Abstract
Treatment-related toxicity in acute lymphoblastic leukemia (ALL) can not only be life threatening but may also affect relapse risk. In 240 patients, we determined whether toxicities were related to 16 polymorphisms in genes linked to the pharmacodynamics of ALL chemotherapy, adjusting for age, race (self-reported or via ancestry-informative markers), sex, and disease risk group (lower- vs higher-risk therapy). Toxicities (gastrointestinal, infectious, hepatic, and neurologic) were assessed in each treatment phase. During the induction phase, when drugs subject to the steroid/cytochrome P4503A pathway predominated, genotypes in that pathway were important: vitamin D receptor (odds ratio [OR], 6.85 [95% confidence interval [CI], 1.73-27.0]) and cytochrome P4503A5 (OR, 4.61 [95% CI, 1.11-19.2]) polymorphisms were related to gastrointestinal toxicity and infection, respectively. During the consolidation phase, when antifolates predominated, the reduced folate carrier polymorphism predicted gastrointestinal toxicity (OR, 10.4 [95% CI, 1.35-80.4]) as it also did during continuation (OR, 2.01 [95% CI, 1.06-4.11]). In all 3 treatment phases, a glucuronosyltransferase polymorphism predicted hyperbilirubinemia (P = .017, P < .001, and P < .001) and methotrexate clearance (P = .028), which was also independently associated with hyperbilirubinemia (P = .026). The genotype-phenotype associations were similar whether analyses were adjusted by self-reported race or ancestry-informative genetic markers. Germ-line polymorphisms are significant determinants of toxicity of antileukemic therapy.
Introduction
Acute lymphoblastic leukemia (ALL) is cured in approximately 80% of children with multiagent chemotherapeutic regimens.1–4 Treatment-related toxicity can not only be life threatening5,6 but is also one of the main reasons for interruption or discontinuation of chemotherapy, which may increase relapse risk. Moreover, adverse events affect the quality of life for patients during and after cancer therapy.7–10 Prediction of toxicity is difficult, because of wide interpatient variation in pharmacokinetics and pharmacodynamics of antileukemic agents. A trial-and-error approach to dosing is not optimal due to delay between dosing and toxicity, and because the same toxicity (eg, myelosuppression) can be attributable to multiple drugs.
The extent to which genetic predisposition influences risk of common toxicities is not clear. Toxicity from anticancer drugs can be affected by inherited polymorphisms in genes that encode drug-metabolizing enzymes, transporters, targets, and receptors.11–14 Although we and others have assessed whether germ-line polymorphisms relate to antileukemic agent toxicity,15–18 most prior studies have focused on few polymorphisms and very specific toxicities, and did not assess the influence of gene-gene interactions. Moreover, many studies failed to account for confounding factors such as age, sex, race, and differences in chemotherapeutic regimens.9,19–21
Herein, we used a candidate-gene approach, adjusting for confounding factors, to determine whether all common therapy-induced toxicities (gastrointestinal toxicity, infection, hyperbilirubinemia, and neurotoxicity) were related to 16 common polymorphisms in genes involved in the pharmacodynamics of ALL therapy. We also assessed whether pathway-oriented groupings of these genetic polymorphisms were useful. These results are interpreted in the context of our prior analysis of genes influencing relapse risk.22
Patients, materials, and methods
Patients
Of 247 children with newly diagnosed ALL treated on the Total XIIIB study23 at St Jude Children's Research Hospital, 240 were evaluable herein. We excluded one patient who died shortly after diagnosis and did not have a remission DNA sample, 5 patients with Down syndrome, and 1 patient with cystic fibrosis because their underlying diseases can influence toxicity.24,25 The study was approved by St Jude Children's Research Hospital's institutional review board, and informed consent was obtained from parents, guardians, or patients (as appropriate), in accordance with the Declaration of Helsinki. Patients were prospectively assigned to 1 of 2 treatment groups based upon relapse risk (lower or higher/intermediate). Of the 240 evaluable patients, 3 patients came off study due to toxicity; 30 patients were censored prior to the end of treatment because of relapse (n = 8), second cancer (n = 3), stem cell transplantation (n = 3), induction failure (n = 3), or other reasons (n = 13). However, for each treatment phase, all patients were included in the analysis up to time of censoring.
Upon admission, patients (or their parents) were asked to declare their “race” according to institutional guidelines including black, white, Asian, and other. Therapy was divided into 3 phases: 8 weeks of remission induction, 2 weeks of consolidation, and 120 weeks of continuation therapy (including a reinduction phase at weeks 16-21) as described.23 Remission induction consisted of “window” therapy with mercaptopurine, alone or combined with low- or high-dose methotrexate, followed 4 days later by prednisone, vincristine, daunorubicin, asparaginase, cytarabine, and etoposide. Consolidation treatment comprised high-dose methotrexate and mercaptopurine. Continuation treatment differed by risk groups: the lower-risk arm received mercaptopurine plus methotrexate with pulses of dexamethasone plus vincristine; the higher-risk arm received drug pairs rotating weekly: etoposide plus cyclophosphamide, mercaptopurine plus methotrexate, methotrexate plus cytarabine, dexamethasone plus vincristine, and etoposide plus cytarabine. Patients at higher risk of central nervous system relapse received extra intrathecal therapy and cranial irradiation at weeks 56 to 57 of continuation treatment. Methotrexate plasma clearance was estimated following each course of high-dose methotrexate (PA134711664; http://pharmgkb.org26 ), leucovorin dosage was adjusted based on plasma methotrexate concentrations as described,27 and the per-patient average clearance during consolidation and continuation treatment was analyzed. Standard supportive care included the use of 3-day-a-week oral trimethoprim/sulfamethoxazole as the only antimicrobial prophylaxis and ondansetron as the primary antiemetic; use of filgrastim and antifungal prophylaxis was rare.
Toxicities
Toxicities were graded using NCI Common Toxicity Criteria version 1.0 and included the most common toxicities: gastrointestinal (stomatitis or diarrhea), infection, hyperbilirubinemia, and neurotoxicity (Table 1). For analyses, toxicity grades were used to dichotomize toxicities as “present” versus “absent,” with grade 3 to 4 or grade 2 to 3 toxicities considered as present, depending on phase, as defined in Table 1. Neurotoxicity was divided into vincristine-related peripheral neuropathy (eg, constipation, neurosensory, and neuromotor) or methotrexate-related central nervous system toxicity (cerebellar or cortical).
Frequencies of toxicity included in analyses by treatment phase
| Treatment phase . | Toxicity . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gastrointestinal . | Infection . | Hyperbilirubinemia . | Peripheral neuropathy . | Central nervous system . | |||||||||
| Grade 3 . | Grade 4 . | Grade 3 . | Grade 4 . | Grade 2 . | Grade 3 . | Grade 4 . | Grade 2 . | Grade 3 . | Grade 4 . | Grade 2 . | Grade 3 . | Grade 4 . | |
| Induction, total no. of patients* with toxicity | 14 | 2 | 28 | 7 | 49 | 17 | 6 | — | 8 | 0 | 0† | 2† | 0† |
| Consolidation, total no. of patients* with toxicity | 16 | 3 | 7 | 0 | 21 | 5 | 0 | 3† | 1† | 0† | 0† | 2† | 0† |
| Continuation, total no. of episodes (no. of patients*) | 61 (41) | 9 (7) | 97 (62) | 21 (18) | — | 59 (34) | 12 (9) | — | 43 (29) | 1 (1) | — | 7 (6) | 23 (13) |
| Continuation, total no. of episodes of toxicity/wk at risk | 0.002866 | 0.000423 | 0.004558 | 0.000987 | — | 0.00277 | 0.0005 | 0.004981 | 0.0020 | 0.00004 | 0.00004 | 0.0003 | 0.00108 |
| Continuation, total no. of patients with toxicity/wk at risk | 0.001926 | 0.000329 | 0.002913 | 0.000846 | — | 0.00159 | 0.0004 | 0.002772 | 0.0013 | 0.00004 | 0.00004 | 0.0002 | 0.00108 |
| Treatment phase . | Toxicity . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gastrointestinal . | Infection . | Hyperbilirubinemia . | Peripheral neuropathy . | Central nervous system . | |||||||||
| Grade 3 . | Grade 4 . | Grade 3 . | Grade 4 . | Grade 2 . | Grade 3 . | Grade 4 . | Grade 2 . | Grade 3 . | Grade 4 . | Grade 2 . | Grade 3 . | Grade 4 . | |
| Induction, total no. of patients* with toxicity | 14 | 2 | 28 | 7 | 49 | 17 | 6 | — | 8 | 0 | 0† | 2† | 0† |
| Consolidation, total no. of patients* with toxicity | 16 | 3 | 7 | 0 | 21 | 5 | 0 | 3† | 1† | 0† | 0† | 2† | 0† |
| Continuation, total no. of episodes (no. of patients*) | 61 (41) | 9 (7) | 97 (62) | 21 (18) | — | 59 (34) | 12 (9) | — | 43 (29) | 1 (1) | — | 7 (6) | 23 (13) |
| Continuation, total no. of episodes of toxicity/wk at risk | 0.002866 | 0.000423 | 0.004558 | 0.000987 | — | 0.00277 | 0.0005 | 0.004981 | 0.0020 | 0.00004 | 0.00004 | 0.0003 | 0.00108 |
| Continuation, total no. of patients with toxicity/wk at risk | 0.001926 | 0.000329 | 0.002913 | 0.000846 | — | 0.00159 | 0.0004 | 0.002772 | 0.0013 | 0.00004 | 0.00004 | 0.0002 | 0.00108 |
— indicates that this grade of event was not considered toxic for this phase.
The number of patients or episodes of toxicity were analyzed, broken down by NCI grade and phase; for example, for hyperbilirubinemia during induction or consolidation, grades 2, 3, and 4 episodes were considered as toxic, whereas for continuation, only grades 3 and 4 episodes were considered as toxic for purposes of the analyses. The total numbers of the patients at risk were 240, 239, and 237 during the induction, consolidation, and continuation phases, respectively.
Not analyzed statistically because of too few events.
For remission induction, time at risk was from beginning of therapy until start of consolidation treatment. For consolidation phase, time at risk was from the start of consolidation until 4 weeks after completion of consolidation, or until start of continuation therapy, whichever came first. During these 2 phases, if a patient experienced multiple episodes of the same toxicity, the highest grade for that phase was used in the analysis. For toxicity occurring during continuation treatment, time at risk was from the beginning of continuation until 2 weeks after the end of therapy. Patients were censored at time of withdrawal from protocol treatment for any reason.
Genotyping
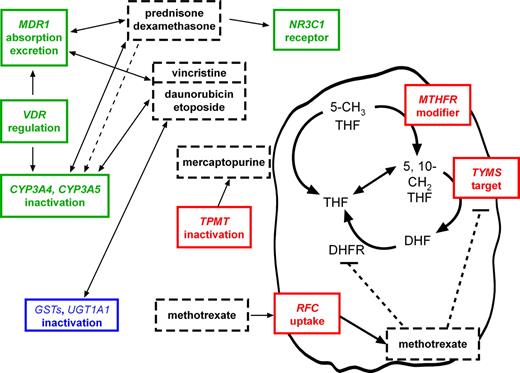
DNA was extracted from normal blood cells using samples that were collected after the successful completion of remission induction in nearly all cases. Polymorphisms in candidate genes encoding proteins involved in pharmacokinetics or pharmacodynamics of antileukemic agents (Figure 1) have previously been linked to a functional phenotype in vivo or in vitro; genotyping for 16 polymorphic loci (CYP3A4*1B [A>G at position −392] and CYP3A5*3 [G>A at position 22893], GSTP1 313A>G, GSTM1 deletion, GSTT1 deletion, MDR1 exon 21 [2677G>T/A], MDR1 exon 26 [3435C>T], MTHFR 677C>T, MTHFR 1298A>C, NR3C1 1088A>G, RFC [SLC19A1] 80A>G, TPMT [238G>C, 460G>A, 719A>G], TYMS enhancer repeat, UGT1A1 promoter repeat, VDR intron 8 G>A, and VDR FokI [start site] T>C) was performed as described22 and was 100% successful.
The interactions of antileukemic agents with gene products. Antileukemic agents (dashed boxes) interact with gene products typed in this study (genes italicized, with their functions indicated in the colored boxes). Bidirectional arrows indicate that the drugs are both substrates for and competitive inhibitors of the indicated gene products; dashed arrow indicates inductive effect of steroids on CYP3A enzymes; flat-headed arrows indicate inhibitory effects. Genotypes were determined at loci in the indicated genes and analyzed individually; they were also pooled into 1 of 3 major groups: glucocorticoid (green), phase II conjugating (blue), and antimetabolite related (red).
The interactions of antileukemic agents with gene products. Antileukemic agents (dashed boxes) interact with gene products typed in this study (genes italicized, with their functions indicated in the colored boxes). Bidirectional arrows indicate that the drugs are both substrates for and competitive inhibitors of the indicated gene products; dashed arrow indicates inductive effect of steroids on CYP3A enzymes; flat-headed arrows indicate inhibitory effects. Genotypes were determined at loci in the indicated genes and analyzed individually; they were also pooled into 1 of 3 major groups: glucocorticoid (green), phase II conjugating (blue), and antimetabolite related (red).
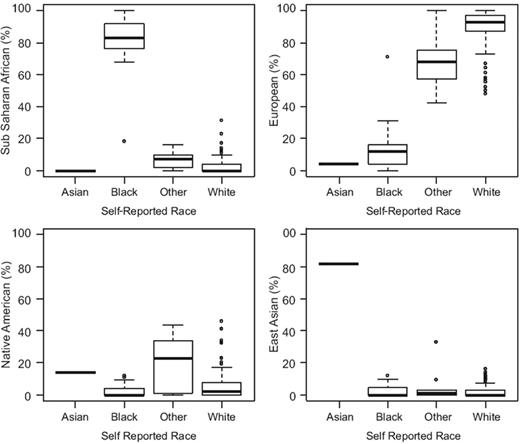
Ancestry-informative markers (AIMs) were genotyped by DNAPrint Genomics (Sarasota, FL) and used 176 autosomal genetic markers with large allele frequency differences between populations to estimate the biogeographic ancestry for each individual. The results are reported as estimated percentage of Sub-Saharan African, European, Native American, and East Asian28 (Figure 2).
Concordance of self-reported and AIMs-determined race. Percentage of Sub-Saharan African, European, Native American, and East Asian ancestry as determined by AIMs (y-axes) plotted by self-reported race categories (x-axes); black, n = 44; white, n = 167; Asian, n = 1; and other, n = 28. Boxes indicate quartiles, horizontal bars indicate medians, and whiskers indicate the range after excluding outliers (circles).
Concordance of self-reported and AIMs-determined race. Percentage of Sub-Saharan African, European, Native American, and East Asian ancestry as determined by AIMs (y-axes) plotted by self-reported race categories (x-axes); black, n = 44; white, n = 167; Asian, n = 1; and other, n = 28. Boxes indicate quartiles, horizontal bars indicate medians, and whiskers indicate the range after excluding outliers (circles).
Statistical analysis
Genotypes for each polymorphic locus were placed in binary groups for statistical analysis as described.22 The percentage of patients in the less common genotypic group at each locus ranged from 3.3% to 48.8% (median, 31.7%; Table 2). Except for the continuation phase, toxicity was regarded as a dichotomous variable. Exact chi-square tests were used to examine the association between self-reported or AIMs-determined race, age, or upfront treatment-arm categories (mercaptopurine, mercaptopurine plus high-dose methotrexate, mercaptopurine plus low-dose methotrexate, or none) and each type of toxicity. Exact tests were used to examine the association between sex (142 male, 98 female) or risk category (126 on lower risk vs 114 higher risk) and each toxicity. Self-reported race was divided into 4 categories: white (n = 167), black (n = 44), Asian (n = 1), and other (n = 28); race determined by AIMs was reported as a percentage of 4 categories for each patient: Sub-Saharan African, European, Native American, and East Asian; age was treated as 3 categories: younger than 1 year (n = 10), 1 to 10 years (n = 159), and older than 10 years (n = 71).
Percentage of the 240 patients falling into the 2 primary genotypic groups at each of 16 loci
| Locus . | Genotype groups . | % in 1st genotype group . | % in 2nd genotype group . |
|---|---|---|---|
| CYP3A4*1B | AA vs AG and GG | 79.6 | 20.4 |
| CYP3A5*3 | AA and AG vs GG | 32.1 | 67.9 |
| GSTM1 deletion | Null vs nonnull | 42.5 | 57.5 |
| GSTP1 313A>G | AA and AG vs GG | 82.9 | 17.1 |
| GSTT1 deletion | Null vs nonnull | 15.8 | 84.2 |
| MDR1 exon 21 G>T/A | GG vs others | 36.7 | 63.3 |
| MDR1 exon 26 C>T | CC and CT vs TT | 76.3 | 23.7 |
| MTHFR 677C>T | CC vs CT and TT | 48.8 | 51.2 |
| MTHFR 1298A>C | AA vs AC and CC | 53.8 | 46.2 |
| NR3C1 1088A>G | AA vs AG | 96.7 | 3.3 |
| RFC 80A>G | AA and AG vs GG | 68.3 | 31.7 |
| TPMT combined genotypes | Others vs 238GG, 460GG, and 719AA | 5.8 | 94.2 |
| TYMS enhancer repeat | 3AND3 vs others | 31.7 | 68.3 |
| UGT1A1 promoter repeat | 7AND7 vs others | 10.4 | 87.9 |
| VDR Fokl T>C | CC vs CT and TT | 46.3 | 53.7 |
| VDR intron8 G>A | AA and AG vs GG | 54.2 | 45.8 |
| Locus . | Genotype groups . | % in 1st genotype group . | % in 2nd genotype group . |
|---|---|---|---|
| CYP3A4*1B | AA vs AG and GG | 79.6 | 20.4 |
| CYP3A5*3 | AA and AG vs GG | 32.1 | 67.9 |
| GSTM1 deletion | Null vs nonnull | 42.5 | 57.5 |
| GSTP1 313A>G | AA and AG vs GG | 82.9 | 17.1 |
| GSTT1 deletion | Null vs nonnull | 15.8 | 84.2 |
| MDR1 exon 21 G>T/A | GG vs others | 36.7 | 63.3 |
| MDR1 exon 26 C>T | CC and CT vs TT | 76.3 | 23.7 |
| MTHFR 677C>T | CC vs CT and TT | 48.8 | 51.2 |
| MTHFR 1298A>C | AA vs AC and CC | 53.8 | 46.2 |
| NR3C1 1088A>G | AA vs AG | 96.7 | 3.3 |
| RFC 80A>G | AA and AG vs GG | 68.3 | 31.7 |
| TPMT combined genotypes | Others vs 238GG, 460GG, and 719AA | 5.8 | 94.2 |
| TYMS enhancer repeat | 3AND3 vs others | 31.7 | 68.3 |
| UGT1A1 promoter repeat | 7AND7 vs others | 10.4 | 87.9 |
| VDR Fokl T>C | CC vs CT and TT | 46.3 | 53.7 |
| VDR intron8 G>A | AA and AG vs GG | 54.2 | 45.8 |
For the induction and consolidation period, logistic regression was used to test whether toxicity was related to each genotype. For the continuation period, each toxicity event was assumed to be independent, and weighted logistic regression was applied to test the association between genotype and each toxicity event. Because the duration of continuation therapy was extensive, time-at-risk for toxicity was considered. Each episode of toxicity was weighted according to the patient's duration of risk for toxicity by the following formula: Wi = [Zi/max(Zi)]1 − tox, where Zi is cumulative incidence of toxic episodes (of a given type) at time of the ith episode or at the time of censoring, tox = 1 if Zi corresponds to a toxicity episode, and tox = 0 otherwise. Preliminary analyses revealed that some toxicities differed by treatment group or demographic factors (Table S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). Because some of these factors could be confounded by genotypes,29 we performed analyses that did (multivariate) and did not (univariate; Tables S2–S4) adjust for demographic factors and risk groups; only the multivariate results are presented in the main article. In the multivariate analysis, we used multiple logistic regression with treatment groups and demographic factors as covariates.
To investigate whether multigenic genotypes predicted toxicities, we categorized the polymorphisms into 3 functional pathways (Figure 1): glucocorticoid-related genes (CYP3A, MDR1, NR3C1, VDR), phase II conjugating enzyme genes (GSTs, UGT1A1), and antimetabolite-related genes (MTHFR, RFC, TPMT, TYMS), and we defined high, medium, and low “activity” for each of these 3 pathway groupings (Table S5). We performed multivariate weighted logistic regression, adjusting for age, sex, treatment groups, and race, to test whether multigene genotypes affected toxicity.
The stepdown Bonferroni method of Holm was used to assess the statistical significance of the correlations among genotypes.30 The log rank test was used to compare the cumulative incidence of toxicity by genotypic groups. A linear or logistic regression model was used to assess the association between genotypes and methotrexate clearance or between toxicity and methotrexate clearance, respectively.
Results
Self-reported versus AIMs-determined race
Because both genotypes22 and some toxicities (Table S1) differed by race, we further refined assessment of race using percent of biogeographic ancestry based on AIMs (Figure 2). The relationships between candidate genotypes and toxicity were essentially identical whether adjusting for self-reported race or percent ancestry by AIMs (Table 3); hence the odds ratios and P values reported throughout are adjusted for self-reported race.
Toxicities significantly associated with genotypes in a multivariate analysis
| Toxicity, genotype* . | Self-reported race† . | AIMs-determined race‡ . | ||
|---|---|---|---|---|
| Odds ratio (95% confidence limits) . | P . | Odds ratio (95% confidence limits)‡ . | P . | |
| Induction phase | ||||
| Gastrointestinal | ||||
| GSTT1 null vs nonnull | 4.77 (1.4-16.3) | .013 | 5.22 (1.50-18.1) | .009 |
| VDR intron8 GG vs AA or AG | 6.85 (1.73-27.0) | .006 | 6.67 (1.64-25.0) | .008 |
| Infection | ||||
| CYP3A5 GG vs AA or AG | 4.61 (1.11-19.2) | .035 | 5.56 (1.32-25.0) | .019 |
| RFC AA or AG vs GG | 3.25 (1.17-9.07) | .024 | 3.25 (1.16-9.13) | .026 |
| VDR intron8 GG vs AA or AG | 3.14 (1.4-7.09) | .005 | 3.13 (1.39-7.14) | .006 |
| Hyperbilirubinemia | ||||
| GSTM1 null vs nonnull | 1.95 (1.06-3.58) | .032 | 2.00 (1.08-3.69) | .027 |
| UGT1A1 7/7 vs others | 3.05 (1.22-7.64) | .017 | 2.98 (1.19-7.46) | .02 |
| VDR FokI CT or TT vs CC | 1.94 (1.04-3.61) | .036 | 2.00 (1.05-3.70) | .034 |
| VDR intron8 GG vs AA or AG | 1.94 (1.04-3.62) | .037 | 2.00 (1.06-3.85) | .032 |
| Consolidation phase | ||||
| Gastrointestinal | ||||
| RFC AA or AG vs GG | 10.4 (1.35-80.4) | .025 | 10.7 (1.37-82.7) | .024 |
| Hyperbilirubinemia | ||||
| UGT1A1 7/7 vs others | 13.0 (4.1-41.3) | < .001 | 13.4 (4.27-41.9) | < .001 |
| Continuation phase | ||||
| Gastrointestinal | ||||
| RFC AA or AG vs GG | 2.01 (1.06-4.11) | .033 | 2.03 (1.02-4.01) | .042 |
| Hyperbilirubinemia | ||||
| CYP3A5 GG vs AA or AG | 2.67 (1.03-6.94) | .044 | 3.13 (1.16-8.33) | .023 |
| GSTT1 nonnull vs null | 4.18 (1.2-14.7) | .025 | 4.55 (1.22-16.7) | .024 |
| RFC GG vs AA or AG | 2.99 (1.61-5.59) | .001 | 2.70 (1.47-5.0) | .001 |
| TYMS others vs 3/3 | 2.08 (1.01-4.32) | .048 | 2.22 (1.04-4.80) | .038 |
| UGT1A1 7/7 vs others | 17.0 (7.23-39.9) | < .001 | 18.27 (7.82-42.7) | < .001 |
| Peripheral neurotoxicity | ||||
| CYP3A5 AA or AG vs GG | 2.81 (1.24-6.39) | .014 | 2.76 (1.34-5.71) | .006 |
| VDR intron8 AA or AG vs GG | 2.22 (1.06-4.67) | .035 | 2.16 (1.03-4.51) | .042 |
| Central nervous system | ||||
| GSTP1 GG vs AG and AA | 3.32 (1.41-7.81) | .006 | 2.70 (1.18-6.25) | .020 |
| Toxicity, genotype* . | Self-reported race† . | AIMs-determined race‡ . | ||
|---|---|---|---|---|
| Odds ratio (95% confidence limits) . | P . | Odds ratio (95% confidence limits)‡ . | P . | |
| Induction phase | ||||
| Gastrointestinal | ||||
| GSTT1 null vs nonnull | 4.77 (1.4-16.3) | .013 | 5.22 (1.50-18.1) | .009 |
| VDR intron8 GG vs AA or AG | 6.85 (1.73-27.0) | .006 | 6.67 (1.64-25.0) | .008 |
| Infection | ||||
| CYP3A5 GG vs AA or AG | 4.61 (1.11-19.2) | .035 | 5.56 (1.32-25.0) | .019 |
| RFC AA or AG vs GG | 3.25 (1.17-9.07) | .024 | 3.25 (1.16-9.13) | .026 |
| VDR intron8 GG vs AA or AG | 3.14 (1.4-7.09) | .005 | 3.13 (1.39-7.14) | .006 |
| Hyperbilirubinemia | ||||
| GSTM1 null vs nonnull | 1.95 (1.06-3.58) | .032 | 2.00 (1.08-3.69) | .027 |
| UGT1A1 7/7 vs others | 3.05 (1.22-7.64) | .017 | 2.98 (1.19-7.46) | .02 |
| VDR FokI CT or TT vs CC | 1.94 (1.04-3.61) | .036 | 2.00 (1.05-3.70) | .034 |
| VDR intron8 GG vs AA or AG | 1.94 (1.04-3.62) | .037 | 2.00 (1.06-3.85) | .032 |
| Consolidation phase | ||||
| Gastrointestinal | ||||
| RFC AA or AG vs GG | 10.4 (1.35-80.4) | .025 | 10.7 (1.37-82.7) | .024 |
| Hyperbilirubinemia | ||||
| UGT1A1 7/7 vs others | 13.0 (4.1-41.3) | < .001 | 13.4 (4.27-41.9) | < .001 |
| Continuation phase | ||||
| Gastrointestinal | ||||
| RFC AA or AG vs GG | 2.01 (1.06-4.11) | .033 | 2.03 (1.02-4.01) | .042 |
| Hyperbilirubinemia | ||||
| CYP3A5 GG vs AA or AG | 2.67 (1.03-6.94) | .044 | 3.13 (1.16-8.33) | .023 |
| GSTT1 nonnull vs null | 4.18 (1.2-14.7) | .025 | 4.55 (1.22-16.7) | .024 |
| RFC GG vs AA or AG | 2.99 (1.61-5.59) | .001 | 2.70 (1.47-5.0) | .001 |
| TYMS others vs 3/3 | 2.08 (1.01-4.32) | .048 | 2.22 (1.04-4.80) | .038 |
| UGT1A1 7/7 vs others | 17.0 (7.23-39.9) | < .001 | 18.27 (7.82-42.7) | < .001 |
| Peripheral neurotoxicity | ||||
| CYP3A5 AA or AG vs GG | 2.81 (1.24-6.39) | .014 | 2.76 (1.34-5.71) | .006 |
| VDR intron8 AA or AG vs GG | 2.22 (1.06-4.67) | .035 | 2.16 (1.03-4.51) | .042 |
| Central nervous system | ||||
| GSTP1 GG vs AG and AA | 3.32 (1.41-7.81) | .006 | 2.70 (1.18-6.25) | .020 |
First genotype listed had a higher risk of toxicity compared with the second genotype listed.
Odds ratio and P value for genotype predictors of toxicity adjusted for nongenetic predictors of toxicity using self-reported race.
Odds ratio and P value for genotype predictors of toxicity adjusted for nongenetic predictors of toxicity using AIMs-determined race.
Remission induction
Multiple (8) drugs were given and many toxicities were observed over the 8-week period (Table 1). Accordingly, different genotypes were associated with each toxicity: GSTT1-null and VDR intron 8 GG genotypes were significantly associated with gastrointestinal toxicity; CYP3A5, RFC, and VDR intron 8 polymorphisms, with infection; and GSTM1, UGT1A1, VDR FokI, and VDR intron 8 polymorphisms, with hyperbilirubinemia (Table 3; Figure 3).
Odds ratios of experiencing toxicity during therapy. Median (95% confidence intervals) odds ratios of experiencing the indicated toxicity for the 3 phases of therapy for the most predictive genotypes. Odds ratios resulting from multivariate analyses using self-declared race. The genotypes depicted were significantly associated with more than one toxicity or with toxicity in more than one phase of therapy.
Odds ratios of experiencing toxicity during therapy. Median (95% confidence intervals) odds ratios of experiencing the indicated toxicity for the 3 phases of therapy for the most predictive genotypes. Odds ratios resulting from multivariate analyses using self-declared race. The genotypes depicted were significantly associated with more than one toxicity or with toxicity in more than one phase of therapy.
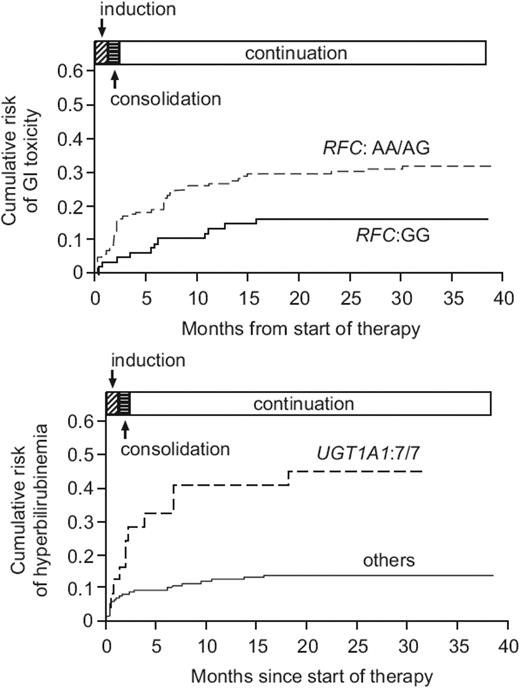
Consolidation
Only antimetabolites (methotrexate and mercaptopurine) were given, and the most common toxicities were gastrointestinal and hyperbilirubinemia (Table 1). The RFC 80A allele, a polymorphism in the methotrexate uptake transporter, was the only genotype significantly associated with gastrointestinal toxicity, and the UGT1A1 7/7 genotype was highly predictive for hyperbilirubinemia (Table 3; Figures 3–4), as in remission induction. When genotypes were combined into 3 pathway-directed functional groups (defined in Figure 1, Table S5), the antimetabolite pathway group was related to gastrointestinal toxicity (overall P = .006), whereas the phase II conjugating enzyme group was highly (overall P = .002) and the glucocorticoid group was weakly (overall P = .047) related to hyperbilirubinemia (Table S6).
Incidence of toxicity based on specific genotypes. Cumulative incidence of the first episode of grade 3 to 4 gastrointestinal (GI) toxicity differing (P = .014) by RFC genotypes during therapy (top). Cumulative incidence of the first episode of grade 3 to 4 hyperbilirubinemia differing (P < .001) by UGT1A1 genotypes, during therapy (bottom).
Incidence of toxicity based on specific genotypes. Cumulative incidence of the first episode of grade 3 to 4 gastrointestinal (GI) toxicity differing (P = .014) by RFC genotypes during therapy (top). Cumulative incidence of the first episode of grade 3 to 4 hyperbilirubinemia differing (P < .001) by UGT1A1 genotypes, during therapy (bottom).
Continuation
Multiple agents were given for more than 120 weeks, but glucocorticoid use was less intensive than during remission induction. The UGT1A1 polymorphism remained the strongest predictor (odds ratio, 17.0; P < .001) of hyperbilirubinemia (Table 3; Figure 3), as during induction and consolidation; incidence of first episode of hyperbilirubinemia was strongly related (P < .001) to UGT1A1 genotype (Figure 4). The CYP3A5 and VDR intron 8 polymorphisms were associated with peripheral neurotoxicity and the GSTP1 GG genotype, with central nervous system toxicity (Table 2). The RFC 80 A allele continued to significantly associate with gastrointestinal toxicity as during consolidation (Table 3; Figures 3–4). With genotypes combined into pathway-directed functional groups, the phase II conjugating enzyme group genotype was related to hyperbilirubinemia (overall P = .001) and to central nervous system toxicity (overall P = .027), and the glucocorticoid group genotype was associated with peripheral neurotoxicity (overall P = .024) (Table S6).
Methotrexate pharmacokinetics
The only antileukemic agent for which pharmacokinetic data were available for all patients was high-dose methotrexate, given twice during consolidation and up to 8 times during continuation. In univariate logistic regression analyses, the only toxicities significantly related to methotrexate clearance were gastrointestinal toxicity (P = .044) and hyperbilirubinemia during the continuation phase (P < .001), although only the latter was significant in a multivariate analysis (P = .026), with average methotrexate clearance lower (92.0 ± 22.2 mL/min per m2) among patients who experienced hyperbilirubinemia than among those who did not (113.4 ± 24.4 mL/min per m2) (Figure S1). Methotrexate clearance significantly predicted hyperbilirubinemia even after adjusting for UGT1A1 genotype (P = .024). Average methotrexate clearance was lower (102.5 ± 24.0 mL/min per m2) among patients with the lower-activity UGT1A1 7/7 genotype than those with other UGT1A1 genotypes (113.6 ± 24.9 mL/min per m2; P = .028) (Figure S1). The UGT1A1 7/7 genotype significantly predicted hyperbilirubinemia (P < .001) even after adjusting for methotrexate clearance. Methotrexate clearance did not differ between patients with RFC AA/AG and GG genotypes (112.7 vs 113.3 mL/min per m2; P = .93).
Genotype correlations
To test whether association of genotypes with toxicities was confounded by associations among genotypes, we assessed correlations among genotypes at the 16 loci. Other than the expected linkage disequilibrium within some loci (eg, CYP3A4 with CYP3A5; MDR1 exon 21 with MDR1 exon 26 polymorphisms), the only genotypes correlated were the MDR exon 21 and CYP3A4 polymorphisms (P < .001) (Table S7). However, these 2 loci were not associated with toxicities in this analysis, and when gene-gene interactions were assessed separately within racial groups, there was no association between the 2 polymorphic loci (P = .999 in whites).
Discussion
In this comprehensive pharmacogenetic study of patients with leukemia, several inherited polymorphisms were significantly related to toxicity of antileukemic therapy. Of particular interest are polymorphisms related to toxicity during more than one phase of therapy, those that predicted more than one type of toxicity (Figure 3), and those that could be related to pharmacokinetics of specific medications.31,32
We found that RFC genotype was associated with infection and gastrointestinal toxicity (Table 3); patients harboring the A allele exhibited a substantial increase in incidence of gastrointestinal toxicity (Figures 3–4). RFC codes for a membrane transporter responsible for cellular uptake of reduced folate and methotrexate.33 Prior experimental work has failed to yield an unequivocal functional consequence resulting from the G to A nonsynonymous substitution at position 80,34,35 although several clinical studies corroborate findings of enhanced toxicity associated with the A allele. Although it has been reported that patients with the RFC AA genotype have higher plasma methotrexate concentrations than those with the AG or GG genotype,36 our data did not corroborate that finding. While these results indicate a potential role for this RFC SNP in toxicity for patients on this protocol, we acknowledge that such genotype/phenotype associations could be complicated by other folate-related polymorphisms, the regimen of leucovorin rescue relative to the methotrexate exposure, and the indirect effects of the RFC on folate and purine/pyrimidine homeostasis.
The strongest predictor of hyperbilirubinemia was the UGT1A1 promoter-repeat polymorphism (Table 3; Figures 3–4). Bilirubin is a substrate for UGT1A1, and the promoter-repeat polymorphism predicts hyperbilirubinemia even in the absence of drug challenge.37,38 However, in the presence of drug challenge, bilirubin concentrations could conceivably be even higher, especially in patients with the low activity UGT1A1 7/7 genotype. In fact, we found that patients with low methotrexate clearance were at higher risk of hyperbilirubinemia (Figure S1), and because both methotrexate clearance and the UGT1A1 polymorphism predicted hyperbilirubinemia, it is possible that higher concentrations of both bilirubin and methotrexate could be due to lower clearance of both, by virtue of each interacting with UGT1A1. This is consistent with a report that methotrexate can inhibit glucuronidation.39 Thus, lower UGT1A1 activity could directly result in hyperbilirubinemia due to reduced bilirubin conjugation, and also indirectly by resulting in higher plasma methotrexate, which could competitively inhibit bilirubin conjugation and excretion.
The VDR intron 8 polymorphism has been associated with several clinical phenotypes,19,40–42 directly or through regulation of CYP3A43 or p-glycoprotein, but has not previously been associated with the toxicities reported here. We found that VDR intron 8 GG genotype was related to gastrointestinal toxicity and infection during induction (Table 3). In contrast, there was no association between VDR polymorphisms and toxicities during consolidation, when only antimetabolites were used. VDR effects on other “glucocorticoid” pathway genes (CYP3A, MDR1, and NR3C1) are complicated when glucocorticoids are given along with other CYP3A/MDR1 substrates during the remission induction phase, because glucocorticoids are potent enhancers of plasma clearance of antileukemic agents (Figure 1),42 which may function as both substrates and inhibitors of CYP3A. Thus, if a polymorphism causes decreased CYP3A activity, this may decrease clearance for most CYP3A substrates (eg, vincristine, etoposide, and daunorubicin) but that may be countered by greater exposure to glucocorticoid, which increases clearance of CYP3A substrates. Hence, that the VDR intron 8 GG genotype was associated with greater toxicity during remission induction but lower toxicity during the continuation phase (Table 3) could be because steroids are given continuously during remission induction but not in continuation. Similar considerations may explain why the “low activity” CYP3A5 G allele was associated with higher risk of toxicity during induction but with lower risk during continuation (Table 3).
The toxicities we analyzed were the most common we observed that included grades 3 and 4, but not all toxicities were dose limiting. For example, hyperbilirubinemia or peripheral neuropathy rarely influenced delivery of therapy, whereas severe infection or mucositis generally resulted in therapy delays. Other ALL studies that emphasize other medications are likely to result in identification of alternative predictive polymorphisms, and both alternative candidate gene and genome-wide strategies to assess germ-line genotype effects on toxicity are likely to identify additional predictive genotypes.
It has been suggested that a series of polymorphisms within pathways may be more predictive of pharmacologic phenotypes than single gene loci. To address this, we clustered polymorphisms into 3 functional groups (Figure 1; Table S5). However these multigenic “pathway” genotypes were no more informative than the strongest individual loci (compare Table S6 to Table 3). It is possible that genotypes for polymorphisms in some genes have evolved to “compensate” for dysfunction in other genes. That MDR1 and CYP3A polymorphisms are significantly associated with each other when all racial groups are combined, and that multigenic pathways are not more predictive of toxicity than single loci, support our hypothesis that human polymorphisms tend to act to “cancel each other out” rather than necessarily accentuating interindividual phenotypic differences.
Inactivating polymorphisms in TPMT12 were not associated with toxicity in this study, as they were in our prior clinical trial.44 This is because the current study included algorithms for prospectively measuring TPMT status and adjusting mercaptopurine dosages downward in all children with at least one TPMT nonfunctional allele and evidence of myelosuppression. This illustrates the potential clinical benefit of prospectively adjusting chemotherapy based on genotypes that have been definitively linked to risk of specific adverse drug effects. In this regard, new genotype/phenotype associations identified in the current study could also lead to less toxicity once translated into routine clinical use in future protocols.
It has been shown that population genetic structure may confound candidate genotype-phenotype association studies.45,46 The improvement in defining genotype versus phenotype relationships likely depends upon the mechanistic basis for confounding by race, the “accuracy” of self-reported race, as well as racial composition of the group. In this study, the more refined assessment of race made possible by genotyping at 176 markers (n = 240) did not alter our genotype versus toxicity findings compared with adjusting for self-reported race, perhaps because of high concordance (Figure 2) between genetically assessed and self-reported race in this cohort.
How should these polymorphisms that affect toxicity be interpreted in the context of their effects on relapse risk? In this protocol, the strongest predictors of hematologic relapse were the higher-activity GSTM1 nonnull and the TYMS 3/3 genotypes.22 Fortunately, we found that neither of these polymorphisms was associated with toxicity. Our results raise the possibility that one may be able to identify pharmacogenetic profiles for patients in whom increased dosages may be warranted to decrease risk of relapse, and for others in whom decreased dosages may be necessary to decrease risk of toxicity. Further studies including patients on alternative chemotherapeutic regimens would be beneficial to enhance the observations herein, as it is likely that additional predictive genotypes may be elucidated by future candidate gene or genome-wide studies.
We conclude that germ-line polymorphisms in candidate genes plausibly linked to the pharmacodynamics of antileukemic therapy influence risk of toxicity during this therapy. Eventually, individualizing dosages based partly on inherited genetic predisposition holds promise as a strategy to minimize risk of serious toxicity without compromising efficacy.
Authorship
Contribution: M.V.R. and W.E.E. conceived the project; C.-H.P. is a principal investigator of the leukemia trials and supervised clinical data collection; N.H. reviewed cases of neurotoxicity; C.C., D.P., and G.L.R. carried out and interpreted the statistical analyses; T.F. carried out the AIMs genotyping; S.D., E.H.C., and C.R. performed genotyping; S.K. and D.F. interpreted the data and were primary authors; and all the investigators contributed to the writing of the paper.
Conflict-of-interest disclosure: One of the authors (T.F.) is employed by a company (DNAPrint Genomics) whose product (AncestrybyDNA 2.5) was used in the present work for some genotyping. These genotyping results were donated by DNAPrint Genomics.
Correspondence: Department of Pharmaceutical Sciences, St Jude Children's Research Hospital, 332 N Lauderdale, Memphis, TN 38105-2794; e-mail: mary.relling@stjude.org.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
The online version of this article contains a data supplement.
This work was supported by National Cancer Institute (NCI) grants CA51001, CA78224, and CA21765; grants from the National Institutes of Health (NIH)/National Institute of General Medical Sciences (NIGMS) Pharmacogenetics Research Network and Database (U01 GM61393, U01 GM61374; http://pharmgkb.org/PS206362); a Center of Excellence grant from the State of Tennessee; and the American Lebanese Syrian Associated Charities (ALSAC). C.-H.P. is the American Cancer Society F. M. Kirby Clinical Research Professor.
We thank our protocol coinvestigators, clinical and research staff, and the patients and their families for their participation.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal