Abstract
Protein C inhibitor (PCI) is a serpin with affinity for heparin and phosphatidylethanolamine (PE). We analyzed the interaction of PCI with different phospholipids and their oxidized forms. PCI bound to oxidized PE (OxPE), and oxidized and unoxidized phosphatidylserine (PS) immobilized on microtiter plates and in aqueous suspension. Binding to OxPE and PS was competed by heparin, but not by the aminophospholipid-binding protein annexin V or the PCI-binding lipid retinoic acid. PS and OxPE stimulated the inhibition of activated protein C (aPC) by PCI in a Ca++-dependent manner, indicating that binding of both, aPC (Ca++ dependent) and PCI (Ca++ independent), to phospholipids is necessary. A peptide corresponding to the heparin-binding site of PCI abolished the stimulatory effect of PS on aPC inhibition. No stimulatory effect of phospholipids on aPC inhibition was seen with a PCI mutant lacking the heparin-binding site. A heparin-like effect of phospholipids (OxPE) was not seen with antithrombin III, another heparin-binding serpin, suggesting that it is specific for PCI. PCI and annexin V were found to be endogenously colocalized in atherosclerotic plaques, supporting the hypothesis that exposure of oxidized PE and/or PS may be important for the local regulation of PCI activity in vivo.
Introduction
Protein C inhibitor (PCI) is a member of the serpin (serine protease inhibitor) family of protease inhibitors. It belongs to the subgroup of alpha-1-antitrypsin–like serpins (clade A) and its gene symbol is SERPINA5.1 PCI, originally described in plasma as an inhibitor of the anticoagulant serine protease activated protein C (aPC),2,3 inactivates many other serine proteases including blood coagulation factors,4,5 fibrinolytic enzymes,4,6 tissue kallikrein,7 and the sperm protease acrosin.8,9 Human PCI is expressed in many organs and tissues10–13 and is present in many body fluids and secretions.11 Complexes of PCI with proteases are present in body fluids,6,14 indicating that PCI interacts with the respective proteases not only in vitro but also in vivo
Human PCI demonstrates modest efficiency as a protease inhibitor, and for some of its target proteases more efficient inhibitors have been described.15,16 However, its specific environment may change the activity and target enzyme specificity of PCI in vivo. PCI is a heparin-binding serpin,17–21 and heparin can stimulate the interactions of PCI with many of its target proteases. In vivo heparin is present mainly intracellularly,22 while on the cell surface membrane-associated heparin sulfate–containing proteoglycans can substitute for heparin.18 In contrast to their activating action on aPC inhibition by PCI, glycosaminoglycans interfere with the inhibition of tissue kallikrein by PCI.7,23 Thus, local factors such as glycosaminoglycans and proteoglycans could play an important role in regulating both the activity of PCI and its selectivity with respect to different target proteases.23
It has been shown by Nishioka et al24 that the phospholipid phosphatidylethanolamine (PE) can bind to PCI and stimulate its inhibitory activity toward aPC, suggesting that phospholipids are important endogenous cofactors of PCI. The protein C system represents a major anticoagulant pathway, and genetic defects affecting the protein C system are the most common risk factors for thrombotic diseases.25–27 Besides its role in coagulation, aPC decreases inflammatory responses, partially by inhibition of nuclear translocation of nuclear factor-kappa B,26–28 and blocks vascular and neuronal toxicities of tissue plasminogen activator.29 Stimulation of PCI activity in vivo could therefore not only increase the risk for thrombotic events, but also result in the suppression of anti-inflammatory and antiapoptotic activities. Different types of cellular stress, tissue injury, and inflammation are accompanied by changes in phospholipid levels, intracellular distribution, and oxidation. We therefore asked the question whether these changes could influence the binding of PCI and the process of aPC inactivation.
Here we show that oxidized PE, unoxidized PS, and oxidized PS directly bind PCI and stimulate its inhibitory activity toward aPC in a heparin-like manner, suggesting that at sites of apoptosis and/or lipid oxidation (eg, in atherosclerotic plaques)30 PCI could efficiently reduce anticoagulant and anti-inflammatory activities of aPC.
Materials and methods
Proteins and reagents
Recombinant PCI31 and urinary PCI7,18 were prepared as described. Plasma PCI was purified according to the protocol for the purification of urinary PCI using anti–PCI (4PCI)–IgG-Sepharose7 and heparin-Sepharose (HiTrap-Heparin HP; Amersham Bioscience, Björkgaten, Sweden). A peptide corresponding to the heparin-binding site of PCI (AA264-283; SEKTLRKWLKMFKKRQLELY) was obtained from piChem (Graz, Austria). The purity of this peptide was more than 95% as judged from high-performance liquid chromatography (HPLC) analysis and mass spectrometry. Human antithrombin III (ATIII) and low-molecular-weight heparin from porcine intestinal mucosa (MW, 4000-6000; Sigma, Vienna, Austria), thrombin (Technoclone, Vienna, Austria), tissue kallikrein from human urine (Calbiochem, Darmstadt, Germany), and aPC (Baxter, Vienna, Austria) were obtained as indicated. The synthetic substrates pyroGlu-Pro-Arg-pNA · HCl (S-2366), H-D-Val-Leu-Arg-pNA · 2HCl (S-2266), and H-D-Phe-Pip-Arg-pNA · 2HCl (S-2238) were from Chromogenix (Milano, Italy). Rabbit anti–PCI-IgG and monoclonal mouse anti–PCI-IgG (4PCI)7 were prepared as described. Mouse anti–Penta-His-IgG was from Qiagen (Qiagen-Vertriebs, Vienna, Austria). Secondary antibodies Alexa Fluor 488 goat anti–rabbit IgG (H+L) and Alexa Fluor 568 goat anti–mouse IgG (H+L) were from Molecular Probes (Eugene, OR). Rabbit polyclonal anti–annexin V IgG was from Abcam (Cambridge, United Kingdom). Enhanced chemiluminescence (ECL) anti–rabbit IgG, horseradish peroxidase–linked whole antibody from donkey, and ECL anti–mouse IgG, horseradish peroxidase–linked whole antibody from sheep, were obtained from Amersham Bioscience (Björkgarten, Sweden). Synthetic phospholipids were from Avanti Polar Lipids (Alabaster, AL). Bovine serum albumin (BSA; Fraction V) was from AppliChem (Darmstadt, Germany). Whenever BSA was used, it was assured that eventually present lipids did not influence the results of the assay. All other reagents and solvents were of analytical grade.
Mutagenesis of PCI
The cDNA for human PCI was cloned between the NdeI and BamHI restriction sites in the pET-15b plasmid (Novagen, Darmstadt, Germany) as described.31 Deletion of bases 962 to 1004 32 of the cDNA of human PCI coding for amino acids 264-277 (H-helix) was done according to the QuickChange Site-directed Mutagenesis Kit procedure (Stratagene, Amsterdam, the Netherlands), using the following primers respectively: 5′-GTG GAG AAT GGA CTG AGG CAG CTC GAG CTT-3′ (forward) and 5′-AAG CTC GAG CTG CCT CAG TCC ATT CTC CAC-3′ (reverse). The plasmids were purified and sequenced using ABI PRISM Big Dye Terminator Cycle Sequencing Ready Reaction Kit (Applied Biosystems, Foster City, CA) on a 310 Genetic Analyzer from Perkin Elmer (Wellesley, MA) to verify the deletion in the mutant construct. The expression and purification of the mutated protein (ΔH-PCI) was done according to the protocol described31 except that the heparin-Sepharose step was omitted.
Lipid oxidation
1-Palmitoyl-2-arachidonoyl-sn-glycero-3-phosphoethanolamine (PAPE), 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphocholine (PAPC), and 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphoserine (PAPS) were oxidized by exposure of the dried lipids to air for 24 to 72 hours. The extent of oxidation was monitored by thin-layer chromatography, and the analysis of the oxidation end products was performed by positive (for OxPAPC, OxPAPE) or negative (for OxPAPS) ion electrospray mass spectrometry as described previously.30
Preparation of phospholipid vesicles
Phospholipids were dissolved in chloroform (10 mg/mL) and stored at −80°C. For each experiment, phospholipid vesicles were prepared freshly. Different amounts of phospholipids were pipetted into Eppendorf tubes. The antioxidant butylated hydroxytoluene (20 μM; Sigma) was added to unoxidized as well as to oxidized phospholipids. Chloroform was evaporated under argon. Dried phospholipids were resuspended in buffer by vortexing at maximal speed for 30 seconds and than shaking (1100 rpm) for 5 minutes at 37°C.
Binding of PCI to immobilized phospholipids
Wells of microtiter plates (Nunc maxisorp; Nunc, Roskilde, Denmark) were coated with phospholipids (PAPE, OxPAPE, PAPC, OxPAPC, PAPS, or OxPAPS; 100 μg/mL each) resuspended in 100 μL of 100 mM NaHCO3 buffer, pH 9.3.24 After 2-hour incubation at 37°C, remaining binding sites were blocked for 2 hours with 5% BSA in 250 μL phosphate-buffered saline (PBS: 140 mM NaCl, 2.7 mM KCl, 1.5 mM KH2PO4, 8 mM Na2HPO4, pH 7.4). After washing the wells with PBS containing 0.1% BSA, 100 μL PCI (4-40 nM) or ΔH-PCI (4 nM) in PBS containing 1% BSA was added to the wells and incubated for 1 hour at 37°C. Binding of PCI to immobilized phospholipids was studied in the absence and presence of heparin (2.5 or 50 μg/mL), retinoic acid (50 nM to 5 μM), PAPE, OxPAPE, PAPS, OxPAPS, PAPC, or OxPAPC (100 μg/mL each). Binding of PCI to phospholipids was also studied in the absence and presence of a 10-fold molar excess of annexin V in PBS containing 2.5 mM CaCl2. Thereafter, the wells were washed and incubated with 100 μL rabbit anti–PCI IgG (14 μg/mL) in PBS containing 0.5% BSA for 1 hour at 37°C. After washing with PBS, 100 μL peroxidase-coupled donkey anti–rabbit IgG (1:1000) in PBS containing 0.5% BSA was added to the wells. After 1 hour of incubation at 37°C, the wells were washed and 100 μL ABTS solution containing 1 g/L diammonium 2,2′-aazino-di-(3-ethylbenzothiazoline-6-sulfonate; Roche Diagnostics, Vienna, Austria), 77 mM Na2HPO4, 60 mM C6H8O7, and 1 mL/L H2O2 was added to the wells. The reaction was stopped with 100 μL 0.32% NaF and the absorbance at 405 nm was determined using an enzyme-linked immunosorbent assay (ELISA) reader (EL 808 Ultra Microplate Reader; Bio-TEK Instruments, Winooski, VT). To account for nonspecific binding, binding of PCI to uncoated wells was determined in each experiment and subtracted from the binding to immobilized phospholipids. PCI concentrations at which half maximal binding occurred were calculated using GraphPad Prism (GraphPad Software, San Diego, CA).
Inhibition of aPC by PCI
Inhibition of the amidolytic activity of aPC by PCI or ΔH-PCI was tested on 96-well microtiter plates. aPC (0.5 or 5 nM) was incubated with PCI (10-90 nM) or ΔH-PCI (10 or 20 nM) in the absence or presence of heparin (0.5 or 2.5 μg/mL) or phospholipids (PAPE, OxPAPE, PAPS, OxPAPS, PAPC, or OxPAPC, 0.5-50 μg/mL) at 37°C in 100 μL Tris-buffered saline (TBS: 10 mM Tris, 100 mM NaCl, pH 7.4), containing 1% BSA and either 2.5 mM CaCl2 or 5 mM EDTA. In some experiments, the peptide corresponding to the H-helix of PCI (peptide AA264-283) was included at final concentrations between 0.1 and 190 μM. After 0.5 to 20 minutes, 100 μL S-2366 (0.4 mM) dissolved in 50 mM Tris-HCl, 100 mM NaCl, pH 8.0, was added to each well. After 20 minutes, the A405 was determined in an ELISA reader. The relative activity of 1 was assigned to the amidolytic activity of incubation mixtures without PCI, and for each reaction remaining aPC activity was calculated. Second-order rate constants were calculated from 3 independent experiments performed in duplicates.7,18,31
Control experiments verified that peptide AA264-283 influenced neither the amidolytic activity of aPC nor the inhibitory activity of PCI in the absence of heparin and phospholipids. Also, phospholipids did not significantly affect the amidolytic activity of aPC.
Inhibition of tissue kallikrein by PCI
Inhibition of the amidolytic activity of purified tissue kallikrein by recombinant PCI was tested on 96-well microtiter plates. Tissue kallikrein (2 nM) was incubated with PCI (45 nM final) in the absence or presence of heparin (0.25-5 μg/mL), PAPS (2.5-75 μg/mL), OxPAPS (2.5-75 μg/mL), PAPE (2.5-50 μg/mL), OxPAPE (2.5-50 μg/mL), PAPC (2.5-75 μg/mL), or OxPAPC (2.5-75 μg/mL) at 37°C in 100 μL TBS buffer containing 1% BSA. After 60 minutes, 100 μL S-2266 (0.4 mM) dissolved in 50 mM Tris-HCl, pH 8.3, was added to each well, and after additional incubation for 3 hours at 37°C, the A405 was determined in an ELISA reader. Remaining kallikrein activity was calculated for each reaction mixture using the relative activity of one for the amidolytic activities of incubation mixtures containing no PCI.
Inhibition of thrombin by antithrombin III (ATIII) or PCI
Inhibition of the amidolytic activity of thrombin by ATIII or PCI was tested on 96-well microtiter plates. Thrombin (1 nM) was incubated with ATIII (20-80 nM) or PCI (7.5-30 nM) in the absence or presence of heparin (2.5 μg/mL), PAPE (50 μg/mL), or OxPAPE (50 μg/mL) at 37°C in 100 μL TBS containing 1% BSA. After 20 minutes, 100 μL S-2238 (0.4 mM) dissolved in 50 mM Tris-HCl, 38 mM NaCl, pH 8.3, was added to each well. After 15 minutes, the A405 was determined in an ELISA reader. Remaining thrombin activity was calculated for each reaction mixture using the relative activity of 1 for the amidolytic activities of incubation mixtures containing no inhibitor.
Native PAGE, SDS-PAGE, and Western blotting
The interaction of PCI with phospholipids was also analyzed by native polyacrylamide gel electrophoresis (PAGE) followed by Western blotting. PCI (350 nM) was incubated without or with PAPE, OxPAPE, or OxPAPS (100 μg/mL each) in PBS containing 1 mM EDTA (pH 8.0) for 30 minutes at 37°C with constant vortexing. Thereafter, an equal volume of sample buffer (20% glycerol, 0.0025% bromphenol blue in PBS containing 1 mM EDTA) was added, and the samples were subjected to native PAGE (8% acrylamide; Tris-HCl based) and analyzed by Western blotting. Proteins were transferred onto PVDF membranes (Millipore, Bedford, MA). Blocking was done with 5% BSA in PBS containing 0.1% Tween 20 at 4°C overnight. Thereafter, the membranes were incubated with the primary antibody (mouse anti–Penta-His IgG, 0.2 μg/mL) for 1 hour at 37°C, and washed with PBS containing 0.1% Tween 20 prior to the addition of the secondary antibody (sheep anti–mouse IgG peroxidase conjugate, 1:1000). The signal was detected with ECL plus Western blotting detection System reagents (Amersham Bioscience, Buckinghamshire, United Kingdom).
Complex formation of aPC and PCI in the presence of PAPE and OxPAPE was analyzed by SDS-PAGE and Western blotting. aPC (200 nM) was incubated with PCI (400 nM) in the absence or presence of 1 μg/μL heparin, 50 μg/mL PAPE, or 50 μg/mL OxPAPE, respectively, in TBS for 30 minutes at 37°C. The reactions were stopped by adding an equal volume of Laemmli buffer (125 mM Tris-HCl [pH 6.8], 20% glycerol, 2.5% SDS, 0.0025% bromphenol blue)33 and heating of the samples at 95°C for 5 minutes. Thereafter, the samples were subjected to SDS-PAGE (10% acrylamide). Protein bands were visualized by silver staining.34 The same samples were also analyzed by Western blotting performed as described above using rabbit anti–PCI IgG (14 μg/mL) and donkey anti–rabbit IgG peroxidase conjugate (1:1000).
The mutated protein ΔH-PCI (44 kDa) was also analyzed by SDS-PAGE and Western blotting performed as described above with mouse anti–Penta-His IgG (0.2 μg/mL) and sheep anti–mouse IgG peroxidase conjugate (1:1000).
Immunohistochemistry
Tissues were snap frozen and embedded in Tissue-Tek OCT Compound (Miles, Elkhart, IN). Cryosections were fixed in acetone at minus 20°C and used for standard immunodetection immediately. Blocking was done with 5% normal goat serum (DAKO, Vienna, Austria) in PBS for 1 hour at room temperature.
For detection of PCI, mouse monoclonal anti–PCI IgG (4PCI; 10 μg/mL) and Alexa Fluor 568 goat anti–mouse IgG (4 μg/mL) were used. Annexin V was detected with rabbit polyclonal anti–annexin V IgG (16 μg/mL) and Alexa Fluor 488 goat anti–rabbit IgG (6.6 μg/mL). All antibodies were diluted in Dako Cytomation Antibody Diluent (DAKO). Confocal images were taken by a Zeiss LSM-Meta microscope system with a 40×/1.3 NA oil immersion objective in multitrack mode with pinholes of 72 μm and were handled with the Zeiss AIM-software package (Zeiss, Jena, Germany).
Analytical methods
The concentrations of plasma PCI, urinary PCI, recombinant PCI, and ΔH-PCI were determined by ELISA as described previously.35 The concentrations of active enzymes were determined from the cleavage of the chromogenic substrates S-2366 (aPC), S-2266 (tissue kallikrein), and S-2238 (thrombin), respectively, as indicated by the manufacturer (Chromogenix).
Concentrations of phospholipids were determined by lipid phosphorus assay.36 Aqueous phospholipid suspensions were prepared from dried lipid films in 1.5-mL tubes before usage. Percentages of phospholipid solubilization (above 94% for PAPC, OxPAPC, and OxPAPS) were calculated after comparison of phospholipid amounts found in aqueous suspensions and chloroform stock solutions.
All concentrations of proteins, phospholipids, heparin, and chromogenic substrates shown indicate final concentrations.
Statistical analyses
Data shown in the figures are means ± SEM. Statistical significance of differences was calculated using unpaired Student t test.
Results
Binding of PCI to phospholipids
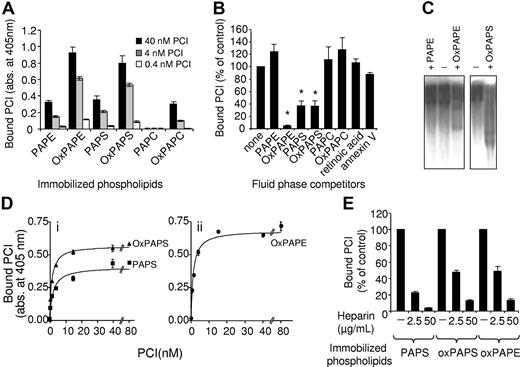
Binding of recombinant PCI to different immobilized phospholipids was studied. PCI bound to immobilized phospholipids (Figure 1A); the highest binding was observed with coated OxPAPE and OxPAPS. Much less binding was seen with immobilized PAPE, PAPS, and OxPAPC. No binding was observed with immobilized PAPC. Similar results were obtained with PCI purified from human plasma (not shown). In order to ensure that PCI binding is not an artifact of lipid immobilization, we studied competition of PCI binding to immobilized OxPAPE by phospholipids in suspension. PAPS, OxPAPS, and OxPAPE added as aqueous lipid suspensions inhibited the binding of PCI to immobilized OxPAPE, whereas unoxidized PAPE and PAPC (oxidized or unoxidized) did not influence binding of PCI to immobilized phospholipids (Figure 1B). When PCI was incubated with OxPAPE or OxPAPS and afterward analyzed by native PAGE followed by Western blotting, a mobility shift of PCI antigen was seen (Figure 1C), confirming binding of PCI to OxPAPE and OxPAPS in lipid suspension. No mobility shift was observed when PCI was incubated with PAPE.
Binding of PCI to immobilized and soluble phospholipids. (A) Phospholipids (100 μg/mL) were immobilized on microtiter plates (Nunc maxisorp; Nunc) and incubated with different concentrations of recombinant PCI (as indicated). Bound PCI was detected as described in “Materials and methods.” Absorbance values shown are corrected for nonspecific binding to uncoated plates and represent means ± SEM of triplicates. The absorbance values at 405 nm for nonspecific binding were between 0.130 and 0.215. Similar results were obtained in at least 3 independent experiments. (B) Microtiter plates were coated with OxPAPE (100 μg/mL) and incubated with 4 nM recombinant PCI in the absence or presence of phospholipids (as indicated, 100 μg/mL each), retinoic acid (5 μM), or annexin V (40 nM in a buffer containing 2.5 mM Ca++). Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown, *P ≤ .001. (C) PCI (350 nM) was incubated with PAPE, OxPAPE, or OxPAPS (100 μg/mL each) as described in “Materials and methods” and loaded on a native 8% PAGE gel. Western blotting was done as described in “Materials and methods.” (D) PAPS, OxPAPS (i), or OxPAPE (ii) (100 μg/mL each) was immobilized on microtiter plates and incubated with different concentrations of recombinant PCI. Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown. (E) Phospholipids were immobilized on microtiter plates (as indicated, 100 μg/mL each) and incubated with PCI (4 nM) in the absence and presence of heparin (concentrations as indicated). Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown.
Binding of PCI to immobilized and soluble phospholipids. (A) Phospholipids (100 μg/mL) were immobilized on microtiter plates (Nunc maxisorp; Nunc) and incubated with different concentrations of recombinant PCI (as indicated). Bound PCI was detected as described in “Materials and methods.” Absorbance values shown are corrected for nonspecific binding to uncoated plates and represent means ± SEM of triplicates. The absorbance values at 405 nm for nonspecific binding were between 0.130 and 0.215. Similar results were obtained in at least 3 independent experiments. (B) Microtiter plates were coated with OxPAPE (100 μg/mL) and incubated with 4 nM recombinant PCI in the absence or presence of phospholipids (as indicated, 100 μg/mL each), retinoic acid (5 μM), or annexin V (40 nM in a buffer containing 2.5 mM Ca++). Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown, *P ≤ .001. (C) PCI (350 nM) was incubated with PAPE, OxPAPE, or OxPAPS (100 μg/mL each) as described in “Materials and methods” and loaded on a native 8% PAGE gel. Western blotting was done as described in “Materials and methods.” (D) PAPS, OxPAPS (i), or OxPAPE (ii) (100 μg/mL each) was immobilized on microtiter plates and incubated with different concentrations of recombinant PCI. Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown. (E) Phospholipids were immobilized on microtiter plates (as indicated, 100 μg/mL each) and incubated with PCI (4 nM) in the absence and presence of heparin (concentrations as indicated). Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown.
Binding of PCI to immobilized PAPS, OxPAPS, and OxPAPE was dose dependent and saturable (Figure 1D). Half maximal binding was observed at 1.4, 1.5, and 2.8 nM PCI for OxPAPS, OxPAPE, and PAPS, respectively.
Binding of PCI to immobilized phospholipids was not dependent on Ca++, since it was similar in the presence of 2.5 mM Ca++ and in the absence of Ca++ in a buffer containing 5 mM EDTA (not shown). Heparin interfered dose dependently with the binding of PCI to immobilized PAPS, OxPAPS, and OxPAPE (Figure 1E), while retinoic acid, which has been previously shown to bind PCI,37 had no effect up to a concentration of 5 μM (shown for OxPAPE in Figure 1B). These data suggest that binding of PCI to phospholipids involves the heparin-binding site of PCI, which is located in the H-helix,20 but not the retinoic acid–binding site.38 Binding of PCI to OxPAPE, PAPS, and OxPAPS was similar in the absence and presence of annexin V (10-fold molar excess over PCI in a buffer containing 2.5 mM Ca++), a protein binding to the head group of PS39 and aldehyde-modified PE40 (shown for OxPAPE in Figure 1B).
Effect of phospholipids on the interaction of PCI with target proteases
Inhibition of aPC.
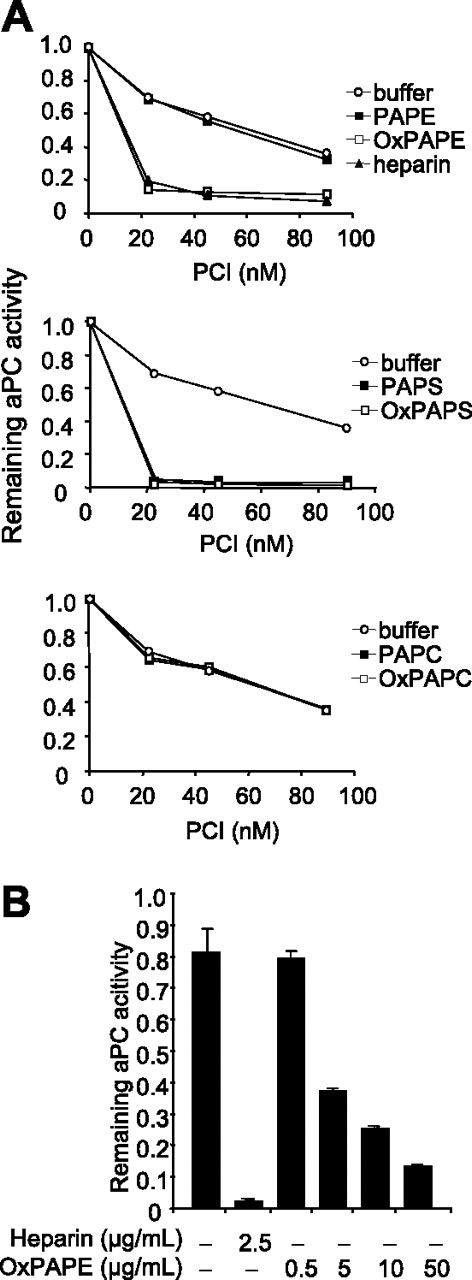
PAPS, OxPAPS, and OxPAPE stimulated the inhibition of aPC by recombinant PCI in systems containing 2.5 mM Ca++, while PAPE, PAPC, and OxPAPC had no effect (Figure 2A; Table 1). Similar results were obtained with PCI purified from plasma or urine (not shown). The stimulatory effect of phospholipids was dose dependent as shown for OxPAPE in Figure 2B. Second-order rate constants (k2) calculated for the inhibition of aPC in the absence and presence of PAPS, OxPAPS, or OxPAPE (50 μg/mL) indicate a 133- to 194-fold stimulation of the reaction by these phospholipids, which is very similar to the stimulatory effect of 2.5 μg/mL heparin (Table 1). k2 calculated in the presence of PAPC, OxPAPC, and PAPE confirmed that these phospholipids have no stimulatory effect. In the absence of Ca++, PAPS, OxPAPS, and OxPAPE interfered with the inhibition of aPC by PCI (Figure S1, available on the Blood website; see the Supplemental Figures link at the top of the online article), while PAPE, PAPC, and OxPAPC had no effect. The interfering effect of phospholipids was dose dependent (Figure S2A) and could be reversed in a dose-dependent manner by heparin (Figure S2B). To confirm the inhibitory effect of OxPAPE on the interaction of PCI with aPC in the absence of Ca++, complex formation of aPC with PCI was analyzed by SDS-PAGE and Western blotting. In the absence of Ca++, neither aPC-PCI complex formation nor cleavage of PCI by aPC occurred in the presence of OxPAPE as judged from silver-stained gels and Western blots, respectively (Figure S3). Unoxidized PAPE effected neither complex formation (Figure S3 upper panel) nor cleavage of PCI (Figure S3 lower panel). The requirement of Ca++ for the stimulatory effect of phospholipids on aPC inhibition by PCI together with the fact that protein C/aPC binding to phospholipids is Ca++ dependent support the assumption that these phospholipids, similarly to heparin, serve as a template for aPC and PCI binding, thereby facilitating their interaction.
Effect of phospholipids on the inhibition of aPC by PCI. (A) aPC (5 nM) was incubated for 20 minutes with different concentration (as indicated) of recombinant PCI in the absence and presence of heparin (2.5 μg/mL) or phospholipids (as shown, 50 μg/mL each) in the presence of 2.5 mM CaCl2. Remaining aPC activity was determined as described in “Materials and methods.” Data shown represent the means of duplicates. Similar results were obtained in at least 3 independent experiments performed with different preparations of recombinant PCI. (B) aPC (5nM) was incubated for 20 minutes with PCI (35 nM) and with different concentrations of OxPAPE or heparin (as shown) in the presence of 2.5 mM CaCl2. Remaining aPC activity was determined as described in “Materials and methods.” Data shown are means of triplicates ± SEM. Similar results were obtained in at least 3 independent experiments.
Effect of phospholipids on the inhibition of aPC by PCI. (A) aPC (5 nM) was incubated for 20 minutes with different concentration (as indicated) of recombinant PCI in the absence and presence of heparin (2.5 μg/mL) or phospholipids (as shown, 50 μg/mL each) in the presence of 2.5 mM CaCl2. Remaining aPC activity was determined as described in “Materials and methods.” Data shown represent the means of duplicates. Similar results were obtained in at least 3 independent experiments performed with different preparations of recombinant PCI. (B) aPC (5nM) was incubated for 20 minutes with PCI (35 nM) and with different concentrations of OxPAPE or heparin (as shown) in the presence of 2.5 mM CaCl2. Remaining aPC activity was determined as described in “Materials and methods.” Data shown are means of triplicates ± SEM. Similar results were obtained in at least 3 independent experiments.
Second-order rate constants (k2) for the inhibition of aPC by PCI and ΔH-PCI in the presence of heparin (2.5 μg/mL) or phospholipids (50 μg/mL each)
| . | k2, M−1min−1, mean ± SEM . | Fold stimulation . |
|---|---|---|
| rPCI-wt | ||
| Buffer | 9.58 ± 0.90 × 104 | — |
| Heparin | 2.58 ± 0.05 × 107 | 269 |
| OxPAPE | 1.47 ± 0.31 × 107 | 153 |
| PAPE | 1.79 ± 0.63 × 105 | 1.9 |
| OxPAPS | 1.27 ± 0.11 × 107 | 133 |
| PAPS | 1.86 ± 0.06 × 107 | 194 |
| OxPAPC | 4.06 ± 1.13 × 104 | 0.4 |
| PAPC | 5.75 ± 1.35 × 104 | 0.6 |
| ΔH-PCI | ||
| Buffer | 1.27 ± 0.18 × 105 | — |
| Heparin | 1.31 ± 0.35 × 105 | 1.03 |
| PAPS | 1.32 ± 0.37 × 105 | 1.04 |
| . | k2, M−1min−1, mean ± SEM . | Fold stimulation . |
|---|---|---|
| rPCI-wt | ||
| Buffer | 9.58 ± 0.90 × 104 | — |
| Heparin | 2.58 ± 0.05 × 107 | 269 |
| OxPAPE | 1.47 ± 0.31 × 107 | 153 |
| PAPE | 1.79 ± 0.63 × 105 | 1.9 |
| OxPAPS | 1.27 ± 0.11 × 107 | 133 |
| PAPS | 1.86 ± 0.06 × 107 | 194 |
| OxPAPC | 4.06 ± 1.13 × 104 | 0.4 |
| PAPC | 5.75 ± 1.35 × 104 | 0.6 |
| ΔH-PCI | ||
| Buffer | 1.27 ± 0.18 × 105 | — |
| Heparin | 1.31 ± 0.35 × 105 | 1.03 |
| PAPS | 1.32 ± 0.37 × 105 | 1.04 |
— indicates not applicable.
Inhibition of tissue kallikrein.
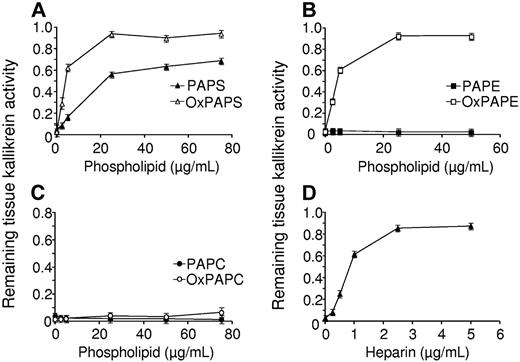
We have shown previously that heparin interfered with the interaction of PCI with tissue kallikrein.7,23 As can be seen from Figure 3, also OxPAPE, PAPS, and OxPAPS, but not PAPE, PAPC, or OxPAPC interfered in a dose-dependent way with the inhibition of tissue kallikrein by PCI. This effect was the same in the absence and presence of Ca++. These data suggest that phospholipids exert opposite effects with respect to PCI and tissue kallikrein compared to PCI and aPC.
Effect of phospholipids on the inhibition of tissue kallikrein by PCI. Tissue kallikrein (2 nM) was incubated for 60 minutes with PCI (45 nM) in the absence or presence of different concentrations of OxPAPS, PAPS (A), OxPAPE, PAPE (B), OxPAPC, PAPC (C), or heparin (D). Remaining tissue kallikrein activity was determined as described in “Materials and methods.” Each value represents the mean ± SEM of triplicate determinations.
Effect of phospholipids on the inhibition of tissue kallikrein by PCI. Tissue kallikrein (2 nM) was incubated for 60 minutes with PCI (45 nM) in the absence or presence of different concentrations of OxPAPS, PAPS (A), OxPAPE, PAPE (B), OxPAPC, PAPC (C), or heparin (D). Remaining tissue kallikrein activity was determined as described in “Materials and methods.” Each value represents the mean ± SEM of triplicate determinations.
Involvement of the heparin-binding site in the interaction of PCI with phospholipids
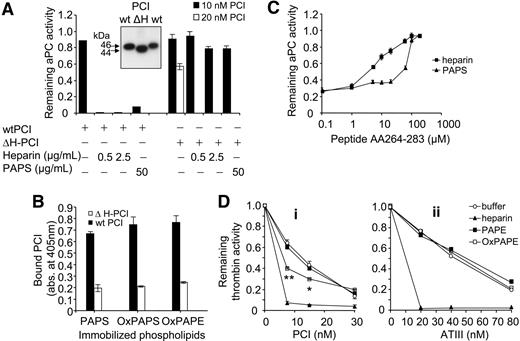
The fact that heparin interfered with the binding of PCI to immobilized phospholipids as well the observations that heparin reversed the inhibitory effect of phospholipids on the aPC inhibition by PCI in the absence of Ca++ suggest that phospholipid binding could involve the heparin-binding site of PCI, which is located in the H-helix.20 We therefore studied inhibition of aPC by mutated PCI, in which the H-helix was deleted. This mutant still inhibited aPC (Figure 4A; Table 1); however, it did not bind to immobilized PAPS, OxPAPS, or OxPAPE to an appreciable extent (Figure 4B), and neither heparin nor PAPS stimulated its inhibitory activity (Figure 4A; Table 1). Furthermore, a peptide corresponding to the H-helix of PCI (AA264-283) interfered in a dose-dependent manner not only with the stimulatory effect of heparin, but also with the stimulatory effect of PAPS on aPC inhibition by wild-type PCI (Figure 4C). Taken together, these data strongly support the hypothesis that the heparin-binding site of PCI is also required for phospholipid binding.
The stimulatory effect of phospholipids requires the heparin-binding site of PCI. (A) aPC was incubated with recombinant wild-type PCI (wtPCI) or mutated PCI, in which the H-helix was deleted (ΔH-PCI) in the absence and presence of heparin or PAPS for 20 minutes as indicated. Remaining aPC activity was determined using S-2366 as described in “Materials and methods.” (Inset) Western blots performed after SDS-PAGE of wtPCI and ΔH-PCI. (B) PAPS, OxPAPS, and OxPAPE (100 μg/mL each) were immobilized on microtiter plates and incubated with wild-type PCI or ΔH-PCI (4 nM each). Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown. (C) aPC was incubated with PCI (10 nM) in the presence of heparin (0.5 μg/mL) or PAPS (50 μg/mL) and in the presence of different concentrations of peptide AA264-283 for 20 minutes at 37°C. Remaining enzymatic activity was determined as described in “Materials and methods.” (D) Thrombin (1 nM) was incubated for 20 minutes with different concentrations of PCI (i) or ATIII (ii) in the absence or presence of heparin (2.5 μg/mL), PAPE (50 μg/mL), or OxPAPE (50 μg/mL). Remaining thrombin activity was determined as described in “Materials and methods.” Data shown represent means of quadruplicates (i) or duplicates (ii). *P ≤ .02; **P ≤ .004. Similar results were obtained in 3 independent experiments.
The stimulatory effect of phospholipids requires the heparin-binding site of PCI. (A) aPC was incubated with recombinant wild-type PCI (wtPCI) or mutated PCI, in which the H-helix was deleted (ΔH-PCI) in the absence and presence of heparin or PAPS for 20 minutes as indicated. Remaining aPC activity was determined using S-2366 as described in “Materials and methods.” (Inset) Western blots performed after SDS-PAGE of wtPCI and ΔH-PCI. (B) PAPS, OxPAPS, and OxPAPE (100 μg/mL each) were immobilized on microtiter plates and incubated with wild-type PCI or ΔH-PCI (4 nM each). Bound PCI was detected as described in “Materials and methods.” Means of triplicates ± SEM are shown. (C) aPC was incubated with PCI (10 nM) in the presence of heparin (0.5 μg/mL) or PAPS (50 μg/mL) and in the presence of different concentrations of peptide AA264-283 for 20 minutes at 37°C. Remaining enzymatic activity was determined as described in “Materials and methods.” (D) Thrombin (1 nM) was incubated for 20 minutes with different concentrations of PCI (i) or ATIII (ii) in the absence or presence of heparin (2.5 μg/mL), PAPE (50 μg/mL), or OxPAPE (50 μg/mL). Remaining thrombin activity was determined as described in “Materials and methods.” Data shown represent means of quadruplicates (i) or duplicates (ii). *P ≤ .02; **P ≤ .004. Similar results were obtained in 3 independent experiments.
To analyze whether certain (oxidized) phospholipids could substitute for heparin/glycosaminoglycans not only in the interaction of PCI with proteases but also in other heparin-dependent reactions, we studied the effect of phospholipids on the inhibition of thrombin by ATIII, another heparin-binding serpin. For comparison, we studied the effect of phospholipids on the inhibition of thrombin by PCI. However, while OxPAPE stimulated the inhibition of thrombin by PCI (Figure 4Di), it had neither a stimulatory nor an inhibitory effect on the inhibition of thrombin by ATIII (Figure 4Dii). These data suggest that the modification of inhibitory activity by phospholipids is not a common property of heparin-binding serpins.
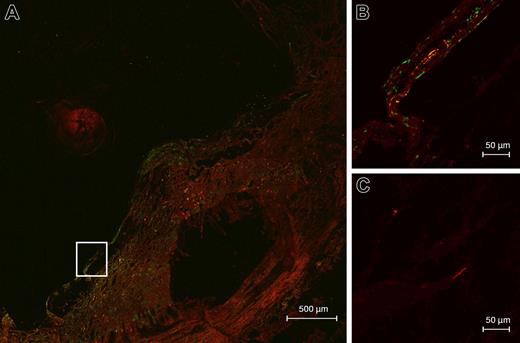
Colocalization of PCI and annexin V in atherosclerotic plaques
To determine whether binding of PCI to phospholipids may also occur in vivo, we stained cryosections of atherosclerotic plaques, known to be enriched in apoptotic cells and phospholipid oxidation products,30 for the presence of PCI and annexin V, a protein generally used to detect surface-exposed phosphatidylserine. In atherosclerotic plaques annexin V is endogenously present,41 presumably associated with phosphatidylserine. In 6 independent atheromas (type II-Va according to the AHA classification42 ) studied so far, PCI antigen was present as judged from confocal laser scanning microscopy. Colocalization of PCI and annexin V was studied in a type IV-Va plaque (Figure 5), and is shown in a region of the fibrous cap, indicating a close proximity of annexin V and PCI.
PCI and annexin V are colocalized in atherosclerotic plaques. Cryosections of atherosclerotic plaques were prepared and stained for PCI (monoclonal anti–PCI IgG and Alexa Fluor 568 goat anti–mouse IgG, red) and annexin V (rabbit anti–annexin V IgG and Alexa Fluor 488 goat anti–rabbit IgG, green) as described in “Materials and methods.” Sections were analyzed by confocal laser scanning microscopy. Yellow color indicates colocalization of PCI (red) and annexin V (green). (A) Atherosclerotic plaque type IV-Va, overview; (B) detail corresponding to the framed area in panel A; (C) control without first antibody, same detail as in panel B.
PCI and annexin V are colocalized in atherosclerotic plaques. Cryosections of atherosclerotic plaques were prepared and stained for PCI (monoclonal anti–PCI IgG and Alexa Fluor 568 goat anti–mouse IgG, red) and annexin V (rabbit anti–annexin V IgG and Alexa Fluor 488 goat anti–rabbit IgG, green) as described in “Materials and methods.” Sections were analyzed by confocal laser scanning microscopy. Yellow color indicates colocalization of PCI (red) and annexin V (green). (A) Atherosclerotic plaque type IV-Va, overview; (B) detail corresponding to the framed area in panel A; (C) control without first antibody, same detail as in panel B.
Discussion
PCI can associate with platelet phospholipids, which can stimulate its inhibitory activity toward aPC.24 In this study, we analyzed the interaction of PCI with individual phospholipid classes. To avoid a bias introduced by the variations in fatty acid contents, we studied effects of synthetic phospholipids, all being composed of the same fatty acids (ie, palmitic acid at position sn-1 and arachidonic acid at position sn-2) as well as the oxidized forms of these phospholipids. We show here that PCI binds to PAPS, both to the unoxidized and the oxidized forms, and to oxidized PAPE. Half-maximal binding to these phospholipids was observed at PCI concentrations between 1.4 and 2.8 nM, indicating high affinity of PCI for these phospholipids and suggesting optimal binding at normal plasma concentrations of PCI (∼ 90 nM).11 Comparable binding was seen with PCI purified from human urine or plasma and recombinant human PCI, indicating that glycosylation of PCI is not important for phospholipid binding.
We furthermore show that those phospholipids that bind PCI (ie, PAPS, OxPAPS, and OxPAPE) also stimulate its inhibitory activity toward aPC and thrombin (shown for OxPAPE). In case of aPC, this stimulatory effect is comparable to the stimulatory effect of heparin and is strongly dependent on the presence of Ca++. These findings are consistent with data demonstrating that the stimulation of aPC inhibition by PE is dependent on the Gla domain of aPC,24 which is the major Ca++-binding site.43 The discrepancy between the data of Nishioka et al,24 who described binding of PCI to PE, and our data (binding of PCI only to oxidized PE) may be explained by possible differences in the fatty acid composition between their and our PE preparation or by the fact that phospholipids used in that study might have been partially oxidized.
We propose that binding of PCI to phospholipids involves the heparin-binding site, which is located in the H-helix: Binding of PCI to immobilized phospholipids can be competed by heparin, whereas retinoic acid, which binds PCI without affecting its inhibitory function,37 did not compete with the binding of PCI to phospholipids. The retinoic acid–binding site has been postulated to be located in a hydrophobic pocket created by the N-terminal shortening of helix A of PCI relative to helix A of other serpins.38 Furthermore, heparin abolished the interfering effect of phospholipids on the aPC-PCI interaction in Ca++-free systems, again suggesting competition for the same binding site. We therefore studied inhibition of aPC by a PCI mutant, in which the H-helix was deleted (ΔH-PCI). The activity of ΔH-PCI, which in the absence of heparin demonstrated inhibitory activity comparable to that of wild-type PCI, could be stimulated neither by heparin nor by PAPS. We also studied inhibition of aPC by PCI in the presence of PAPS and increasing concentrations of a peptide corresponding to the H-helix of PCI. We can show that this peptide, known to quench the stimulatory effect of heparin,20 abolished not only the effect of heparin but also the effect of PAPS. Taken together, our data support the hypothesis that positively charged amino acids in the H-helix of PCI are involved not only in heparin binding, but also in the binding of PAPS, OxPAPS, and OxPAPE.
The results of our studies suggest that PAPS and OxPAPE could in general act as hitherto unrecognized functional analogs for heparin and influence other heparin-dependent reactions as well. We therefore studied inhibition of thrombin by ATIII, another heparin-binding serpin, in the presence of these phospholipids. However, we observed neither a stimulatory nor an interfering effect of phospholipids on the inhibition of thrombin by ATIII, although in control experiments these phospholipids also stimulated the inhibition of thrombin by PCI. Therefore, PAPS, OxPAPS, and OxPAPE seem to specifically interact with the heparin-binding site of PCI.
In living cells, PE and PS are localized mainly to the inner leaflet of the plasma membrane, whereas PC, which does not interact with PCI, is the main phospholipid of the outer leaflet.44 A classical condition under which PS, and also PE, become exposed to the outer leaflet of the plasma membrane is apoptosis.44–46 In addition, PE and PS become surface exposed upon platelet activation47 and during a sperm maturation process called capacitation.48,49 Also cells of the trophoblast have PS on the outer leaflet of the cell membrane.50 Transient exposure of PS is furthermore observed in cell fusion, such as in myotube formation during skeletal muscle development.51 Oxidation of phospholipids occurs under different conditions, and the presence of phospholipid oxidation products in atherosclerotic vessels is well documented.52 These data raise the intriguing possibility that PAPS, OxPAPS, and OxPAPE may act as inducible “heparin analogs,” adding an additional level of regulation of proteolysis at sites of injury and inflammation.
To determine whether binding of PCI to negatively charged/oxidized phospholipids also occurs in vivo, we used the atherosclerotic plaque as a model for a tissue rich in apoptotic cells and oxidized phospholipids. By double-immunostaining for PCI and the phosphatidylserine-binding protein annexin V, which is endogenously present in atherosclerotic plaques,41 we can show colocalization of PCI and annexin V. Based on these data, we suggest that binding of PCI to negatively charged/oxidized phospholipids also occurs in vivo, and that phospholipids may promote local accumulation of PCI. Additionally, phospholipids can stimulate PCI activity by more than 100-fold (Table 1). Therefore PCI might be locally a much more efficient inhibitor of aPC than expected from its plasma concentration. Despite the fact that oxidized phospholipids have been shown to enhance the anticoagulant function of aPC,53 lipid oxidation could therefore promote blood coagulation and thrombus formation at sites of tissue injury by stimulating the inhibition of aPC by PCI. PCI has been shown previously to be a mild risk factor for venous thrombosis54 and a risk marker for acute coronary events.55 Our present data on the stimulation of PCI activity by phospholipids together with these previous observations suggest consideration of a possible role of PCI in arterial thrombosis.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by grants P16093-B04, P17337-B09 (M.G.), and S9407-B11 (V.B.) from the Austrian Science Foundation, by the EU Molstroke project LSHM-CT-2004-005206 (V.B.), and by the Wiener Wissenschafts-, Forschungs- und Technologiefonds, project LSC200 (V.B.).
We thank Thomas Nardelli for his help with the artwork.
Authorship
Contribution: J.M.M., O.O., V.B., B.S., T.P., J.B., B.R.B., and M.G. participated in designing the research; J.M.M., O.O., I.J., B.S., and T.P. performed research; J.M.M., O.O., V.B., J.B., and M.G. controlled and analyzed data; J.M.M., V.B., and M.G. wrote the paper; all authors checked the final version of the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Margarethe Geiger, Department of Vascular Biology and Thrombosis Research, Center for Biomolecular Medicine and Pharmacology, Medical University of Vienna, Schwarzspanierstraße 17, A-1090 Vienna, Austria; e-mail: margarethe.geiger@meduniwien.ac.at.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal