Abstract
Impact of complete response on outcome is a subject of ongoing debate.
Aim: In this retrospective analysis of all myeloma-ASCT patients transplanted between 1999– 2007 (n: 116) in our center with a minimum 3 mo followup (n: 91) and a disease status available at the time of M (n:66) were analyzed for evaluation of the impact of response at M, preASCT, postASCT; the preASCT use of novel agents ; timing of M (>,< 6 mo) and ASCT (>,< 12 mo) on response and survival. 91 patients aged 33–66(med: 52) were included. Induction (VAD/T D/MP: 72/8/10) was given for a median of 8.3 mo pre M. 45 patients received additional chemo (n:3), (V :1, T :17, both:10) or none(n:41) untill ASCT with Melphalan (200 mg/sq.m) within 12 months (54%). For < 90% response, V/T alone or in combination was given during the postASCT period and/or received a second ASCT/NMA. SPSS version 11.0 was used for Kaplan Meier survival and Chi Square analysis.
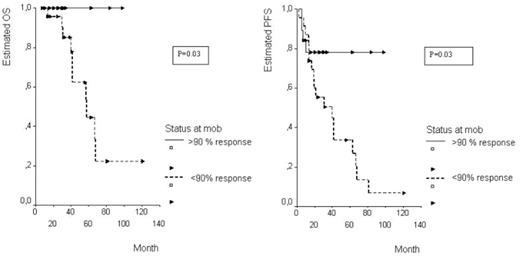
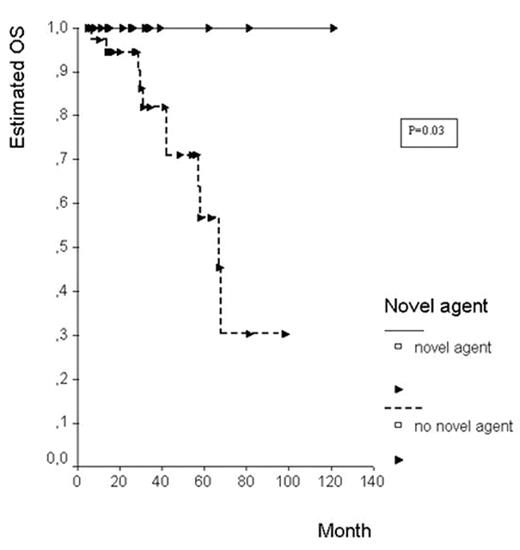
Results: Patient characteristics between early vs late M or ASCT, novel agent (+) vs (−) were similar .>90% response rates at different time points (M/preASCT/postASCT) were: 54.5%, 59.7% and 61.3%. One third of patients could be mobilized early. Response rates of early and late M were: 73.6% vs 46.6% (p=0.04). Novel agents were used less frequently in early M patients (22% vs 40%). Among all analyzed, only response during M, timing of M and use of V/T were found to be influential on PFS and/or OS. Evaluation of factors (b2mg,ISS,age,chemo line)on response during M revealed only late M to be associated with less response (p=0.05). Among early M patients, amplitude of response (>90% vs others) did not prolong PFS or OS. However, among patients who were mobilized later, achievement of >90% response prolonged PFS at 3 yr (100% vs 85%,p=0.03) at 5 yr (100% vs 44%,p=0.03) (Fig.1). The impact of response to induction, on OS was also observed in all patients irrespective of M time (3 yr: 93% vs 83%, 5 yr: 80% vs 55%, p=0.02). Comparison of patients who had received at least one novel agent during the preASCT, compared to those not, revealed an OS prolongation (3yr:100% vs 81%; 5yr: 81% vs 56%, p=0.03). (Fig. 2). Patients who had received a novel agent were mobilized at similar times but were transplanted later (9/27 vs 28/42, p= 0.01). Although there was a trend, novel agents did not influence PFS or response rate significantly at any time point.
Conclusions: In this retrospective analysis, we were able to demonstrate a benefical effect of response amplitude, earlier (<6 months) mobilization,and pre ASCT use of novel agents. Early M but not late M masks any influence of chemosensitivity to induction. Late M which is associated with less response contributes to the impact of response on survival.
Author notes
Disclosure:Research Funding: Janssen Cilag. Membership Information: Janssen Cilag and Pharmion.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal