixation electrophoresis in all cases.11 The characterization of amyloidosis as AL type was confirmed by immuno-electron microscopy12 and the hereditary forms excluded by DNA analysis. Heart involvement was defined on the basis of echocardiographic evidence; that is, a mean left ventricular wall thickness more than 12 mm in the absence of hypertension or other potential causes of left ventricular hypertrophy, according to the Consensus Opinion from the 10th International Symposium on Amyloid and Amyloidosis.13 Only patients classified as having New York Heart Association (NYHA) class II or higher were included in the study. Patients in dialysis were excluded because of the altered metabolism of NT-proBNP and FLCs.14 Patients in whom a more than 25% decrease or increase in creatinine clearance was observed after chemotherapy were also excluded.
NT-proBNP levels were measured via an electrochemiluminescence sandwich immunoassay (ECLIA; Roche, Basel, Switzerland) on an Elecsys System 2010. Upper reference limits (the 97.5 percentiles of healthy subjects) in men and women were, respectively, 88 ng/L and 153 ng/L in subjects younger than 50 years old and 227 ng/L and 334 ng/L in individuals older than 50 years old. The concentration of circulating FLCs was measured using a latex-enhanced immunoassay (The Binding Site, Birmingham, United Kingdom) on a Behring BN II nephelometric analyzer (Dade Behring, Deerfield, IL). The reference range for polyclonal free κ and free λ light chains was 3.3 mg/L to 19.4 mg/L and 5.7 mg/L to 26.3 mg/L, respectively, with a mean κ-to-λ ratio of 0.59 (95% confidence interval 0.3-1.2, diagnostic range 0.26-1.65).15
The patients were assigned to different therapeutic regimens: melphalan plus high-dose dexamethasone (MDex, n = 25, 49%), thalidomide plus intermediate-dose dexamethasone (TDex, n = 12, 23%), high-dose dexamethasone (Dex, n = 6, 12%), melphalan plus prednisone (MP, n = 4, 8%), or thalidomide alone (n = 4, 8%). None of the patients was eligible for autologous stem cell transplantation (ASCT). The choice of the therapeutic strategy was made following a risk-based approach. Patients ineligible for ASCT according to the criteria proposed by Comenzo and Gertz16 were treated with first-line MDex. If they presented contraindications to Dex (eg, severe fluid retention, poorly controlled diabetes, psychosis) they received standard MP; if they presented contraindications to melphalan (eg, creatinine clearance less than 20 mL/min, plan to undergo stem-cell mobilization if they respond to therapy and become eligible for ASCT), they received Dex alone. Thalidomide was offered to patients who did not respond to or who relapsed after first-line treatment (n = 16, 31%) and was associated to dexamethasone in patients who could tolerate it. NT-proBNP and FLCs were evaluated at study entry and after 3 cycles of chemotherapy (or 3 months after treatment initiation in the case of continuous treatment with thalidomide alone).
Given the reported high biologic variability of serum NT-proBNP evaluation,17,18 we chose to consider a NT-proBNP reduction of at least 30% or its normalization as clinically relevant. According to the Consensus Opinion from the International Society for Amyloidosis, a 2-mm or greater reduction of mean left ventricular wall thickness was considered clinically significant.13
Hematologic response to treatment was defined as a more than 50% reduction of FLCs, and complete remission as disappearance of the amyloidogenic monoclonal component at high-resolution immunofixation with normal κ and λ FLC concentrations and a normal κ-to-λ ratio.11,13
The differences in mean FLC and NT-proBNP changes after chemotherapy between subgroups were tested for statistical significance by the nonparametric Mann-Whitney U test. Survival curves were plotted according to Kaplan-Meier and the difference in survival tested for significance with the log-rank test.
The study was approved by the institutional review board of the “Istituto di Ricovero e Cura a Carattere Scientifico (I.R.C.C.S.) San Matteo” and the patients gave written informed consent, according to the Helsinki Protocol.
Results
Fifty-one patients with AL and cardiac involvement were enrolled into the study. Their clinical characteristics are reported in Table 1.
Clinical characteristics at enrollment of 51 patients with AL and cardiac involvement
. | No. (%) . | Median (range) . |
|---|---|---|
| Male | 27 (53) | NA |
| Age, years | NA | 63 (28-82) |
| Organ involvement | ||
| Kidney | 32 (63) | NA |
| Autonomic nervous system | 10 (20) | NA |
| Liver | 7 (14) | NA |
| Peripheral nervous system | 5 (10) | NA |
| Soft tissues | 5 (10) | NA |
| Gastrointestinal system | 3 (6) | NA |
| More than one organ involved | 42 (82) | NA |
| Serum creatinine, μM/L | NA | 97.2 (44.2-380.1) |
| Creatinine clearance, mL/min | NA | 54 (15-152) |
| Proteinuria, g/24 h | NA | 1.4 (0.1-23) |
| Monoclonal component type, κ:λ | 12/39 (23/77) | NA |
| NT-proBNP concentration, ng/L | NA | 2916 (393-35563) |
| Mean left ventricular wall thickness, mm | NA | 16 (12.5-21) |
| NYHA class II | 22 (43) | NA |
| NYHA class III | 29 (57) | NA |
. | No. (%) . | Median (range) . |
|---|---|---|
| Male | 27 (53) | NA |
| Age, years | NA | 63 (28-82) |
| Organ involvement | ||
| Kidney | 32 (63) | NA |
| Autonomic nervous system | 10 (20) | NA |
| Liver | 7 (14) | NA |
| Peripheral nervous system | 5 (10) | NA |
| Soft tissues | 5 (10) | NA |
| Gastrointestinal system | 3 (6) | NA |
| More than one organ involved | 42 (82) | NA |
| Serum creatinine, μM/L | NA | 97.2 (44.2-380.1) |
| Creatinine clearance, mL/min | NA | 54 (15-152) |
| Proteinuria, g/24 h | NA | 1.4 (0.1-23) |
| Monoclonal component type, κ:λ | 12/39 (23/77) | NA |
| NT-proBNP concentration, ng/L | NA | 2916 (393-35563) |
| Mean left ventricular wall thickness, mm | NA | 16 (12.5-21) |
| NYHA class II | 22 (43) | NA |
| NYHA class III | 29 (57) | NA |
NA indicates not applicable.
At the time of evaluation of response, a more than 50% FLC reduction was observed in 22 patients (43%), and in 7 more patients (14%) the FLCs had decreased by at least 25%. Normalization of FLC concentration and of the κ-to-λ ratio was achieved in 13 cases (25%), and in 9 (18%) of them the monoclonal component disappeared at high-resolution immunofixation. The serum NT-proBNP decreased by at least 30% in 20 patients (39%), and in 2 patients (4%) its levels normalized. The reduction of NT-proBNP was accompanied by an improvement of symptoms of heart failure in all cases, with reduction of at least one NYHA class (from NYHA class II to class I in 7 cases, from NYHA class III to class II in 5 cases, and from NYHA class III to class I in 8 patients). In patients in whom NT-proBNP did not improve, symptoms of heart failure, as assessed by NYHA class, remained stable (26 patients) or worsened (5 patients).
Among the 20 patients in whom NT-proBNP improved after chemotherapy, only 3 (15%) showed a 2-mm or greater decrease in mean left ventricular wall thickness. The characteristics of these patients are reported in Table 2.
Characteristics of 3 patients in whom mean left ventricular wall thickness decreased by 2 mm or more and NT-proBNP decreased by 30% or more after chemotherapy
. | . | FLC, mg/L . | . | . | NT-proBNP, ng/L . | . | Mean VWT, mm . | . | NYHA class . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient no. . | FLC type . | Pre-Tx . | Post-Tx . | CR . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | ||||
| 1 | λ | 248.0 | 68.6 | No | 861 | 174 | 19 | 14 | II | I | ||||
| 2 | λ | 140.0 | 5.3 | Yes | 6 097 | 1052 | 21 | 18 | III | I | ||||
| 3 | κ | 129.0 | 1.7 | Yes | 10 447 | 2746 | 16 | 13 | III | I | ||||
. | . | FLC, mg/L . | . | . | NT-proBNP, ng/L . | . | Mean VWT, mm . | . | NYHA class . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient no. . | FLC type . | Pre-Tx . | Post-Tx . | CR . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | ||||
| 1 | λ | 248.0 | 68.6 | No | 861 | 174 | 19 | 14 | II | I | ||||
| 2 | λ | 140.0 | 5.3 | Yes | 6 097 | 1052 | 21 | 18 | III | I | ||||
| 3 | κ | 129.0 | 1.7 | Yes | 10 447 | 2746 | 16 | 13 | III | I | ||||
Pre-Tx indicates before therapy; Post-Tx, after therapy; CR, complete remission at immunofixation; and VWT, ventricular-wall thickness.
In 18 (90%) of the 20 patients in whom the NT-proBNP decreased by at least 30%, the FLC concentration remaining after chemotherapy was less than 50% and in the 2 remaining patients it was 72% and 74% of that observed at the time of enrollment. In 4 of the 22 patients who obtained a more than 50% reduction of FLCs (without complete remission at immunofixation), the NT-proBNP concentration did not decrease. The characteristics of these patients are reported in Table 3.
Characteristics of 4 patients who obtained 50% or greater reduction of FLC, without improvement of NT-proBNP
. | . | FLC, mg/L . | . | . | NT-proBNP, ng/L . | . | Mean VWT, mm . | . | NYHA class . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient no. . | FLC type . | Pre-Tx . | Post-Tx . | CR . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | ||||
| 1 | κ | 228.0 | 99.1 | No | 1 058 | 1 233 | 14 | 14 | II | II | ||||
| 2 | λ | 90.1 | 8.5 | No | 18 050 | 23 006 | 20 | 19 | III | III | ||||
| 3 | λ | 173.0 | 63.8 | No | 2 706 | 4 046 | 18 | 20 | II | II | ||||
| 4 | λ | 112.0 | 52.8 | No | 1 882 | 3 655 | 16 | 16 | II | II | ||||
. | . | FLC, mg/L . | . | . | NT-proBNP, ng/L . | . | Mean VWT, mm . | . | NYHA class . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient no. . | FLC type . | Pre-Tx . | Post-Tx . | CR . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | Pre-Tx . | Post-Tx . | ||||
| 1 | κ | 228.0 | 99.1 | No | 1 058 | 1 233 | 14 | 14 | II | II | ||||
| 2 | λ | 90.1 | 8.5 | No | 18 050 | 23 006 | 20 | 19 | III | III | ||||
| 3 | λ | 173.0 | 63.8 | No | 2 706 | 4 046 | 18 | 20 | II | II | ||||
| 4 | λ | 112.0 | 52.8 | No | 1 882 | 3 655 | 16 | 16 | II | II | ||||
Pre-Tx indicates before therapy; Post-Tx, after treatment; CR, complete remission at immunofixation; and VWT, ventricular-wall thickness.
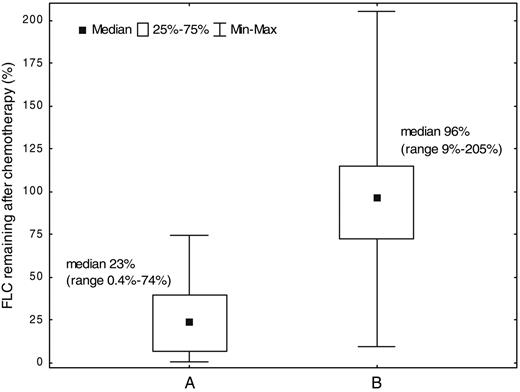
The concentration of FLCs remaining after chemotherapy was significantly lower in patients in whom the NT-proBNP decreased by at least 30% (median 23% vs 96%; P < .001; Figure 1).
Among the patients in whom the FLCs decreased by at least 50%, the median decrease in NT-proBNP was 48%, whereas in the remaining patients the NT-proBNP concentration increased by a median of 47% (P < .001). The reduction of NT-proBNP was more prominent in the 9 patients who achieved a complete remission, with disappearance of the monoclonal component at high-resolution immunofixation, than in the 13 patients who obtained a hematologic response without complete remission (median –53% vs –31%; P = .04; Figure 2).
However, these 13 patients still showed a significant NT-proBNP reduction when compared with the 29 nonresponders (P = .001; Figure 2). Interestingly, all the patients in complete remission achieved a more than 30% improvement of NT-proBNP levels and clinical improvement (at enrollment 6 were classified in NYHA class III and 3 in class II and, after chemotherapy, all of them were classified in NYHA class I).
The changes in NT-proBNP and FLCs after chemotherapy were not correlated with the type or concentration of the amyloidogenic FLCs at enrollment, with the initial concentration of NT-proBNP, with the mean left ventricular wall thickness, or with the NYHA class.
An analysis of the correlation between hematologic response and NT-proBNP modification was performed in the subgroups of patients treated with MDex and thalidomide-based regimens (TDex and thalidomide alone). There was a statistically significant correlation between FLCs and NT-proBNP modifications in each of the subgroups, with no detectable influence of the therapeutic regimen that induced the response (data not shown).
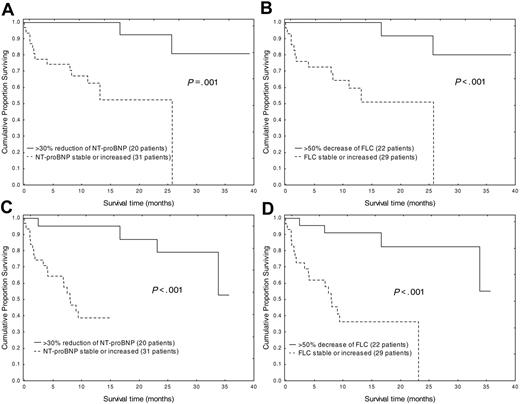
Fifteen patients (29%) died at a median of 3.9 months (range: 0-25.7 months) after evaluation of response. One of them had achieved normalization of FLC concentration and of the κ-to-λ ratio and a 53% reduction of NT-proBNP (from 1364 ng/L to 637 ng/L) and died after 17 months of a nonamyloid-related lung disease. One patient progressed 3 months after having achieved a hematologic response (λ FLC fell from 248 mg/L to 68.6 mg/L) and an 80% decrease of NT-proBNP (from 861 ng/L to 174 ng/L). In this patient relapse was marked by increasing NYHA class (from I to III), NT-proBNP (to 1210 ng/L), and FLCs (to 91 mg/L) and the patient died due to heart failure after a 25-month follow-up. The remaining 13 patients died due to sudden death (2 patients), heart failure (10 patients), or infection (1 patient), after a median follow-up of 1.8 months (range: 0.1-25.7 months) and in none of them had a reduction of FLCs or NT-proBNP been achieved. The median follow-up of living patients is 12.4 months (range: 4.6-39.1 months). Overall median survival has not been reached and median progression-free survival is 23.7 months. Both more than 50% reduction of amyloidogenic FLCs and more than 30% reduction of NT-proBNP resulted in a significant improvement of overall and progression-free survival (Figure 3).
Discussion
These data show that in cardiac AL the chemotherapy-induced decrease of the concentration of the circulating amyloidogenic precursor translates into a reduction of NT-proBNP. In 18 of 20 patients a clinically relevant improvement of NT-proBNP required at least a 50% decrease in the pretreatment concentration of the amyloidogenic FLCs. The 50% FLC reduction threshold is commonly used to define hematologic response to treatment10 and is associated with a prolonged survival.8 Although a minority of patients can achieve an improvement in cardiac dysfunction, as assessed by NT-proBNP, with a less substantial decrease in the circulating amyloidogenic precursor, our data confirm that a reduction of at least 50% of FLCs is usually sufficient. However, complete remission (ie, disappearance of the amyloidogenic FLCs at high-resolution immunofixation) is associated with a more substantial NT-proBNP reduction and with improvement of cardiac dysfunction in all cases. This observation suggests that the more the concentration of the circulating amyloidogenic precursor is reduced by chemotherapy, the greater is the improvement in cardiac dysfunction that can be obtained.
Correlation between changes in NT-proBNP levels and hematologic response to chemotherapy in 51 AL patients with cardiac involvement. (A) Twenty patients in whom NT-proBNP decreased by 30% or more, or normalized; median NT-proBNP modification –52% (range: –95% to –30%). (B) Thirty-one patients in whom NT-proBNP was stable or increased, median NT-proBNP modification +37% (range: –24% to +1862%). The difference between A and B was statistically significant (P < .001) by the Mann-Whitney U test.
Correlation between changes in NT-proBNP levels and hematologic response to chemotherapy in 51 AL patients with cardiac involvement. (A) Twenty patients in whom NT-proBNP decreased by 30% or more, or normalized; median NT-proBNP modification –52% (range: –95% to –30%). (B) Thirty-one patients in whom NT-proBNP was stable or increased, median NT-proBNP modification +37% (range: –24% to +1862%). The difference between A and B was statistically significant (P < .001) by the Mann-Whitney U test.
Changes in N-terminal proBNP levels in patients who reached complete remission, partial remission, or who did not respond to chemotherapy. (A) Nine patients in whom the amyloidogenic FLCs disappeared at immunofixation. (B) Thirteen patients in whom amyloidogenic FLCs decreased by more than 50%, but were still present at immunofixation. (C) Twenty-nine patients in whom FLCs remained stable or increased. The differences between A and B (P = .04), B and C (P = .001), and A and C (P < .001) were statistically significant by Mann-Whitney U test.
Changes in N-terminal proBNP levels in patients who reached complete remission, partial remission, or who did not respond to chemotherapy. (A) Nine patients in whom the amyloidogenic FLCs disappeared at immunofixation. (B) Thirteen patients in whom amyloidogenic FLCs decreased by more than 50%, but were still present at immunofixation. (C) Twenty-nine patients in whom FLCs remained stable or increased. The differences between A and B (P = .04), B and C (P = .001), and A and C (P < .001) were statistically significant by Mann-Whitney U test.
A proportion (18% in the present series) of the patients who achieve a more than 50% reduction of FLCs without complete remission do not obtain an improvement in NT-proBNP levels nor any clinical benefit (as assessed by reduction of NYHA class). It is possible that these patients already have irreversible cardiac damage, although there are no elements (NT-proBNP concentration, FLC type and concentration, mean left ventricular wall thickness at echocardiography, clinical presentation) to differentiate them from the remaining patient population before therapy. More likely, these clones may produce a light chain with high propensity to aggregate and thus a more drastic reduction of their concentration may be required in order to achieve benefits in organ function and survival.
Effects of NT-proBNP and FLC reduction on survival. Effect of NT-proBNP reduction on overall (A) and progression-free (C) survival and effect of FLC reduction on overall (B) and progression-free (D) survival.
Effects of NT-proBNP and FLC reduction on survival. Effect of NT-proBNP reduction on overall (A) and progression-free (C) survival and effect of FLC reduction on overall (B) and progression-free (D) survival.
In the present study, both hematologic response and improvement of NT-proBNP were associated to prolonged overall and event-free survival. A longer follow-up of a greater number of patients allowing a multivariate analysis will clarify whether hematologic response in the absence of an improvement of NT-proBNP can still endow a survival advantage. This is particularly important for defining the optimal therapeutic target: that is, hematologic response alone or in conjunction with a significant improvement of a marker of organ function such as NT-proBNP. The clarification of this important matter will affect the tailoring of the anticlone treatment, improving our ability to fine tune the balance between the toxicity of chemotherapy and its clinical benefit.
With the exception of 2 patients, all the patients who died had not achieved reductions in either FLC or NT-proBNP levels and they died after a median follow-up of 1.8 months from evaluation of response. It is clear that the absence of an improvement of FLCs and NT-proBNP after the first 3 cycles of therapy identifies a subset of patients at high risk of an early death. This underlines the need for an aggressive follow-up of patients with AL cardiomyopathy during therapy, in order to recognize the patients who will not benefit from the ongoing treatment as soon as possible, and to promptly start second-line regimens.
The changes in NT-proBNP and FLC concentrations were simultaneous and obtained after only 3 cycles of chemotherapy. The reduction of serum NT-proBNP was accompanied by an improvement of symptoms of heart failure, but only in 3 of 20 patients did we observe a 2 mm or greater reduction of the mean left ventricular wall thickness at echocardiography. Thus, one of the commonly accepted markers for determining the response of amyloid cardiac involvement to chemotherapy13 appears to be insensitive and could lead to an underestimation of the effect of treatment. It is likely that other more refined echocardiographic parameters, which were not considered in the present study, can better identify rapid changes of cardiac function. However, our data show that the combination of measurements of 2 readily available biochemical markers, FLCs and NT-proBNP, can significantly improve the management of AL patients by detecting early organ response and, most importantly, early treatment failures.
Finally, these data show that in AL a reduction of the concentration of the circulating amyloidogenic precursor is associated with a rapid improvement in cardiac dysfunction. This is the first documentation in humans of a direct link between the concentration of the circulating amyloidogenic precursor and target organ dysfunction, independently of the amyloid load. However, the molecular species involved in cardiotoxicity (ie, early aggregates, oligomers of the amyloidogenic precursor as well documented in Aβ Alzheimer amyloidosis,19 or nascent amyloid fibrils) has not yet been defined. Clarification of this crucial point is important for directing the therapeutic effort.
Prepublished online as Blood First Edition Paper, January 24, 2006; DOI 10.1182/blood-2005-11-4385.
Supported in part by an investigator fellowship from Collegio Ghislieri, Pavia, Italy (G.P.).
A.R.B. has declared a financial interest in The Binding Site Ltd, Birmingham, United Kingdom, whose product, the serum free light chain assay, was studied in the present work.
G.P. and G.M. participated in the study concept, study design, data collection, data analysis, and writing of the report; F.L., P.R., S.P., V.P., and L.O. participated in data collection, data analysis, and manuscript review; T.B. was involved in performing the free light chain test, data collection, and manuscript review; A.R.B., G.M.D'E., R.F., and R.M. participated in study design and manuscript review.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal