Abstract
B-lymphocyte stimulator (BLyS), a relatively recently recognized member of the tumor necrosis factor ligand family (TNF), is a potent cell-survival factor expressed in many hematopoietic cells. BLyS binds to 3 TNF-R receptors, TACI, BCMA, BAFF-R, to regulate B-cell survival, differentiation, and proliferation. The mechanisms involved in BLYS gene expression and regulation are still incompletely understood. In this study, we examined BLYS gene expression, function, and regulation in B-cell non-Hodgkin lymphoma (NHL-B) cells. Our studies indicate that BLyS is constitutively expressed in aggressive NHL-B cells, including large B-cell lymphoma (LBCL) and mantle cell lymphoma (MCL), playing an important role in the survival and proliferation of malignant B cells. We found that 2 important transcription factors, NF-κB and NFAT, are involved in regulating BLyS expression through at least one NF-κB and 2 NFAT binding sites in the BLYS promoter. We also provide evidence suggesting that the constitutive activation of NF-κB and BLyS in NHL-B cells forms a positive feedback loop associated with lymphoma cell survival and proliferation. Our findings indicate that constitutive NF-κB and NFAT activations are crucial transcriptional regulators of the BLyS survival pathway in malignant B cells that could be therapeutic targets in aggressive NHL-B.
Introduction
B-lymphocyte stimulator (BLyS; also known as BAFF, TALL-1, THANK, zTNF4, and TNFSF13B) exists as a homotrimer in hematopoietic cells, either on the cell surface as a type 2 transmembrane protein or is released in a soluble form after plasma membrane cleavage. BLyS belongs to the tumor necrosis factor (TNF) ligand family that plays crucial roles in B-cell homeostasis, tolerance, and malignancy.1-5 BLyS-deficient mice are viable at birth but lack a mature B-cell compartment (follicular and marginal zone B lymphocytes), suggesting that the expression of this gene is necessary to maintain mature B-cell development.5 Three BLyS receptors have been identified: BCMA (B-cell maturation antigen), TACI (transmembrane activator, calcium-modulator, and cyclophilin ligand interactor), and BAFF-R/BR3 (BAFF receptor/BLyS receptor 3). In particular, the BLyS/BAFF-R pathway is crucial to the survival of peripheral B cells.6-8
BLyS is expressed in a cell membrane bound or soluble form1-4 by various cell types, including dendritic cells, monocytes, macrophages, activated T cells, neutrophils, and antigen-presenting cells.1-4,9-19 Cytokines such as interleukin 10 (IL-10), interferon γ (IFN-γ), and IFN-α augment BLyS expression in monocytes, macrophages, and dendritic cells, while CD40 ligand stimulates BLyS secretion from dendritic cells.19 BLyS levels are elevated in the serum of non-Hodgkin lymphoma (NHL) patients and have been reported to be associated with disease activity progression and patient prognosis.13
Several studies have shown that malignant B cells from NHL-B and multiple myeloma (MM) patients also express abnormal levels of BLyS protein, which protects malignant B cells from spontaneous apoptosis and myeloma cells from apoptosis induced by IL-6 deprivation or dexamethasone.9,11,12,20,21 In addition to its antiapoptotic activity in malignant B cells, BLyS also promotes MM cell survival.21 Various studies also have shown that inhibiting BLyS protein using decoy receptors or blocking antibodies restores the apoptotic process in malignant B cells and myeloma cells.9,12,19,20,22
NF-κB is a family of important transcription factors that regulate B-cell development, maintenance, and stimulation.23,24 B-cell receptor signaling and some tumor necrosis factor (TNF) cytokine signaling induce NF-κB activation through the NF-κB1 pathway,25 where phosphorylation of the NF-κB inhibitor IκB by the IκB kinase (IKK) complex allows the cytoplasmic NF-κB proteins p65 and p50 to translocate to the nucleus when their nuclear localization sequence (NLS) is exposed. Alternatively, NF-κB also can be activated through the NF-κB2 pathway, in which the NF-κB2 precursor p100 is proteolytically cleaved to activate p52 through the NF-κB–inducing kinase(NIK) and IKKα.26-28 Both mechanisms of NF-κB activation play important roles in B-cell development and survival.26,29 Constitutive NF-κB activation is a molecular “signature” that has been reported in several malignant B-cell types, including aggressive NHL-B cells.30-33
In vivo and in vitro studies have demonstrated that BLyS signaling increases the expression of antiapoptotic molecules such as Bcl-2 and promotes cell survival, cell-cycle progression, and proliferation of B cells.34-37 Previous studies also have shown that BLyS can activate NF-κB2 through the ubiquitin-mediated proteolysis of p100,27,28 and the NF-κB1 pathway through the proteolysis of IκBα in vitro.35,38 These studies suggest that activation of NF-κB family members play a major role in critical BLyS signaling pathway in the mature B-cell lineage.
The nuclear factor of activated T cells (NFAT) is another important family of transcription factors that play key roles in the transcriptional activation of T-lymphocyte cytokines such as IL-2, IL-4, CD40L, and Fas ligand.39 In resting T lymphocytes, these transcription factors are maintained in the cell cytoplasm in the phosphorylated state. In response to increasing intracellular concentrations of calcium, the N-terminus of the NFAT protein is dephosphorylated by a calcium-sensitive protein phosphatase, calcineurin, that induces exposure of the NFAT protein NLS and leads to NFAT translocation from the cytoplasm to the nucleus.39-42 Recent studies have shown that the NFAT family members NFATc1 and NFATc2 are constitutively activated in malignant B cells,43,44 suggesting that both NFAT and NF-κB activation likely contribute to malignant B-cell survival.
Although it is known that NF-κB, NFAT, and BLyS are important components of cellular pathways that maintain B-cell survival and proliferation, the mechanism(s) underlying their persistent activation and expression, as well as intracellular interactions between these proteins in malignant B cells, are still unclear. In this study, we show that constitutive BLyS expression plays an important role in NHL-B cell survival and also identify one NF-κB binding site and 2 NFAT binding sites in the BLYS promoter that are critical for BLYS gene transcription. Our findings indicate that constitutive activation of NF-κB and NFAT family members is critical for the transcriptional regulation of the BLyS survival pathway in both normal and malignant B cells. Recognition that this pathway is involved in the pathophysiology of NHL-B may provide a useful future therapeutic target in aggressive NHL-B.
Materials and methods
Cells
Human NHL-B cell lines were established from fresh patient biopsy samples. MS, JM, and DS are LBCL cell lines. Jeko, SP53, Granta, and JMP1 are previously established mantle cell lymphoma (MCL) cell lines.45 This study was conducted in accordance with the Helsinki protocol and approved by the M D Anderson Cancer Center Institution Review Board. Informed consent was obtained from all patients whose tumor samples were used. Tumor cell samples after preliminary isolation procedures contained more than 90% NHL-B cells by flow cytometry analysis. Cells were cultured in RPMI (GIBCO, Rockville, MD) containing 15% fetal bovine serum (FBS) (Hyclone, Logan, UT). Normal human B lymphocytes were purified from healthy donors' buffy coats by using the appropriate ratio of RosetteSep human B-cell enrichment cocktail (StemCell Technologies, Vancouver, BC, Canada). Cells were incubated in 50 mL tubes with the cocktail for 20 minutes at room temperature and then underlayered with 15 mL Ficoll-Paque PLUS (Amersham Pharmacia Biotech, Arlington Heights, IL). The gradient was centrifuged for 20 minutes at 1200g at room temperature. The interfaces were collected, washed with 2% FBS phosphate-buffered saline (PBS) solution, and analyzed by flow cytometry (FACS Caliber) (BD Bioscience, San Jose, CA) that showed that the cells were 95% to 98% CD20 positive. Normal Go peripheral blood B cells were activated by incubating for 24 hours with anti-IgM (α-μ) (35 μg/mL; ICN, Aurora, OH) and soluble CD40L (1 μg/mL; PeproTech EC, Rocky Hill, NJ). Fresh biopsy-derived lymphoma tissues were minced in cold RPMI, and single-cell suspension of lymphoma cells were purified by Ficoll-Paque PLUS and stained positive for CD19, CD20, and CD10 but negative for CD3 by immunohistochemistry.
Reagents
The phospho-IκBα inhibitor BAY11-7082 was purchased from Calbiochem (San Diego, CA). The calcineurin inhibitor cyclosporin A (CsA) was purchased from Sigma-Aldrich (St Louis, MO). Antibodies against the following molecules were used: BLyS polyclonal antibody for Western blotting (Upstate Biotechnology, Lake Placid, NY); BLyS monoclonal antibody for immunostaining (R&D Systems, Minneapolis, MN); NF-κB p50, p52, and p65 (Upstate Biotechnology, Lake Placid, NY); c-Rel (Chemicon International, Temecula, CA); and BLyS polyclonal antibody for neutralization of bioactivity, Rel-B, NFAT C1, C2, C3, cyclin D1, Bcl-xL, Bcl-2, and pIκBα (Santa Cruz Biotechnology, Santa Cruz, CA). The following kits were used: Ready-To-Go RT-PCR beads (Amersham Pharmacia Biotech), NucleoSpin RNA II purification kit (BD Bioscience), QuikChange Multi Site-Directed Mutagenesis Kit (Stratagene, La Jolla, CA), cell death detection kit, fluorescein (Roche Applied Science, Indianapolis, IN), and ApoAlert caspase 3 colorimetric assay kit (Clontech, Palo Alto, CA), and cell proliferation kit II (XTT) (Roche Applied Science, Penzberg, Germany). siRNA oligonucleotides for p52 and rel-B were purchased from Santa Cruz Biotechnology. BLyS siRNA and negative control (nontargeting RNA sequence) oligonucleotides were purchased from Upstate Biotechnology.
In vitro [3H]thymidine proliferation assays
Proliferation assays were performed as described previously.37 Briefly, cells were plated in triplicate at 4 × 104 cells per well in 200 μL of RPMI 1640 with 15% fetal calf serum and the indicated reagents (siRNA of BLYS or negative control nucleotides) in a 96-well plate and incubated in 5% CO2 at 37°C. Each well was pulsed with 0.5 μCi (0.0185 MBq)/10 μL of [3H]thymidine (Amersham Pharmacia Biotech) for 16 hours before harvest. Cells were then harvested, and the radioactivity was counted in a Beckman LS3800 liquid scintillation counter.
Electrophoretic mobility shift assay (EMSA)
Gel-shift assays were performed as follows. A 20-mer double-stranded NF-κB oligonucleotide (5′-AACTGGGGAATGTCCAGGAA-3′) and two 20-mer double-stranded NFAT oligonucleotides (5′-AGACTGTGTGGAAATGTAGAGT-3′) and (5′-GTCCCAGAAGGAAAAAGTTTAT-3′) were labeled with γ-32P and incubated with nuclear extract for 15 minutes. The extracts were electrophoresed on 6% nondenaturing acrylamide gels. Corresponding unlabeled oligonucleotides were used for competition experiments. The gels were dried and assayed using a Typhoon Phosphor Imager (Amersham Biosciences, Piscataway, NJ).
RT-PCR analysis
Total RNA was prepared using protocol from a NucleoSpin RNA II purification kit (BD Biosciences). Total RNA (5 μg) was used to perform first-strand cDNA synthesis by reverse transcription. The sequences of the BLYS primers were previously described,2 which are 5′-GGAGAAGGCAACTCCAGTCAGAAC-3′ (forward) and 5′-CAATTCATCCCCAAAGACATGGAC-3′ (reverse). The polymerase chain reaction (PCR) conditions were 94°C for 1 minute, 55°C for 1 minute, and 72°C for 1 minute for 40 cycles.
XTT proliferation assay
Cells were plated in triplicate at 1.5 × 104 cells per well in 100 μL RPMI 1640 with 15% fetal calf serum and the indicated reagents (20 μg/mL goat IgG or goat polyclonal BLyS antibody) in a 96-well plate and incubated in 5% CO2 at 37°C. After 48 hours, 50 μL XTT labeling mixture was added to the culture media and incubated overnight. The samples were measured using a Benchmark microplate reader (Bio-Rad Laboratories, Hercules, CA) with 490 nm absorbance wavelength and 655 nm reference wavelength.
Immunoblot analysis
Whole-cell extracts (50 μg) were solubilized with 1.0% sodium dodecyl sulfate (SDS) sample buffer and electrophoresed on a 4% to 15% SDS gel (Bio-Rad, Richmond, CA). Protein was transferred onto a polyvinylidene difluoride membrane, probed with specific primary antibodies, and treated with the appropriate horseradish peroxidase–conjugated secondary antibodies (Amersham Pharmacia Biotech). Protein was visualized by enhanced chemiluminescence ECL (Amersham).
Confocal microscopic analysis
Cells were cytospun onto poly-l-lysine–coated glass slides, fixed with 100% cold methanol for 5 minutes, and air dried. Nonspecific protein binding was prevented by blocking the cells with 10% fetal calf serum (FCS) in PBS. Cells were stained with the appropriate primary antibodies (1:200 dilution) overnight at 4°C. After 3 washes with PBS, the slides were stained with the appropriate antidonkey secondary antibodies (labeled with Cy2, 1:200 dilution) for 45 minutes and washed with PBS. Coverslips were applied with Slow Fade reagent (Molecular Probes, Eugene, OR). The cells were visualized using an Olympus FluoView 500 (FV500) laser scanning confocal microscope (Olympus America, Melville, NY). Images were captured with a PlanApo 40 ×/1.4 numeric aperture oil objective using the appropriate filter sets. Digital images were obtained using the manufacturer's FluoView software.
Flow cytometry
Cells (1 × 105) were washed in PBS containing 2% FCS and incubated with fluorescein isothiocyanate (FITC)–conjugated anti-BLyS antibody (Alexis Biotechnology, San Diego, CA) or FITC-conjugated isotopic control antibody (BD Bioscience) for 1 hour at room temperature. Cells were analyzed using a FACS Caliber (BD Bioscience).
TUNEL and caspase-3 activity assays
TdT-mediated dUTP nick end labeling (TUNEL) assay was performed with an in situ cell death detection kit (Roche Applied Science). Cells were cytospun onto poly-L-lysine–coated glass slides, fixed, permeabilized, and incubated with TUNEL reaction mixture at 37°C for 1 hour as described in the manufacturer's protocol. Cells were analyzed by confocal microscopy. Caspase-3 activity was detected with a BD ApoAlert caspase-3 colorimetric assay kit (Clontech). The cell samples were prepared using the manufacturer's protocol.
Plasmid and site-directed mutagenesis
To construct the pGL4-basic BLYS-luc reporter plasmid, BLYS promoter DNA was amplified by PCR with oligonucleotide primers (5′-ATTGGTACCAGCCTGGGTCTGGAGTT-3′[forward] and 5′-AGAGCTCACTTGGAGTTTGGATTGG-3′[reverse]) and then inserted into the pGL4-basic luciferase reporter vector using the SacI and XhoI sites. Site-directed mutagenesis of the pGL4-basic-BLYS-Luc at the NF-κB site (–869 bp from AACTGGGGAATGTCCAGGAA to AACTGGGTCTGTCCAGGAA; mutated residues are underlined), NFAT1 site (–1018 bp from AGACTGTGTGGAAATGTAGAGT to AGACTGTGTGGTCATGTAGAGT) and NFAT2 site (–505 pb from GTCCCAGAAGGAAAAAGTTTAT to GTCCCAGAAGGCCAAAGTTTAT) was performed using the QuickChange Multi Site-Directed Mutagenesis Kit (Stratagene). All mutations in reporter constructs were verified by nucleotide sequencing. The pCMV-IκBα plasmid was purchased from Clontech. The dominant negative (DN)–NFAT expression vector was a gift from Dr Chi-Wing Chow (Department of Molecular Pharmacology, Albert Einstein College of Medicine). The CMV-hc-Rel expression vector was a gift from Dr Celine Gelinas (Center for Advanced Biotechnology and Medicine, Piscataway, NJ). The NFATc1 eukaryotic expression vector construct was kindly provided by Dr Gerald R. Crabtree (Department of Pathology, Stanford University, Palo Alto, CA).
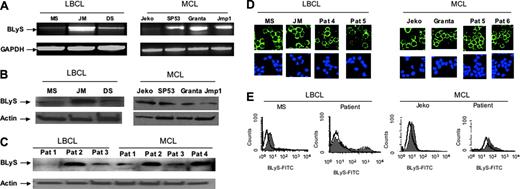
BLyS is constitutively expressed in aggressive NHL-B cells. (A) RT-PCR analysis of BLYS mRNA expression in NHL-B cell lines. (B) Immunoblot analysis of BLyS protein expression in NHL-B cell lines. (C) Immunoblot analysis of BLyS protein expression in cells from representative NHL-B patient biopsies. (D) Confocal immunofluorescence microscopic analysis of BLyS protein localization in LBCL and MCL cell lines and representative biopsy-derived LBCL and MCL patient samples. BLyS protein was stained for Cy2 (green) fluorescence, and the nuclear marker for TOPRO-3 (blue) fluorescence. (E) Flow cytometric analysis of BLyS protein on NHL-B cell surfaces. NHL (LBCL and MCL) cell lines and tumor cells from patient biopsies were stained with FITC-conjugated BLyS antibody (gray histograms) or FITC-conjugated isotype control (open histograms).
BLyS is constitutively expressed in aggressive NHL-B cells. (A) RT-PCR analysis of BLYS mRNA expression in NHL-B cell lines. (B) Immunoblot analysis of BLyS protein expression in NHL-B cell lines. (C) Immunoblot analysis of BLyS protein expression in cells from representative NHL-B patient biopsies. (D) Confocal immunofluorescence microscopic analysis of BLyS protein localization in LBCL and MCL cell lines and representative biopsy-derived LBCL and MCL patient samples. BLyS protein was stained for Cy2 (green) fluorescence, and the nuclear marker for TOPRO-3 (blue) fluorescence. (E) Flow cytometric analysis of BLyS protein on NHL-B cell surfaces. NHL (LBCL and MCL) cell lines and tumor cells from patient biopsies were stained with FITC-conjugated BLyS antibody (gray histograms) or FITC-conjugated isotype control (open histograms).
Transfection, luciferase, and beta-galactosidase (β-gal) assays
Transient transfections of cultured lymphoma cells were conducted using the nucleofector protocol from Amaxa Biosystems (Cologne, Germany).33 Luciferase and β-gal assays were performed according to the manufacturer's directions (Promega, Madison, WI). Each sample in an experiment was repeated at least 3 times in different experiments with similar results. Luciferase activity values were normalized to transfection efficiency by the cotransfected β-gal expression vector.
Results
BLyS is constitutively expressed in aggressive NHL-B cells
Since BLyS has been shown to be an important factor that maintains B-cell growth and survival, we first examined the expression of BLyS in representative LBCL (MS, JM, DS) and MCL (Jeko, SP53, Granta, Jmp1) cell lines. RT-PCR analysis showed that BLYS mRNA is expressed constitutively but in quantitatively variable amounts in all 3 LBCL and 4 MCL cell lines (Figure 1A). Western blot analysis further confirmed that BLyS protein is expressed in all LBCL and MCL cell lines studied (Figure 1B) and in representative biopsy-derived LBCL and MCL patient samples (Figure 1C). Localization of BLyS protein was then determined using immunofluorescence confocal microscopy. It can be seen that BLyS protein is located in the plasma membrane of both NHL-B (LBCL and MCL) cell lines and fresh biopsy-derived LBCL and MCL patient samples (Figure 1D). Membrane-bound BLyS protein also can be detected on LBCL and MCL cell surfaces by flow cytometry (Figure 1E) in both lymphoma cell lines and patient biopsy samples.
Constitutive BLyS expression contributes to NHL-B cell survival in vitro
To determine whether BLyS protein is involved in the survival of aggressive NHL-B cells, a representative LBCL cell line (MS) and a representative MCL cell line (Jeko) were treated with control IgG or BLyS antibody, and effects on cell survival were assessed. Growth of NHL-B cells can be inhibited about 70% to 80% when BLyS bioactivity was blocked by specific BLyS antibody in 48 hours as compared to control IgG (Figure 2A). To determine whether BLyS antibody inhibited cell growth due to cell death, BLyS antibody-treated cells were subjected to TUNEL assays for detecting apoptosis. As shown in Figure 2B, apoptotic (green fluorescent) cells were significantly more prominent after treatment with BLyS antibody (right panel) than with control IgG (left panel).
Constitutive BLyS expression contributes to NHL-B cell survival in vitro. (A) XTT proliferation assay of NHL-B (LBCL-MS, MCL-Jeko) cells treated with control IgG or BLyS antibody. The number of live cells was monitored by the absorbance of 490 nm wavelength. (B) TUNEL analysis of NHL-B (LBCL-MS) cells treated with control IgG or BLyS antibody. Free DNA fragments in apoptotic cells were labeled with green fluorescence. (C) Proliferation of NHL-B (LBCL-MS) cells transfected with BLYS siRNA or control nontargeting sequence. DNA synthesis was assessed by [3H]thymidine uptake in vitro. (D) Immunoblot analysis of BLyS protein in NHL-B (LBCL-MS) cells transfected with BLYS siRNA or control siRNA. Actin was used as loading control. The BLyS level was analyzed by BioMax 1D software, normalized with actin levels, and presented as relative fold decrease compared to control samples. (E) TUNEL analysis of NHL-B (LBCL-MS) cells transfected with BLYS siRNA or a control siRNA. Free DNA fragments in apoptotic cells were labeled with green fluorescence. (F) Caspase-3 activity in an NHL-B (LBCL-MS) cell line transfected with BLYS or control siRNA. (G) Immunoblot analysis of Bcl-2 and Bcl-xL in NHL-B (LBCL-MS) cells transfected with BLYS or control siRNA. Bcl-2 and Bcl-xL levels were normalized to those of actin previously described in D. (H) Immunoblot analysis of BLyS, c-myc, and cyclin D1 in NHL-B cell line cells transfected with BLYS or control siRNA. Actin was used as loading control. The BLyS, c-myc, and cyclin D1 levels were normalized to those of actin as previously described in panel D. The data in panels A, C, and F are representative of 2 independent experiments. The error bars indicate standard deviation of triplicate samples.
Constitutive BLyS expression contributes to NHL-B cell survival in vitro. (A) XTT proliferation assay of NHL-B (LBCL-MS, MCL-Jeko) cells treated with control IgG or BLyS antibody. The number of live cells was monitored by the absorbance of 490 nm wavelength. (B) TUNEL analysis of NHL-B (LBCL-MS) cells treated with control IgG or BLyS antibody. Free DNA fragments in apoptotic cells were labeled with green fluorescence. (C) Proliferation of NHL-B (LBCL-MS) cells transfected with BLYS siRNA or control nontargeting sequence. DNA synthesis was assessed by [3H]thymidine uptake in vitro. (D) Immunoblot analysis of BLyS protein in NHL-B (LBCL-MS) cells transfected with BLYS siRNA or control siRNA. Actin was used as loading control. The BLyS level was analyzed by BioMax 1D software, normalized with actin levels, and presented as relative fold decrease compared to control samples. (E) TUNEL analysis of NHL-B (LBCL-MS) cells transfected with BLYS siRNA or a control siRNA. Free DNA fragments in apoptotic cells were labeled with green fluorescence. (F) Caspase-3 activity in an NHL-B (LBCL-MS) cell line transfected with BLYS or control siRNA. (G) Immunoblot analysis of Bcl-2 and Bcl-xL in NHL-B (LBCL-MS) cells transfected with BLYS or control siRNA. Bcl-2 and Bcl-xL levels were normalized to those of actin previously described in D. (H) Immunoblot analysis of BLyS, c-myc, and cyclin D1 in NHL-B cell line cells transfected with BLYS or control siRNA. Actin was used as loading control. The BLyS, c-myc, and cyclin D1 levels were normalized to those of actin as previously described in panel D. The data in panels A, C, and F are representative of 2 independent experiments. The error bars indicate standard deviation of triplicate samples.
To further determine whether constitutive BLyS protein expression is involved in the survival of aggressive NHL-B cells, LBCL (MS) cells were transfected with a BLYS siRNA. In vitro studies with BLYS siRNA inhibited lymphoma cell growth by approximately 50% after 48 hours when compared to control siRNA (Figure 2C). Furthermore, BLyS protein expression was reduced by approximately 60% in 24 hours after treatment with BLYS siRNA when compared to control siRNA (Figure 2D).
To determine whether BLYS siRNA inhibited cell growth due to cell death, BLYS siRNA-treated cells were subjected to TUNEL assays for detecting apoptosis. As shown in Figure 2E, apoptotic (green fluorescent) cells were significantly more prominent after treatment with BLYS siRNA (right panel) than with control siRNA (left panel). To further confirm the BLYS siRNA transfected cells undergo apoptosis, the activity of the apoptotic protein caspase-3 also was assessed. We observed a 4-fold increase in caspase-3 activity in NHL-B cells (LBCL-MS) transfected with BLYS siRNA, compared with a negative control plasmid (Figure 2F). Western blot analysis of the Bcl-2 family survival proteins Bcl-2 and Bcl-xL also showed that the 2 molecules that are constitutively activated in these cells were down-regulated by approximately 20% and 40%, respectively, after inhibition of BLyS expression (Figure 2G).
To assess whether BLyS expression is involved in NHL-B cell proliferation, we next evaluated the expression of c-myc and cyclin D1, which are important molecules in cell-cycle entry and progression. Western blot analysis showed that the expression of both c-myc and cyclin D1 expression is substantially decreased after inhibition of BLyS expression in NHL-B cells (Figure 2H), indicating that BLyS expression is involved in and may be important for NHL-B cell proliferation.
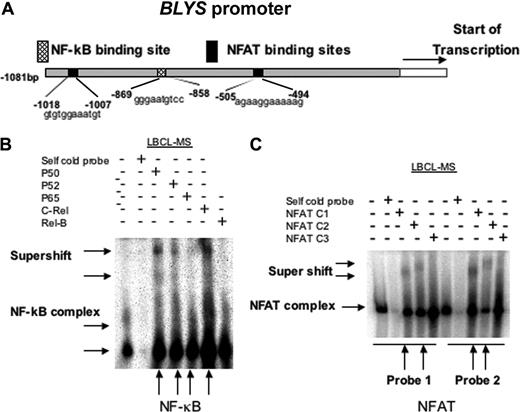
Transcription factors NF-κB and NFAT bind to the BLYS promoter
Because our data has shown that BLyS is required for NHL-B survival, we hypothesized that BLYS might be regulated by NF-κB and NFAT, 2 transcription factor families involved in lymphoid cell growth and survival. To determine whether BLYS is targeted by NF-κB or NFAT, the BLYS promoter sequence was scanned with MatInspector V2.2 software, and a single putative binding site for NF-κB and 2 putative binding sites for NFAT were identified (Figure 3A). To assess the binding activity of NF-κB in the BLYS promoter, we performed EMSA supershift assays with nuclear extracts from NHL-B cells (LBCL-MS) using specific antibodies to NF-κB family members. The NF-κB components binding to the BLYS promoter included predominantly p50, p52, c-Rel, and to a lesser extent p65 (Figure 3B). The c1 and c2 subunits of NFAT also were found in the NFAT complex binding to the BLYS promoter, but the c3 subunit was not present (Figure 3C).
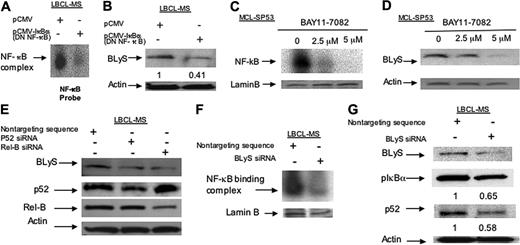
Constitutive BLyS expression stimulating the NF-κB pathway may activate a positive feedback loop contributing to NHL-B cell survival
To further evaluate the effects of the NF-κB1 pathway on BLyS expression in NHL-B cells, EMSAs were performed with nuclear extracts from NHL-B cells (LBCL-MS) transfected with dominant-negative NF-κB, a plasmid overexpressing IκBα. These studies show significantly decreased NF-κB DNA-binding activities in NHL-B cells transfected with a dominant-negative NF-κB construct, compared to control cells (Figure 4A). BLyS protein expression also was decreased (∼ 60%) in NHL-B cells (LBCL-MS) transfected with the dominant-negative NF-κB (Figure 4B). To confirm the possible regulatory activity of NF-κB on BLyS expression, NHL-B cells (MCL-SP53) were treated with BAY11-7082, an IκBα phosphorylation inhibitor. BAY11-7082 significantly reduced NF-κB binding activity to BLYS promoter (Figure 4C) and BLyS protein expression (Figure 4D) in NHL-B cells in a dose-dependent manner.
Transcription factors NF-κB and NFAT bind to the BLYS promoter. (A) BLYS gene promoter diagram (GenBank accession no. AY129225) showing the putative binding sites for NF-κB (dots) and NFAT (black). (B) EMSA analysis of NF-κB binding to the BLYS promoter. Nuclear extracts from NHL-B (MS) cells were incubated with BLYS–NF-κB binding site oligonucleotides. BLYS-NF-κB cold probe and antibodies to p50, p52, p65, c-rel, or rel-B were added to the binding reaction mixtures. Arrows indicate the DNA-protein and supershifted complex. (C) EMSA analysis of NFAT binding to BLYS promoter. Nuclear extracts from NHL-B (LBCL-MS) cells were incubated with oligonucleotides for the 2 different BLYS-NFAT binding sites. BLYS-NFAT cold probes and antibodies to NFATc1, NFATc2, or NFATc3 were added to the binding reaction mixtures. Arrows indicate the DNA-protein and supershifted complexes.
Transcription factors NF-κB and NFAT bind to the BLYS promoter. (A) BLYS gene promoter diagram (GenBank accession no. AY129225) showing the putative binding sites for NF-κB (dots) and NFAT (black). (B) EMSA analysis of NF-κB binding to the BLYS promoter. Nuclear extracts from NHL-B (MS) cells were incubated with BLYS–NF-κB binding site oligonucleotides. BLYS-NF-κB cold probe and antibodies to p50, p52, p65, c-rel, or rel-B were added to the binding reaction mixtures. Arrows indicate the DNA-protein and supershifted complex. (C) EMSA analysis of NFAT binding to BLYS promoter. Nuclear extracts from NHL-B (LBCL-MS) cells were incubated with oligonucleotides for the 2 different BLYS-NFAT binding sites. BLYS-NFAT cold probes and antibodies to NFATc1, NFATc2, or NFATc3 were added to the binding reaction mixtures. Arrows indicate the DNA-protein and supershifted complexes.
To determine whether the NF-κB 2 pathway also might be involved in regulation of BLyS expression, siRNA specific for molecules in the NF-κB2 pathway (p52 or Rel-B) was employed. Western blot analysis showed that blocking the NF-κB2 pathway specifically reduced BLyS protein expression (Figure 4E), suggesting that both NF-κB pathways are involved in regulation of BLyS expression in NHL-B cells.
Since the NF-κB components binding to the BLYS promoter included predominantly p50, p52, and c-Rel, and to a lesser extent p65 (Figure 3B), subsequent EMSA analysis showed that BLYS siRNA treatment reduces these NF-κB components' activity in NHL-B cells (Figure 4F). Regulation of NF-κB activity by BLyS was confirmed in NHL-B cells in vitro, where BLyS expression was inhibited by BLYS siRNA transfection, which led to a decrease in the phosphorylation of IκBα and cleavage of p100 to p52 in NHL-B cells (Figure 4G). These results suggest that BLyS and NF-κB may form a positive feedback loop that promotes NHL-B cell survival, where constitutively expressed BLyS protein in NHL-B cells binds to its cognate receptor(s), which in turn maintains the BLyS ligand expression through stimulation of the NF-κB pathway that is required for BLYS gene expression.
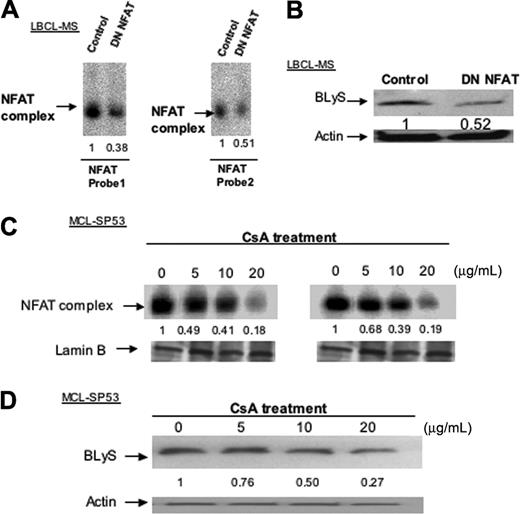
Inhibition of NFAT activation in NHL-B cells reduces BLyS protein expression
To evaluate a possible effect of NFAT on BLyS expression in NHL-B cells, EMSAs were performed with nuclear extracts from NHL-B cell line cells (LBCL-MS) transfected with a dominant-negative NFAT vector (a plasmid expressing a mutant calcineurin molecule). These assays detected a decrease of NFAT DNA-binding activities in BLYS promoter (Figure 5A). BLyS protein expression (Figure 5B) was significantly decreased in cells transfected with dominant-negative NFAT when compared to control lymphoma cells. To further assess the role of NFAT in BLyS expression, NHL-B cells (MCL-SP53) were treated with the calcineurin inhibitor cyclosporine A (CsA), an inhibitor of NFAT. In these studies, NFAT binding activity to the BLYS promoter (Figure 5C) and BLyS protein expression level (Figure 5D) were decreased in NHL-B cells treated with CsA, indicating that NFAT proteins also are involved in the regulation of BLyS expression.
Constitutive BLyS expression through the NF-κB pathway activates a positive feedback loop contributing to NHL-B cell survival. (A) EMSA analysis of NF-κB protein binding to the BLYS promoter. Nuclear extracts from NHL-B cells were transfected with dominant-negative (DN) NF-κB or control plasmid and analyzed with an oligonucleotide probe for the BLYS–NF-κB binding site. (B) Immunoblot analysis of BLyS expression in NHL-B (LBCL-MS) cells transfected with DN NF-κB or control plasmid. Actin was used as loading control. BLyS levels were normalized to those of actin as previously described and presented as relative fold decrease compared to control samples. (C) EMSA analysis of NF-κB protein binding to the BLYS promoter in NHL-B (MCL-SP53) cells treated with various doses of the IκB inhibitor BAY11-7082. Lamin B was used as nuclear protein loading control. (D) Immunoblot analysis of BLyS in NHL-B (MCL-SP53) cells treated with various doses of IκB inhibitor BAY11-7082. (E) Immunoblot analysis for BLyS, p52, and Rel-B expression in NHL-B (LBCL-MS) cells treated with 100 nM p52 or Rel-B siRNA. Actin was used as loading control. (F) EMSA analysis of NF-κB binding to the BLYS promoter. Nuclear extracts from an NHL-B cell line (LBCL-MS) were transfected with BLYS or control siRNA and analyzed with an oligonucleotide probe for the BLYS–NF-κB binding site. Lamin B was used as nuclear protein loading control. (G) Immunoblot analysis of phosphorylated IκBα (pIκBα) and p52 in NHL-B cells transfected with BLYS or control siRNA. pIκBα and p52 protein expression levels were normalized to those of actin as previously described in panel B.
Constitutive BLyS expression through the NF-κB pathway activates a positive feedback loop contributing to NHL-B cell survival. (A) EMSA analysis of NF-κB protein binding to the BLYS promoter. Nuclear extracts from NHL-B cells were transfected with dominant-negative (DN) NF-κB or control plasmid and analyzed with an oligonucleotide probe for the BLYS–NF-κB binding site. (B) Immunoblot analysis of BLyS expression in NHL-B (LBCL-MS) cells transfected with DN NF-κB or control plasmid. Actin was used as loading control. BLyS levels were normalized to those of actin as previously described and presented as relative fold decrease compared to control samples. (C) EMSA analysis of NF-κB protein binding to the BLYS promoter in NHL-B (MCL-SP53) cells treated with various doses of the IκB inhibitor BAY11-7082. Lamin B was used as nuclear protein loading control. (D) Immunoblot analysis of BLyS in NHL-B (MCL-SP53) cells treated with various doses of IκB inhibitor BAY11-7082. (E) Immunoblot analysis for BLyS, p52, and Rel-B expression in NHL-B (LBCL-MS) cells treated with 100 nM p52 or Rel-B siRNA. Actin was used as loading control. (F) EMSA analysis of NF-κB binding to the BLYS promoter. Nuclear extracts from an NHL-B cell line (LBCL-MS) were transfected with BLYS or control siRNA and analyzed with an oligonucleotide probe for the BLYS–NF-κB binding site. Lamin B was used as nuclear protein loading control. (G) Immunoblot analysis of phosphorylated IκBα (pIκBα) and p52 in NHL-B cells transfected with BLYS or control siRNA. pIκBα and p52 protein expression levels were normalized to those of actin as previously described in panel B.
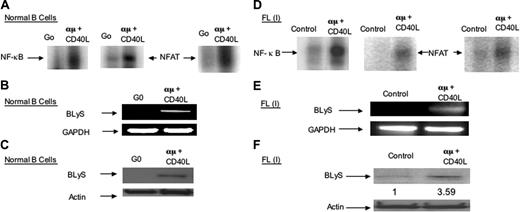
Induction of cellular NF-κB and NFAT activation leads to BLyS protein expression in normal B lymphocytes and low-grade follicular lymphoma cells
In activated normal peripheral B cells (α-μ and soluble CD154 [CD40L] treated), we detected binding of both NF-κB and NFAT proteins to the BLYS promoter by EMSA analysis (Figure 6A). BLyS mRNA and protein expression were enhanced in activated B cells in contrast to nonstimulated (G0) B cells (Figure 6B,C). Similar results were obtained in low-grade (grade I) follicular lymphoma (FL) patient biopsy cells (Figure 6D-F). These results indicate that both NF-κB and NFAT binding to the BLYS promoter are involved in induction of BLyS expression and that indolent (low-grade) NHL-B such as FL show a similar pattern of increased BLyS expression after exogenous cellular activation, in contrast to aggressive NHL-B, where BLYS is constitutively active (Figure 1).
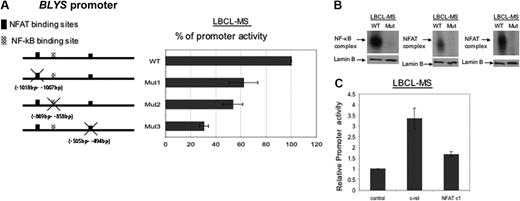
Both NF-κB and NFAT binding sites in the BLyS promoter are important for its functional activity
To determine whether BLyS expression requires the activation of both NF-κB and NFAT, NHL-B cells were transfected with pGL4 luciferase reporter plasmids containing either wild-type or mutated BLYS promoters. Luciferase assays were used to evaluate the transcriptional activity of the BLYS promoter. The experiments showed that mutation of the NF-κB and NFAT binding sites in the BLYS promoter leads to decreased promoter activity (Figure 7A). To further evaluate whether mutations in the BLYS promoter can inhibit NF-κB or NFAT binding, EMSA analyses were performed. The results showed that NF-κB and NFAT binding to the BLYS promoter was decreased when their binding sites were mutated (Figure 7B). Since c-Rel and NFATc1 are major components in NF-κB and NFAT binding complexes, respectively, that bind to the BLYS promoter (Figure 3), c-Rel or NFAT c1 expression vectors were transfected into NHL-B cell (LBCL-MS), and BLYS promoter activity was determined in a luciferase assay. The results showed that BLYS promoter activity was increased about 3-fold in the NHL-B cells overexpressing c-Rel, and 0.5 fold in NHL-B cells overexpressing NFATc1, compared to NHL-B cells transfected with a control vector. These findings indicate that the putative NF-κB and NFAT binding sites on the BLYS promoter are functional, and probably necessary, and sufficient for the regulation of BLyS expression in this type of NHL-B.
Inhibition of NFAT activity reduces BLyS protein expression in NHL-B cells. (A) EMSA analysis of NFAT protein binding to BLYS promoter. Nuclear extracts from NHL-B (LBCL-MS) cells were transfected with dominant-negative (DN) NFAT or control plasmid and analyzed with oligonucleotide probes from the 2 BLYS-NFAT binding sites. NFAT binding levels were analyzed by BioMax 1D software, presented as before, as relative fold decrease compared to control samples. Lamin B was used as nuclear protein loading control. (B) Immunoblot analysis of BLyS expression in NHL-B (LBCL-MS) cells transfected with DN NFAT or control plasmid. Actin is used as loading control. BLyS protein levels were analyzed by BioMax 1D software, normalized with actin levels as before, and presented as before. (C) EMSA analysis of NFAT binding to the BLYS promoter in a representative NHL-B cell line (MCL-SP53). Nuclear extracts from NHL-B (MCL-SP53) cells treated with cyclosporine A (CsA) were analyzed with oligonucleotide probes from the 2 BLYS-NFAT sites to detect NFAT binding activity. NFAT binding levels were analyzed as previously described in panel A. Similar results observed in LBCL-MS cells too (data not shown). (D) Immunoblot analysis of BLyS protein in NHL-B (MCL-SP53) cells treated various doses of CsA. Actin was used as loading control. BLyS protein expression levels were analyzed as previously described in panel B. Similar results observed in LBCL-MS cells too.
Inhibition of NFAT activity reduces BLyS protein expression in NHL-B cells. (A) EMSA analysis of NFAT protein binding to BLYS promoter. Nuclear extracts from NHL-B (LBCL-MS) cells were transfected with dominant-negative (DN) NFAT or control plasmid and analyzed with oligonucleotide probes from the 2 BLYS-NFAT binding sites. NFAT binding levels were analyzed by BioMax 1D software, presented as before, as relative fold decrease compared to control samples. Lamin B was used as nuclear protein loading control. (B) Immunoblot analysis of BLyS expression in NHL-B (LBCL-MS) cells transfected with DN NFAT or control plasmid. Actin is used as loading control. BLyS protein levels were analyzed by BioMax 1D software, normalized with actin levels as before, and presented as before. (C) EMSA analysis of NFAT binding to the BLYS promoter in a representative NHL-B cell line (MCL-SP53). Nuclear extracts from NHL-B (MCL-SP53) cells treated with cyclosporine A (CsA) were analyzed with oligonucleotide probes from the 2 BLYS-NFAT sites to detect NFAT binding activity. NFAT binding levels were analyzed as previously described in panel A. Similar results observed in LBCL-MS cells too (data not shown). (D) Immunoblot analysis of BLyS protein in NHL-B (MCL-SP53) cells treated various doses of CsA. Actin was used as loading control. BLyS protein expression levels were analyzed as previously described in panel B. Similar results observed in LBCL-MS cells too.
Induction of cellular NF-κB and NFAT activation leads to BLyS protein expression in normal B lymphocytes and low-grade follicular lymphoma (FL) cells. (A) EMSA analysis of normal G0 and activated peripheral blood B cells using the NF-κB or NFAT binding site oligonucleotides from the BLYS promoter. (B) RT-PCR analysis of BLyS expression in normal peripheral blood B cells. (C) Western blot analysis of BLyS in normal peripheral blood B cells. (D) EMSA analysis of tumor cells from a patient with follicular lymphoma (> 90% small cleaved cells: grade 1 FL) using oligonucleotide probes from BLYS-NF-κBor BLYS-NFAT binding sites on the BLYS promoter. (E) RT-PCR analysis of BLyS expression in the FL cells (described in panel D). (F) Western blot analysis of BLyS expression in follicular lymphoma (small cleaved cell lymphoma, grade 1) patient biopsy cells. Actin was used as loading control. BLyS protein expression levels were analyzed by BioMax 1D software as before.
Induction of cellular NF-κB and NFAT activation leads to BLyS protein expression in normal B lymphocytes and low-grade follicular lymphoma (FL) cells. (A) EMSA analysis of normal G0 and activated peripheral blood B cells using the NF-κB or NFAT binding site oligonucleotides from the BLYS promoter. (B) RT-PCR analysis of BLyS expression in normal peripheral blood B cells. (C) Western blot analysis of BLyS in normal peripheral blood B cells. (D) EMSA analysis of tumor cells from a patient with follicular lymphoma (> 90% small cleaved cells: grade 1 FL) using oligonucleotide probes from BLYS-NF-κBor BLYS-NFAT binding sites on the BLYS promoter. (E) RT-PCR analysis of BLyS expression in the FL cells (described in panel D). (F) Western blot analysis of BLyS expression in follicular lymphoma (small cleaved cell lymphoma, grade 1) patient biopsy cells. Actin was used as loading control. BLyS protein expression levels were analyzed by BioMax 1D software as before.
Both NF-κB and NFAT binding sites in the BLyS promoter are important for its activity. (A) Diagram of the BLYS promoter showing locations of site-directed mutagenesis. Luciferase activity in NHL-B (LBCL-MS) cells that had been transfected with wild-type, NF-κB, or NFAT mutant BLYS promoter-luciferase reporter constructs. (B) EMSA analysis of NF-kB or NFAT binding levels in NHL-B (LBCL-MS) cells incubated with wild-type BLYS–NF-κB or BLYS-NFAT binding site oligonucleotide probes or the corresponding mutant oligonucleotide probes from the BLYS promoter. Lamin B is used as nuclear extract loading control. (C) Luciferase activity in NHL-B (LBCL-MS) cells that had been transfected with control vector, c-rel expression vector, or NFATc1 expression vector. The error bars in panels A and C indicate the standard deviation of triplicate samples.
Both NF-κB and NFAT binding sites in the BLyS promoter are important for its activity. (A) Diagram of the BLYS promoter showing locations of site-directed mutagenesis. Luciferase activity in NHL-B (LBCL-MS) cells that had been transfected with wild-type, NF-κB, or NFAT mutant BLYS promoter-luciferase reporter constructs. (B) EMSA analysis of NF-kB or NFAT binding levels in NHL-B (LBCL-MS) cells incubated with wild-type BLYS–NF-κB or BLYS-NFAT binding site oligonucleotide probes or the corresponding mutant oligonucleotide probes from the BLYS promoter. Lamin B is used as nuclear extract loading control. (C) Luciferase activity in NHL-B (LBCL-MS) cells that had been transfected with control vector, c-rel expression vector, or NFATc1 expression vector. The error bars in panels A and C indicate the standard deviation of triplicate samples.
Discussion
Both in vivo and in vitro studies have demonstrated that the TNF receptor ligand BLyS promotes B-lymphocyte maturation, survival, and at least the early stages of cell-cycle progression.1-5,10,19 Abnormally expressed BLyS protein has been observed in a variety of malignant cells of the B-cell lineage.9,12,13 However, the transcriptional regulation of BLYS has been little studied to date. In this study, we have demonstrated that expression of BLyS protein both in normal B cells and NHL-B cells is transcriptionally regulated by 2 critical families of transcription factors, NF-κB and NFAT. Constitutive activation of NF-κB and NFAT in aggressive NHL-B induces abnormal BLyS expression through one NF-κB and 2 NFAT binding sites in the BLYS promoter. In addition, BLyS signaling and NF-κB expression appear to form a positive feedback loop that contributes to prolonged or continuous malignant B-cell survival and diminished tumor cell death in the malignant B cell.
Various studies also have shown that inhibiting BLyS through use of decoy receptors or blocking antibodies restores the apoptotic process in malignant B cells.6,9,12,13 However, it has been unclear as to whether constitutive BLyS expression is directly involved in malignant B-cell survival. We have shown that BLyS protein is constitutively expressed in aggressive NHL-B cell lines (LBCL and MCL), as well as in tumor cells from NHL-B patient biopsies, but, as expected, the expression level of BLyS in the tumor cells varies quantitatively. We also show the presence of cell surface bound BLyS in LBCL and MCL cell lines, as well as LBCL and MCL NHL-B patient biopsy cells, that not only confirmed the data shown by another group,12 but also further indicates that constitutively expressed BLyS protein can bind to malignant B cells, promoting their survival (Figure 1). This hypothesis also was confirmed by our demonstration that neutralization of BLyS protein by specific BLyS antibody decreases LBCL and MCL cells survival (Figure 2A,B) in vitro. Our data also indicate that direct inhibition of constitutive BLyS expression in NHL-B (LBCL) cells using BLYS-specific siRNA decreases the expression of antiapoptotic Bcl-2 family members (Bcl-2 and Bcl-xL) and cell cycle progression promoting molecules (cyclin D1 and c-myc), leading to reduced proliferative activity and apoptosis in NHL-B cells (Figure 2). These data show that in addition to Burkitt lymphoma (BL),12 constitutive expression of BLyS is crucial for the survival of other histotypes of NHL-B cells, such as LBLC and MCL, through activation of similar survival pathways previously reported in normal B cells treated with BLyS protein in vitro.19 Our findings also identify survival pathways that are induced by BLyS in these NHL-B cells.
Several groups have reported that BLyS is expressed by various cell types in the immune system1-5,14,15 as well as in multiple types of malignant B cells, including multiple myeloma cells.9,12,13 However, the nature of BLyS protein regulation and expression is still poorly understood. A number of studies have shown that in aggressive NHL-B cells, NF-κB is constitutively activated and mediates neoplastic B-cell growth and cell survival.30-33 Recent studies from our lab and from others have shown that activated NFAT expression also is detected in malignant B cells,43,44 suggesting an important role for NFAT in malignant B-cell growth and survival. Previous studies by other investigators showed that BLyS expression was increased in EBV LMP1–positive BJAB (BL) cells due to constitutive NF-κB activation,11 but whether NF-κB regulates BLyS expression in LMP1-negative NHL-B cells was not clear. Also, a binding site for NF-κBonthe BLYS promoter was not identified. Our data not only demonstrate that BLyS is a key molecule for tumor cell survival and proliferation in aggressive NHL-B, but also address the issues of whether NF-κB and NFAT family members induce BLyS expression in malignant B cells. We have identified one putative NF-κB binding site and 2 NFAT binding sites in the BLYS promoter that are constitutively bound by activated NF-κB or NFAT in aggressive NHL-B cells (Figures 3, 7). Further studies showed that inhibiting transactivation of NF-κB (NF-κB1 and NF-κB2) or NFAT results in decreased BLyS protein expression, suggesting that constitutive activation of both NF-κB and NFAT are important for sustained BLyS protein expression in NHL-B cells (Figures 4, 5). We also found that BLyS expression is induced by activation of the NF-κB and NFAT pathways in normal peripheral blood (Go) B cells and in cells from a patient with indolent follicular (small cleaved cell) lymphoma, further confirming the importance of NF-κB and NFAT in the induction of BLyS expression in normal and low-grade malignant B cells (Figure 6).
Previous studies in another laboratory also have shown that CD40L stimulation induces expression of BLyS protein in normal Go B cells and increases BLyS expression in BL,12 but the underlying mechanism of these observations has been unclear. Our study shows that stimulation with exogenous CD40L (CD154) and anti-IgM induces BLyS expression in normal human B cells by activating both NF-κB and NFAT binding to the BLYS promoter. This finding supports our contention that NF-κB and NFAT are important regulators of BLyS protein expression and delineates a mechanism by which BLyS expression is induced in normal B cells in vitro after CD40L stimulation. Similarly, we found that BLyS expression can be induced in vitro by CD40L and anti-IgM stimulation in grade 1, follicular B-cell lymphoma patient biopsy cells, suggesting that in this low-grade (indolent) B-cell lymphoma, NF-κB and NFAT activation also can induce BLyS expression. These findings suggest that this type of low-grade NHL-B also depends on exogenous activation of the CD40/NF-κB pathway, retaining similarity in this respect to normal B cells, that require exogenous activation rather than endogenous (constitutive) activation of BLyS, as observed in aggressive NHL-B cells (Figure 1).
The full neoplastic phenotype in NHL-B cells cannot be accounted for by the translocation of a single dominant oncogene and/or the inactivation of a tumor suppressor gene(s), characteristic of these lymphomas, suggesting that undefined cellular abnormalities, in addition to the well-defined nonrandom chromosomal translocations, are required for attaining the transformed state and are also involved in the pathogenesis.46,47 We have previously shown that abnormal CD40L/CD40 signaling and constitutive NF-κB activation are involved in the pathogenesis of aggressive NHL-B in an interdependent manner.32,33 Several groups have reported that in normal mature murine and human B cells, BLyS signaling stimulates both the NF-κB1 and NF-κB2 pathways through one or more of the 3 BLyS receptors: BAFF-R, TACI, and BCMA.6-8,27,28,35,38 However, whether both the NF-κB1 and NF-κB2 pathways are involved individually or together in BLyS-mediated survival in NHL-B cells has not been addressed. Our studies have shown that all 3 BLyS receptors are expressed in NHL-B cells at various levels (data not shown). These observations suggest that in aggressive NHL-B cells, BLyS induces cell survival through an autonomous signaling pathway. Our data also show that inhibition of BLyS protein expression by BLYS siRNA decreases the DNA-binding activity of various NF-κB components such as p50, p52, and c-Rel, as well as the level of pIκB and p52 protein, demonstrating that constitutive expression of BLyS is important for maintaining endogenous activation of both the NF-κB1 and NF-κB2 signaling pathways in NHL-B cells (Figure 4D,E).
Based on our findings, we suggest that in addition to constitutive CD40L expression, in aggressive NHL-B cells, abnormal BLyS signaling and NF-κB activity form a positive feedback loop. NF-κB activation induces BLyS expression, while the up-regulated BLyS ligand is in turn involved in maintaining constitutive NF-κB activation, after cognate receptor binding. We hypothesize that such a positive feedback loop then contributes to sustained NHL-B cell survival and neoplastic cell proliferation. Delineating the specific molecular mechanisms involved in generating this positive feedback loop will be crucial in elucidating further mechanism(s) in NHL-B pathogenesis and could provide future therapeutic targets for aggressive NHL-B.
Prepublished online as Blood First Edition Paper, February 23, 2006; DOI 10.1182/blood-2005-10-4042.
Supported by National Cancer Institute grants CA-R01-100836 (R.J.F.) and CA-16672-26 and grants from the Lymphoma Research Foundation of New York City (R.J.F.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

![Figure 2. Constitutive BLyS expression contributes to NHL-B cell survival in vitro. (A) XTT proliferation assay of NHL-B (LBCL-MS, MCL-Jeko) cells treated with control IgG or BLyS antibody. The number of live cells was monitored by the absorbance of 490 nm wavelength. (B) TUNEL analysis of NHL-B (LBCL-MS) cells treated with control IgG or BLyS antibody. Free DNA fragments in apoptotic cells were labeled with green fluorescence. (C) Proliferation of NHL-B (LBCL-MS) cells transfected with BLYS siRNA or control nontargeting sequence. DNA synthesis was assessed by [3H]thymidine uptake in vitro. (D) Immunoblot analysis of BLyS protein in NHL-B (LBCL-MS) cells transfected with BLYS siRNA or control siRNA. Actin was used as loading control. The BLyS level was analyzed by BioMax 1D software, normalized with actin levels, and presented as relative fold decrease compared to control samples. (E) TUNEL analysis of NHL-B (LBCL-MS) cells transfected with BLYS siRNA or a control siRNA. Free DNA fragments in apoptotic cells were labeled with green fluorescence. (F) Caspase-3 activity in an NHL-B (LBCL-MS) cell line transfected with BLYS or control siRNA. (G) Immunoblot analysis of Bcl-2 and Bcl-xL in NHL-B (LBCL-MS) cells transfected with BLYS or control siRNA. Bcl-2 and Bcl-xL levels were normalized to those of actin previously described in D. (H) Immunoblot analysis of BLyS, c-myc, and cyclin D1 in NHL-B cell line cells transfected with BLYS or control siRNA. Actin was used as loading control. The BLyS, c-myc, and cyclin D1 levels were normalized to those of actin as previously described in panel D. The data in panels A, C, and F are representative of 2 independent experiments. The error bars indicate standard deviation of triplicate samples.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/107/11/10.1182_blood-2005-10-4042/4/m_zh80110696510002.jpeg?Expires=1769137320&Signature=ewSTohPydszb7P5nPM5agNxM-PjakWPx4G7v4Z4lGq55BV6n1kk3lXWQ9bv~VyeZgJj5fuOqF9vIQuPSO~3bSc64ZspQ3MilB3b~VdH25lR23Cy-dkUmpX6dTsZCN-7B43QFg2mroal395LQrj-sbViHQxAHXIae~OvsSAjfyk~AR2OqyL--k3mc8qU22qHKPjYJ3wKqL5YNiib2ikTiDh1LoQ7w~lqBjm9ZgiCuXJT7QdTW7DPjyLq-DXv0z0mpYKjG7qKA4apGvJM5p9a5~eMuUZGWnosiOySvJ01H3IRgrMdquSMirSGDR2wDPagf9oFi2TwMeVVcalgxKhDJVQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal