Abstract
Background: High-dose chemotherapy and hematopoietic stem cell (HSC) transplantation is curative in about 40% of patients with relapsed chemosensitive diffuse large B cell lymphoma (DLBCL). The international prognostic index obtained at the time of relapse (IPI-R) and the time from initial treatment to relapse (TTR) have been suggested in different series to be predictors of outcome after HSC transplantation. We explored the concomitant effect of IPI-R and TTR on therapeutic outcome in a modern and uniform cohort of patients with relapsed chemosensitive DLBC undergoing high-dose chemotherapy and peripheral HSC transplantation.
Methods: Retrospective analysis of 80 consecutive patients treated at Mayo Clinic, Rochester, MN between 2001 and 2006 who received a peripheral HSC transplant (except for 3 patients who receive bone marrow) after being conditioned with BCNU, etoposide, cytarabine and melphalan (BEAM) for relapsed chemosensitive DLBCL.
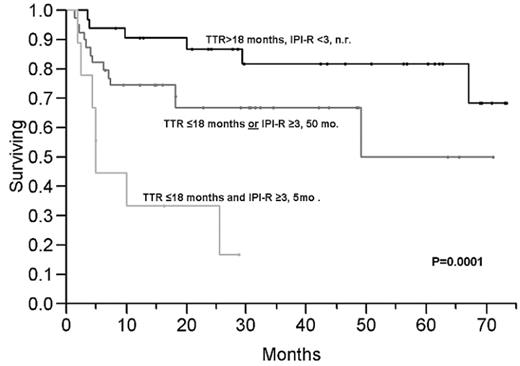
Results: Median follow-up of survivors was 31.4 months, Median age at the time of transplant was 62 (interquartile range 53–65; range 26–77), 65% were males; median number of prior chemotherapy regimens was 2. All patients had received at least one previous anthracycline-based regimen, 78% had been previously exposed to rituximab and all achieved at least CRu after the initial treatment. The median time from diagnosis to relapse was 19 months (interquartile range 10–43), 25% of patients had a high or high-intermediate IPI-R. The median survival from the time of transplant for patients with TTR>18 months v. ≤ 18 months was not reached and 50 months respectively (P=0.005). Median survival for patients with high or high-intermediate IPI-R at the time of relapse (IPI score ≥3) was 23.3 months and not reached for patients with low or low-intermediate IPI (P=0.01). These two factors were independent in multivariate analysis with RR for death of 1.8 (1.2–2.9; P=0.004) for TTR ≤ 18 months and 1.7 (1.1–2.5; P=0.017) for high or high-intermediate IPI and therefore combined in a prognostic system were patients with none (n=32), one (n=39) or two (n=9) of these prognostic factors had median disease free survival not reached v. 50 months v. 3.3 months (P=0.001) and overall survival not reached v. 50 months v. 5 months (P=0.0001) (Figure).
Conclusion: TTR and IPI-R provide an easy and powerful prognostic system in patients with DLBCL undergoing modern high-dose chemotherapy with HSC support.
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal