Abstract
Oncogenic activation loop KIT mutations are observed in acute myeloid leukemia (AML) and systemic mastocytosis (SM); however, unlike the KIT juxtamembrane mutants, the activation loop mutants are insensitive to imatinib mesylate. Furthermore, as prior studies primarily used heterologous cell lines, the molecular mechanism(s) underlying oncogenic KIT-induced transformation in primary cells is poorly understood. We demonstrate that expression of KITD814V in primary hematopoietic stem/progenitor cells (HSC/Ps) and mast cell progenitors (MCps) induces constitutive KIT autophosphorylation, supports ligand-independent hyperproliferation, and promotes promiscuous cooperation with multiple cytokines. Genetic disruption of p85α, the regulatory subunit of class IA lipid kinase phosphoinositol-3-kinase (PI3K), but not of p85β, or genetic disruption of the hematopoietic cell-specific Rho GTPase, Rac2, normalizes KITD814V-induced ligand-independent hyperproliferation. Additionally, deficiency of p85α or Rac2 corrects the promiscuous hyperproliferation observed in response to multiple cytokines in both KITD814V-expressing HSC/Ps and MCps. Treatment of KITD814V-expressing HSC/Ps with a Rac inhibitor (NC23766) or with rapamycin showed a dose-dependent suppression in ligand-independent growth. Taken together, our results identify p85α and Rac2 as potential novel therapeutic targets for the treatment of KITD814V-bearing AML and SM.
Introduction
Stem cell factor (SCF) is a unique cytokine with important functional roles in melanocytes, germ cells, interstitial cells of Cajal, mast cells, and hematopoietic stem cells.1 Consistent with the importance of SCF signaling within these defined tissues, activating mutations of KIT, which encodes the receptor for SCF, have been described in germ cell tumors, gastrointestinal stromal tumors (GISTs), sinonasal lymphomas, acute myeloid leukemia (AML), and systemic mastocytosis (SM).2-6 SM is characterized by clonal expansion of myelomastocytic progenitors with tissue accumulation of malignant mast cells and commonly bears the KIT activation loop mutant KITD816V.7 Although this disease may assume an indolent course, it can also take an aggressive direction (aggressive systemic mastocytosis or mast cell leukemia) or can be associated with a non–mast-cell hematologic malignancy (associated clonal hematologic non–mast-cell lineage disease). Oncogenic KIT mutations are also observed in core binding factor-acute myeloid leukemia (CBF-AML), leukemias that bear either the t(8;21) or inv(16) cytogenetic abnormality, generating the fusion genes AML1-ETO or CBFβ-MYH11 and disrupting CBFα (AML1) or CBFβ, respectively.8 Studies examining both adult and pediatric AML have indicated that the presence of the KITD816V mutant in CBF-AML carrying t(8;21) worsens the prognosis based on several clinical indices.9-12
Oncogenic KIT is constitutively phosphorylated, suggesting that signals emanating from this receptor are not regulated by ligand stimulation,13,14 and, consistently, cell lines expressing oncogenic KIT demonstrate ligand-independent proliferation.13,15,16 KIT contains an extracellular portion containing 5 immunoglobulin-like repeats, a transmembrane domain, a juxtamembrane domain, and a cytoplasmic tyrosine kinase domain that is split by an insert sequence. Activating KIT mutations within the juxtamembrane region are commonly found in GISTs and are sensitive to inhibition by the tyrosine kinase inhibitor, imatinib mesylate (Gleevec); however, KIT mutations within the carboxy-terminal lobe of the cytoplasmic tyrosine kinase domain (TK2), such as KITD816V, stabilize the KIT activation loop conformation in its active form, which precludes sufficient imatinib binding for tyrosine kinase inhibition. Therefore, in contrast to successful use of imatinib mesylate to treat GISTs, imatinib mesylate is ineffective for the treatment of the hematologic diseases commonly harboring the KIT activation loop mutants, including SM and CBF-AML.17-19 Accordingly, experimental tyrosine kinase inhibitors have been examined for efficacy in inhibiting the proliferation or promoting the apoptosis of KITD816V-bearing cells. Tyrosine kinase inhibitors PKC412 and BMS-354825 (dasatinib), and to a lesser extent AMN107, are able to inhibit the growth of the human mast cell line HMC-1, which harbors both the KITV560G and the KITD816V mutations, and Ba/F3 cells bearing KITD814V.20-22 Additionally, PKC412 demonstrated some efficacy in a patient with mast cell leukemia, although the patient eventually succumbed to the disease.23 Although results from these studies are promising, interpretation of these data is limited due to the use of heterologous and transformed cell lines, which may not accurately reflect the aberrant molecular mechanisms and abnormal substrate utilization induced by oncogenic KIT mutants. Thus, additional studies are warranted to better define the molecular mechanisms of transformation induced by oncogenic KIT activation loop mutants in relevant primary cells.
It has been hypothesized that KIT activation loop mutants, including KITD816V (human) and KITD814V or KITD814Y (murine), alter the specificity of KIT substrate recognition and utilization.14 As a result, the nonspecific signals emanating from oncogenic KIT are promiscuous in nature and induce aberrant signals not normally regulated by wild-type KIT, including the activation of signal transducer and activator of transcription 3 (STAT3)24,25 and the degradation of KIT-signaling inhibitory molecules, such as Shp-1.14 Therefore, an alternative therapeutic approach to directly targeting KIT is to target KIT effector molecules that contribute to the transformation of oncogenic KIT-bearing cells. Previous functional and pharmacologic studies using cell line models and wortmannin, respectively, have demonstrated that the lipid kinase phosphoinositol-3-kinase (PI3K) may contribute to the transforming ability of D816V (murine D814V).15,26-28
Although informative, these studies do not provide information regarding the extent to which PI3K contributes to the transforming ability of D816V. In addition, conclusions drawn from these studies are limited as in some cases the cell types used normally do not express KIT, and, thus, it is likely that the substrate availability within these cells differs from that of primary KIT-expressing hematopoietic progenitor/stem cells (HSC/Ps) and mast cell progenitors (MCps). Additionally, the class IA PI3Ks are a group of heterodimeric lipid kinases composed of a p85 regulatory subunit (p85α, p55α, p50α, p85β, or p85γ) and a p110 catalytic subunit (p110α, p110β, or p110δ)29,30 and are all nonspecifically inhibited by wortmannin.31-33 Thus, although the use of wortmannin as a PI3K inhibitor is useful in experimental in vitro systems, this inhibitor is broad spectrum, nonspecific, and associated with extreme toxicity in vivo.33 Therefore, to better understand and to intelligently manipulate the PI3K signaling cascade for therapeutic purposes, qualitative as well as quantitative studies evaluating the contribution of the PI3K regulatory subunits to the transforming capacity of oncogenic KIT are essential. In addition to PI3K itself, downstream effectors of PI3K may also play a role in and serve as therapeutic targets in oncogenic KIT-bearing diseases. Multiple lines of evidence demonstrate that several Rac-regulated cellular functions depend on PI3K activity34 and that products of PI3K activate Vav, a guanine-nucleotide exchange factor, which promotes the conversion of inactive Rac-GDP to active Rac-GTP.35 We chose to focus specifically on Rac2, which is hematopoietic specific, in contrast to Rac1, which is ubiquitously expressed. Furthermore, Rac2−/− mice are viable and relatively normal, while the Rac1−/− mice are lethal in utero, suggesting that Rac2 inhibition should be well tolerated over prolonged periods and, therefore, may provide a relatively specific and less toxic therapeutic target.
Although cell lines expressing KITD814V clearly demonstrate ligand-independent proliferation,13,36 these studies may not portray the true abnormalities induced by oncogenic KIT in relevant primary myeloid or mast cells. This is particularly important as the expression and activation of kinases and their downstream transcription factors in primary HSC/Ps or MCps are likely to differ significantly from those seen in heterologous cell lines. Adding to the complexity is the well-documented role of KIT in cooperating with a significant number of lineage-specific cytokines in the expansion of the bone marrow progenitor cell pool, which, unfortunately cannot be appreciated in factor-dependent cell lines.1 Therefore, we have used genetic and pharmacologic approaches to examine the effect of inhibition of p85α or p85β, regulatory subunits of class IA PI3K, and of Rac2, to define the molecular mechanisms underlying the transforming capacity of KITD814V in HSC/Ps and MCps, with the long-term goal of defining novel therapeutic targets in CBF-AML and SM.
Materials and methods
Mice, cytokines, and antibodies
C57BL/6 mice were purchased from Jackson Laboratory (Bar Harbor, ME). p85α+/− and Rac2−/− mice have been previously described.29,37 Mice deficient in the expression of both Rac2 and p85α were obtained by crossing Rac2−/− mice with p85α+/− mice. Progeny from these crosses were genotyped by polymerase chain reaction (PCR) as previously described.29,37 All mice used in this study were between 6 and 8 weeks of age. These mice were maintained under specific pathogen-free conditions at the Indiana University Laboratory Animal Research Center (Indianapolis, IN), and this study was approved by the Institutional Animal Care and Use Committee of the Indiana University School of Medicine. Murine interleukin-3 (IL-3), IL-4, IL-10, stem cell factor (SCF), granulocyte colony-stimulating factor (G-CSF), macrophage colony-stimulating factor (M-CSF), and thrombopoietin (Tpo) were purchased from Peprotech (Rocky Hill, NJ). Methylcellulose-based media were obtained from StemCell Technologies (Vancouver, BC). Rapamycin was purchased from Cell Signaling (Beverly, MA) and NSC23766 was purchased from Calbiochem (San Diego, CA). Anti-p85α antibody and antiphosphotyrosine (4G10) antibodies were purchased from Upstate Biotechnology (Lake Placid, NY).
Construction of wild-type (WT) and mutant KIT receptors
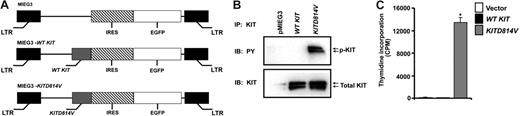
cDNA encoding wild-type murine KIT was cloned into a bicistronic retroviral vector MIEG3 as previously described.38 The Quick Change site-directed mutagenesis kit (Stratagene, La Jolla, CA) and primers (forward: 5′-GGG CTA GCC AGA GTC ATC AGG AAT GAT TCG-3′; reverse: 5′-CGA ATC ATT CCT GAT GAC TCT GGC TAG CCC-3′) were used to mutate aspartic acid at residue 814 to valine in the wild-type murine KIT gene to generate KITD814V. EcoRI-NotI fragment containing the KITD814V mutation was verified by sequencing and ligated into the EcoRI-NotI sites of the MIEG3 retroviral vector. The KITD814V cDNA was inserted upstream of the internal ribosome entry site (IRES) and the enhanced green fluorescent protein (EGFP) gene (Figure 1).
Expression of KITD814V results in constitutive phosphorylation of KIT and ligand-independent growth. (A) Schematic diagram of retroviral vectors expressing WT KIT and KITD814V. (B) KITD814V is constitutively autophosphorylated in the absence of growth factor stimulation. 32D cells expressing vector alone, WT KIT, or KITD814V were lysed and equal amounts of protein were subjected to immunoprecipitation using an anti-KIT antibody followed by Western blot analysis using an antiphosphotyrosine antibody. Shown is the level of phosphorylation and total KIT protein in each lane. (C) Expression of KITD814V in 32D cells induces ligand-independent growth. 32D cells expressing empty vector, WT KIT, or KITD814V were subjected to a thymidine incorporation assay in the absence of growth factor stimulation. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector or WT KIT.
Expression of KITD814V results in constitutive phosphorylation of KIT and ligand-independent growth. (A) Schematic diagram of retroviral vectors expressing WT KIT and KITD814V. (B) KITD814V is constitutively autophosphorylated in the absence of growth factor stimulation. 32D cells expressing vector alone, WT KIT, or KITD814V were lysed and equal amounts of protein were subjected to immunoprecipitation using an anti-KIT antibody followed by Western blot analysis using an antiphosphotyrosine antibody. Shown is the level of phosphorylation and total KIT protein in each lane. (C) Expression of KITD814V in 32D cells induces ligand-independent growth. 32D cells expressing empty vector, WT KIT, or KITD814V were subjected to a thymidine incorporation assay in the absence of growth factor stimulation. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector or WT KIT.
Generation of lineage-negative (Lin−) bone marrow cells
Lineage-negative (Lin−) cells were obtained by harvesting bones from 5 to 10 mice. Red blood cells were lysed using the red cell lysis solution and cells were resuspended in IMDM containing 10% fetal bovine serum (FBS). These cells were subsequently subjected to ficoll for 30 minutes at room temperature to isolate the mononuclear low-density mononuclear cells (LDMNCs), and cells were counted using a hemocytometer. Lineage depletion was performed using the EasySep kit (StemCell Technologies).
Expression of wild-type and mutant KIT receptors in 32D cells, primary HSC/Ps, and Lin− HSC/Ps
Retroviral supernatants for transduction of 32D cells and primary bone marrow LDMNCs were generated using the Phoenix ecotropic packaging cell line transfected with retroviral vector plasmids using a calcium phosphate transfection kit (Invitrogen, Carlsbad, CA). Supernatants were collected 48 hours after transfection and filtered through 0.45-μM membranes. 32D cells were infected with 2 mL high-titer virus supernatant in the presence of 8 μg/mL polybrene. EGFP-positive cells containing the wild-type or mutant KIT were sorted to homogeneity and used in experiments. Bone marrow LDMNCs were suspended in IMDM containing 20% FBS and 1% penicillin/streptomycin and prestimulated in non-tissue culture plates supplemented with 100 ng/mL SCF, 100 ng/mL G-CSF, and 100 ng/mL Tpo for 2 days prior to retroviral infection on fibronectin fragments (Retronectin; Takara, Madison, WI). Forty-eight hours after infection, bone marrow cells expressing the vector alone, WT KIT, or KITD814V were sorted to homogeneity based on EGFP expression. Bone marrow cells expressing similar levels of vector, WT KIT, or KITD814V were used to perform all experiments.
Progenitor assay and generation of bone marrow–derived MCps
EGFP-sorted vector-, WT KIT-, or KITD814V-expressing primary bone marrow cells (1.5 × 104) were plated in methylcellulose in the presence or absence of SCF 100 ng/mL and colonies were counted on day 10. MCps were generated using EGFP-sorted cells expressing either WT KIT or KITD814V as previously described.39
Proliferation assay
Proliferation was assessed by conducting a thymidine incorporation assay on EGFP-sorted vector-, WT KIT-, or mutant KITD814V-expressing HSC/Ps or on in vitro–generated MCps. Briefly, cells were washed and starved in 0.2% BSA with or without any growth factors for 6 to 7 hours. Cells (5 × 104) were plated in a 96-well plate in 200 μL complete medium either in the absence or in presence of indicated growth factors. Cells were cultured for 48 hours and subsequently pulsed with 1.0 μCi (0.037 MBq) [3H] thymidine for 6 to 8 hours. Cells were harvested using an automated 96-well cell harvester (Brandel, Gaithersburg, MD) and thymidine incorporation was determined as counts per minute (CPM).
Immunoprecipitation, PI3K, and Rac activity assay
Western blot analysis and immunoprecipitation experiments were performed as previously described.40 32D cells expressing either the vector, WT KIT, or KITD814V were starved for 8 hours, harvested, and lysed and an equal amount of protein was subjected to immunoprecipitation. To examine levels of phosphorylated KIT, proteins were subjected to immunoprecipitation using an anti-KIT antibody, followed by Western blot analysis using an antiphosphotyrosine antibody. To examine PI3K activity, proteins were immunoprecipitated with anti-p85α antibody followed by a PI3K lipid assay, as previously described.39,41,42 Rac activity was determined by immunoprecipitation with PAK-1 p21 activated kinase binding domain-agarose (binds activated Rac) and analyzing by Western blot using an anti-Rac antibody as described.41
Results
Expression of KITD814V in 32D cells and HSC/Ps results in constitutively phosphorylated KIT and ligand-independent proliferation
To examine the biochemical and functional effect of KITD814V when expressed in myeloid cells, 32D cells were transduced with the murine stem cell virus-based retroviral vectors pMIEG3, pMIEG3-WT KIT, or pMIEG3-KITD814V (Figure 1A) and sorted to homogeneity based on EGFP expression. Cells transduced with WT KIT or KITD814V demonstrated similar levels of total KIT expression (Figure 1B); however, following 8 hours of serum and growth factor deprivation, cells bearing KITD814V demonstrated persistent KIT phosphorylation as well as ligand-independent proliferation (Figure 1B,C). Murine bone marrow LDMNCs were transduced with pMIEG3, pMIEG3-WT KIT, and pMIEG3-KITD814V and sorted to homogeneity based on EGFP expression (Figure 2A top panel). Similar to that observed in the 32D cells, primary HSC/Ps bearing KITD814V, but not WT KIT, demonstrated ligand-independent proliferation (Figure 2A). HSC/Ps depleted of lineage-committed cells (Lin− population, a homogeneous population of immature hematopoietic progenitors) expressing KITD814V also displayed ligand-independent proliferation (Figure 2B). Together, these findings demonstrate that the oncogenic KITD814V mutant functions in a constitutively active fashion and confers hyperproliferation in the absence of ligand stimulation in primary HSC/Ps.
Expression of KITD814V in HSC/Ps results in ligand-independent growth and promiscuous proliferation in response to multiple cytokines. (A) Bone marrow LDMNCs were transduced with empty vector, WT KIT, or KITD814V. Top panel demonstrates the relative transduction efficiency from one of several experiments as determined by EGFP expression (x-axis). After 48 hours of culture, cells were pulsed with [3H] thymidine in the absence of growth factors for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector or WT KIT. (B) Lin− LDMNCs were transduced with empty vector or KITD814V (top panel). EGFP-positive cells were subjected to thymidine incorporation in the absence of growth factors as described in panel A. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector. Bone marrow LDMNCs were transduced with empty vector or KITD814V (C) or with WT KIT or KITD814V (D). EGFP-positive cells were subjected to thymidine incorporation in the presence of indicated cytokines: no growth factor (NO GF), SCF 50 ng/mL, M-CSF 50 ng/mL, G-CSF 20 ng/mL, or IL-3 5 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from one of several experiments performed in quadruplicate. *P < .05, KITD814V versus vector (C) or KITD814V versus WT KIT (D).
Expression of KITD814V in HSC/Ps results in ligand-independent growth and promiscuous proliferation in response to multiple cytokines. (A) Bone marrow LDMNCs were transduced with empty vector, WT KIT, or KITD814V. Top panel demonstrates the relative transduction efficiency from one of several experiments as determined by EGFP expression (x-axis). After 48 hours of culture, cells were pulsed with [3H] thymidine in the absence of growth factors for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector or WT KIT. (B) Lin− LDMNCs were transduced with empty vector or KITD814V (top panel). EGFP-positive cells were subjected to thymidine incorporation in the absence of growth factors as described in panel A. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector. Bone marrow LDMNCs were transduced with empty vector or KITD814V (C) or with WT KIT or KITD814V (D). EGFP-positive cells were subjected to thymidine incorporation in the presence of indicated cytokines: no growth factor (NO GF), SCF 50 ng/mL, M-CSF 50 ng/mL, G-CSF 20 ng/mL, or IL-3 5 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from one of several experiments performed in quadruplicate. *P < .05, KITD814V versus vector (C) or KITD814V versus WT KIT (D).
Exogenous cytokines augment proliferation of HSC/Ps bearing KITD814V
We next examined the effect of exogenous cytokines on KITD814V-bearing HSC/P proliferation. In addition to ligand-independent growth, the proliferation of KITD814V-expressing HSC/Ps was augmented by SCF, the ligand for KIT, IL-3, or M-CSF compared with cells transduced with empty vector or WT KIT (Figure 2C,D). These findings demonstrate that KITD814V-expressing HSC/Ps hyperproliferate in response to multiple cytokines, not merely in a ligand-independent fashion or in response to the appropriate KIT ligand, SCF, suggesting promiscuous cooperation between KITD814V and multiple hematopoietic cytokine receptors. Based on these initial observations, we next probed the molecular mechanisms fundamental to the observed KITD814V-induced transformation in order to define novel therapeutic targets in CBF-AML and SM.
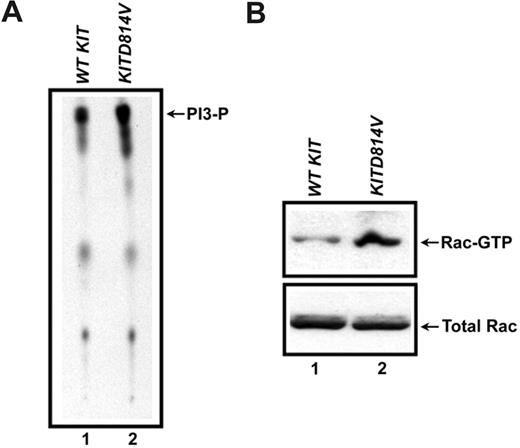
KITD814V induces increased basal activation of PI3K and Rac-GTPase
Two effector molecules within the KIT signaling pathway of potential therapeutic relevance in SM or CBF-AML are PI3K and Rac. To examine the hypothesis that KITD814V induces elevated activation of PI3K and Rac, we used 32D cells transduced with pMIEG3-WT KIT or pMIEG3-KITD814V. Cells were transduced and sorted to homogeneity, serum and growth factor deprived for 8 hours, and assayed for PI3K and Rac activity levels. Activation of Rac GTPase was measured by evaluating the ability of Rac to bind to its downstream substrate p21 activated kinase (PAK). At baseline, both PI3K and Rac were hyperactivated in cells expressing KITD814V compared with cells expressing WT KIT (Figure 3), providing evidence that pharmacologic inhibition or genetic disruption of these molecules may provide a rational approach for therapies of KITD814V-bearing diseases.
Increased basal activation of PI3K and Rac-GTPase in KITD814V-expressing hematopoietic progenitors. (A) 32D cells expressing either WT KIT or KITD814V were starved for 8 hours, harvested, and lysed. Equal amount of lysates were subjected to immunoprecipitation using an anti-p85α antibody followed by a PI3K lipid assay. The position of p85α-associated PI3-phosphate (PI3-P) activity is indicated to the right of the blot. (B) Cell lysates derived from the treatment described in panel A were analyzed for Rac-GTPase activation by incubating the lysates with PAK-1 p21 activated kinase binding domain-agarose and analyzing by Western blot using an anti-Rac antibody. The position of Rac-GTP (active Rac) is indicated to the right of the blot. The bottom panel shows total Rac protein in each lane.
Increased basal activation of PI3K and Rac-GTPase in KITD814V-expressing hematopoietic progenitors. (A) 32D cells expressing either WT KIT or KITD814V were starved for 8 hours, harvested, and lysed. Equal amount of lysates were subjected to immunoprecipitation using an anti-p85α antibody followed by a PI3K lipid assay. The position of p85α-associated PI3-phosphate (PI3-P) activity is indicated to the right of the blot. (B) Cell lysates derived from the treatment described in panel A were analyzed for Rac-GTPase activation by incubating the lysates with PAK-1 p21 activated kinase binding domain-agarose and analyzing by Western blot using an anti-Rac antibody. The position of Rac-GTP (active Rac) is indicated to the right of the blot. The bottom panel shows total Rac protein in each lane.
Genetic disruption of p85α, but not p85β, abrogates ligand-independent proliferation and colony formation of KITD814V-bearing HSC/Ps
The multiple regulatory and catalytic subunits of PI3K complicate the interpretation of PI3K hyperactivation in KITD814V-bearing cells. The PI3K regulatory subunits p85α and p85β share significant homology at the amino acid level43 ; however, based on murine genetic studies, disruption of these genes produces distinct hematopoietic phenotypes, including a selective loss of mast cells in the gut but not other tissues.30,44,45 These mice are otherwise normal, suggesting that inhibiting aspects of p85α function should be well tolerated over time. To examine the relevance of PI3K isoforms in mediating oncogenic KIT-induced ligand-independent growth and cooperation with other cytokines, we examined the effect of genetic disruption of p85α or p85β on the proliferative capacity of HSC/Ps expressing KITD814V. Upon genetic disruption of p85α, KITD814V-induced ligand-independent proliferation was reduced approximately 5-fold (Figure 4A); however, the same effect was not observed with disruption of p85β (Figure 4B). These findings suggest that p85α preferentially functions within the oncogenic KIT-stimulated signaling pathway and that, in spite of significant homology, p85α and p85β are not functionally redundant in KITD814V-induced transformation. In progenitor colony assays, expression of KITD814V in wild-type cells resulted in significantly increased colony formation both in the absence of growth factors (Figure 4C) and in the presence of SCF (Figure 4D). Consistent with the proliferation studies, progenitor colony formation was significantly reduced in p85α−/− cells expressing KITD814V compared with KITD814V-expressing wild-type cells (Figure 4C). Similar results were obtained when progenitors were cultured with SCF (Figure 4D). These findings support the notion that p85α contributes to the transforming ability of KITD814V in HSC/Ps.
Ligand-independent growth due to KITD814V expression in wild-type HSC/Ps is abrogated in the absence of p85α subunit of class IA PI3K, but not in the absence of p85β subunit of class IA PI3K. (A,B) Vector- or KITD814V-expressing wild-type, p85α−/−, or p85β−/− HSC/Ps were subjected to a thymidine incorporation assay in the absence of cytokine stimulation. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 5 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing p85α−/− cells versus wild-type cells. (C,D) Vector- or KITD814V-transduced cells were subjected to an in vitro methylcellulose progenitor colony assay in the absence (C) or presence (D) of SCF 100 ng/mL. Colonies were counted after 10 days of culture. Bars denote the average number of colonies ± SD from 1 of 2 independent experiments performed in triplicate. *P < .05, KITD814V-expressing p85α−/− cells versus wild-type cells.
Ligand-independent growth due to KITD814V expression in wild-type HSC/Ps is abrogated in the absence of p85α subunit of class IA PI3K, but not in the absence of p85β subunit of class IA PI3K. (A,B) Vector- or KITD814V-expressing wild-type, p85α−/−, or p85β−/− HSC/Ps were subjected to a thymidine incorporation assay in the absence of cytokine stimulation. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 5 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing p85α−/− cells versus wild-type cells. (C,D) Vector- or KITD814V-transduced cells were subjected to an in vitro methylcellulose progenitor colony assay in the absence (C) or presence (D) of SCF 100 ng/mL. Colonies were counted after 10 days of culture. Bars denote the average number of colonies ± SD from 1 of 2 independent experiments performed in triplicate. *P < .05, KITD814V-expressing p85α−/− cells versus wild-type cells.
Genetic disruption of Rac2 diminishes growth- factor–stimulated proliferation, but combined deficiency of Rac2 and p85α does not cooperate to reduce ligand-independent proliferation of KITD814V-bearing HSC/Ps
The hematopoietic cell-specific Rho GTPase, Rac2, was considered to be a promising therapeutic target in oncogenic KIT-bearing diseases as Rac is necessary for many PI3K-mediated cellular functions and as products of PI3K activate Rac via activation of guanine exchange factors. To examine the hypothesis that Rac2 contributes to KITD814V-induced hyperproliferation, either wild-type or Rac2−/− bone marrow LDMNCs were transduced with pMIEG3 or pMIEG3-KITD814V and sorted to homogeneity (Figure 5A). Cells were serum and growth factor deprived followed by stimulation with SCF, G-CSF, or M-CSF. Rac2−/− cells expressing KITD814V demonstrated reduced proliferation in response to each of these growth factors as well as in response to combination of these growth factors compared with KITD814V-expressing wild-type cells (Figure 5B), demonstrating that Rac2 also contributes to the HSC/P hyperproliferation induced by KITD814V. We further examined the effect of the combined deficiency of Rac2 and p85α on KITD814V-induced hyperproliferation. The combined deficiency of these molecules very modestly, but not significantly, further reduced the proliferative capacity of KITD814V-bearing p85α−/− cells (data not shown). These findings suggest that although PI3K and Rac2 function within the same KIT-stimulated signaling pathway, PI3K likely regulates the activation of multiple signaling molecules in addition to Rac2. Thus, genetic disruption of p85α leads to a more dramatic inhibition in the growth of cells expressing oncogenic KIT, and the additional disruption of Rac2 contributes only modestly to this inhibition.
KITD814V-induced ligand-independent growth and promiscuous cooperation with other cytokines is inhibited in the absence of Rac2 GTPase in HSC/Ps. (A) Wild-type or Rac2−/− bone marrow LDMNCs were transduced with a retrovirus expressing the empty vector or KITD814V. Transduction efficiency of various constructs in wild-type and Rac2−/− progenitors is shown. (B) EGFP-positive cells in panel A were sorted to homogeneity and subjected to thymidine incorporation assay in the presence of indicated cytokines: no growth factor (NO GF), SCF 50 ng/mL, M-CSF 50 ng/mL, or G-CSF 20 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 3 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing Rac2−/− cells versus wild-type cells in response to indicated stimuli.
KITD814V-induced ligand-independent growth and promiscuous cooperation with other cytokines is inhibited in the absence of Rac2 GTPase in HSC/Ps. (A) Wild-type or Rac2−/− bone marrow LDMNCs were transduced with a retrovirus expressing the empty vector or KITD814V. Transduction efficiency of various constructs in wild-type and Rac2−/− progenitors is shown. (B) EGFP-positive cells in panel A were sorted to homogeneity and subjected to thymidine incorporation assay in the presence of indicated cytokines: no growth factor (NO GF), SCF 50 ng/mL, M-CSF 50 ng/mL, or G-CSF 20 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 3 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing Rac2−/− cells versus wild-type cells in response to indicated stimuli.
Genetic disruption of p85α and Rac2 abrogates ligand-independent and cytokine-stimulated proliferation of KITD814V-expressing MCps
Disruption of p85α or Rac2 significantly reduced the ligand-independent proliferation of HSC/Ps expressing KITD814V, a model system relevant to CBF-AML. We also examined the effect of growth factor stimulation on MCps expressing KITD814V, which is relevant to SM. Briefly, either wild-type, p85α−/−, Rac2−/−, or p85α−/−:Rac2−/− cells were transduced with pMIEG3-WT KIT or pMIEG3-KITD814V, sorted to homogeneity based on EGFP expression, and cultured in IL-3 (10 U/mL) for growth of MCps. Similar to that observed in HSC/Ps, following 8 hours of serum and growth factor deprivation, MCps bearing KITD814V demonstrated increased ligand-independent proliferation (Figure 6). Deficiency of p85α, and to a lesser extent, Rac2, reduced ligand-independent proliferation of MCps expressing KITD814V to near wild-type levels (Figure 6 top left). Consistent with that observed in HSC/Ps, combined deficiency of p85α and Rac2 did not cooperate to reduce MCp proliferation below that of p85α deficiency alone, suggesting that additional PI3K-dependent, but Rac2-independent, pathways contribute to KITD814V-mediated cytokine cooperation and ligand-independent growth. Similar trends were observed upon stimulation with the mast cell growth factors IL-4 or IL-10 or when SCF was combined with IL-4 (Figure 6).
KITD814V-induced ligand-independent growth and promiscuous cooperation with other cytokines is inhibited in the absence of p85α or Rac2 GTPase in MCps. KITD814V-expressing wild-type, p85α−/−, Rac2−/−, or Rac2−/−:p85α−/− MCps were subjected to a thymidine incorporation assay in the absence of cytokine stimulation (NO GF) or in the presence of IL-4 10 ng/mL, IL-10 10 ng/mL, or SCF 50 ng/mL plus IL-4 10 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 2 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing p85α−/−, Rac2−/−, or p85α−/−:Rac2−/− cells versus wild-type cells.
KITD814V-induced ligand-independent growth and promiscuous cooperation with other cytokines is inhibited in the absence of p85α or Rac2 GTPase in MCps. KITD814V-expressing wild-type, p85α−/−, Rac2−/−, or Rac2−/−:p85α−/− MCps were subjected to a thymidine incorporation assay in the absence of cytokine stimulation (NO GF) or in the presence of IL-4 10 ng/mL, IL-10 10 ng/mL, or SCF 50 ng/mL plus IL-4 10 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 2 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing p85α−/−, Rac2−/−, or p85α−/−:Rac2−/− cells versus wild-type cells.
KITD814V-bearing HSC/P hyperproliferation is inhibited by the Rac2 inhibitor, NSC23766, and by the mTor inhibitor, rapamycin
Based on the normalization of KITD814V-bearing HSC/P and MCp hyperproliferation on Rac2−/− and p85α−/− genetic backgrounds, we hypothesized that pharmacologic inhibition of Rac2 or of mTor, a downstream effector of PI3K, would also normalize KITD814V-induced hyperproliferation. Treatment with the Rac2 inhibitor, NSC23766, resulted in a dose-dependent reduction of ligand-independent hyperproliferation of HSC/Ps expressing KITD814V in both wild-type and Rac2−/− cells; however, this effect was more pronounced in the wild-type cells (36% reduction) compared with the Rac2−/− cells (18% reduction, Figure 7A left panel). Rac2 inhibition was also effective at inhibiting SCF-stimulated hyperproliferation (Figure 7A right panel), and this inhibition was again more substantial in wild-type cells (40% reduction) compared with that in Rac2−/− cells (15% reduction). Furthermore, treating WT KIT-expressing cells with NSC23766 in the presence of SCF 50 ng/mL did not affect cellular growth (data not shown). Upon treatment of cells expressing KITD814V with rapamycin, ligand-independent proliferation was dramatically reduced compared with cells expressing WT KIT (Figure 7B). Importantly, treatment of the WT KIT-expressing cells with the indicated concentrations of rapamycin in the presence of SCF did not inhibit proliferation (Figure 7B). Taken together, these findings imply that cells bearing the activating KITD814V mutation are more sensitive to inhibition by NSC23766 or rapamycin compared with cells transduced with empty vector or WT KIT, making investigation of these compounds as potential therapeutic agents in CBF-AML or SM very attractive.
KITD814V-induced ligand-independent and SCF-stimulated growth of hematopoietic progenitors is sensitive to the Rac-GTPase inhibitor, NSC23766, and the mTor inhibitor, rapamycin. (A) KITD814V-expressing wild-type or Rac2−/− bone marrow progenitors were treated with the indicated concentrations of NSC23766 and subjected to a thymidine incorporation assay in the absence of cytokine stimulation (NO GF, left panel) or in the presence of SCF 50 ng/mL (right panel). After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± S.D). *P < .05, KITD814V-expressing wild-type cells treated with 50, 100, or 200 μM NSC23766 versus vehicle (water). (B) WT KIT- or KITD814V-expressing cells were treated with vehicle (ethanol), SCF 50 ng/mL, or the indicated concentrations of rapamycin and subjected to a thymidine incorporation assay. WT KIT-expressing cells treated with rapamycin were also treated with SCF 50 ng/mL. After 24 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 2 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing cells treated with 1 nM or 2 nM rapamycin versus vehicle (ethanol).
KITD814V-induced ligand-independent and SCF-stimulated growth of hematopoietic progenitors is sensitive to the Rac-GTPase inhibitor, NSC23766, and the mTor inhibitor, rapamycin. (A) KITD814V-expressing wild-type or Rac2−/− bone marrow progenitors were treated with the indicated concentrations of NSC23766 and subjected to a thymidine incorporation assay in the absence of cytokine stimulation (NO GF, left panel) or in the presence of SCF 50 ng/mL (right panel). After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± S.D). *P < .05, KITD814V-expressing wild-type cells treated with 50, 100, or 200 μM NSC23766 versus vehicle (water). (B) WT KIT- or KITD814V-expressing cells were treated with vehicle (ethanol), SCF 50 ng/mL, or the indicated concentrations of rapamycin and subjected to a thymidine incorporation assay. WT KIT-expressing cells treated with rapamycin were also treated with SCF 50 ng/mL. After 24 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 2 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing cells treated with 1 nM or 2 nM rapamycin versus vehicle (ethanol).
Discussion
Oncogenic activation loop KIT mutations are observed with high frequency in patients with acute myeloid leukemia (AML) and systemic mastocytosis (SM). Although significant biochemical and functional information has been obtained with respect to how these mutations function, most published work has been performed in heterologous cell lines, such as Ba/F3. Though informative, and perhaps most appropriate for identifying biochemical signals downstream of activating KIT mutations, functional data derived from transformed and/or heterologous cell lines likely do not adequately reveal the true manifestation of these mutations in human disease. For example, the expression and activation of kinases and their downstream transcription factors in primary stem/progenitor cells are likely to differ significantly in comparison with those induced in a pro–B-cell line such as Ba/F3. Adding to the complexity is the unique ability of KIT to synergize with a significant number of hematopoietic-specific cytokines, including IL-3, G-CSF, M-CSF, IL-4, and IL-101. This type of cooperation has been shown to play a critical role in the expansion of bone marrow progenitors. Unfortunately, the extent to which activating KIT mutations cooperate with cytokines and contribute to the overall disease process cannot be fully appreciated by studying factor-dependent heterologous cell lines. To better assess the function of activation loop KIT mutants and to extend previously published observations in cell lines, we have analyzed the impact of expression of KITD814V on HSC/P (relevant to AML) and MCp (relevant to SM) growth and activation of downstream signaling pathways. Using genetic, biochemical, and pharmacologic approaches, our results demonstrate that KITD814V-harboring HSC/Ps and MCps hyperproliferate in response to multiple hematopoietic cytokines and promote promiscuous, aberrant cellular growth via these cytokines. Based on these observations, it is likely that in addition to ligand-independent growth, cooperation with other cytokines might contribute to the overall disease process in patients harboring KITD814V (eg, AML and SM).
Previous studies have suggested the involvement of PI3K in KITD814V-induced ligand-independent growth.15,26 Although instructive and insightful, the conclusions drawn from these studies are limited due to the use of cell line models, dominant-negative approaches, and pharmacologic inhibitors that inhibit all classes of PI3K and, therefore, induce unacceptable levels of toxicity in vivo.31-33 Since cells express multiple classes of PI3K, including class IA and class IB, and since growth factor receptors activate mostly type IA PI3K, an alternate approach to inhibiting PI3K might involve interfering with the function of specific catalytic and/or regulatory subunits of class IA PI3K. In the present study, we have used this approach to specifically address the involvement of p85α and p85β regulatory subunits of class IA PI3K in KITD814V-induced ligand-independent growth and cytokine cooperation. Our reasoning to test this approach is based on the fact that regulatory subunits of class IA PI3K recruit signaling proteins via their Src-homology 3 (SH3), break-cluster region (BCR), and proline-rich (PR) domains and use their Src-homology 2 (SH2) domain for recruitment and activation of the PI3K catalytic subunit.43 Thus, one could potentially use small peptides to inhibit the interactions between the SH2 domain of p85 and receptor phosphotyrosine residues or to interfere with the ability of p85 to bind the p110 catalytic subunit. Alternatively, blocking peptides designed against the SH3, BCR, or PR domains of p85 may inhibit the recruitment of p85 effectors. Such strategies have proved effective in blocking the activation of several kinases.46 To begin to validate some aspects of this strategy and to determine the extent to which these regulatory subunits contribute to ligand-independent growth via KITD814V in relevant cell types, we conducted studies examining the genetic disruption of p85α or p85β on KITD814V-induced growth. Although genetic deletion of p85α did normalize KITD814V-induced ligand-independent proliferation in hematopoietic progenitors, genetic deletion of p85β, an alternative regulatory subunit of the class IA PI3K, had no effect. Interestingly, p85α and p85β subunits share near identity in the known functional domains in the carboxy terminus, including the N-SH2 and C-SH2 domains, which are critical for mediating association with other SH2-containing proteins as well as binding to the p110 catalytic subunit. Furthermore, these domains are shared by the p50α and p55α subunits of class IA PI3K. We speculate that the basis for differential specificity between p85α and p85β for KITD814V is likely to be derived from p85α's amino terminal region. Sequence comparison between p85α and p85β shows significant differences in the amino terminal half of the protein, including the SH3 and the BCR homology domains; therefore, it is likely that p85β recruits a different set of proteins compared with p85α. Structure-function studies to map the regions in p85α involved in KITD814-induced hyperproliferation are ongoing in our laboratory. Taken together, our results suggest that, in spite of the significant homology between p85α and p85β, these regulatory subunits play a nonredundant function within the oncogenic KIT-stimulated signaling pathway and suggest that blocking the regulatory function of p85α, while sparing that of p85β, may provide an effective and relatively specific therapeutic approach to KITD814V-bearing leukemias and SM. This approach is further supported by the fact that p85α−/− mice are viable and have a relatively normal life span. Furthermore, studies have demonstrated relatively normal hematopoietic phenotype in mice lacking the binding site for p85α on the KIT receptor.47,48 Taken together, these results suggest that p85α may play a prominent role in oncogenic KIT-induced transformation as opposed to normal KIT functions, suggesting that inhibiting aspects of p85α function should be well tolerated over a prolonged period.
In addition to directly inhibiting KITD814V or PI3K, we hypothesized that effector molecules of activated PI3K may be potential drug targets in oncogenic KIT-bearing hematologic diseases. We reasoned that inhibition of Rac2 may normalize KITD814V-induced cellular transformation based on previous findings that several PI3K-dependent cellular functions require Rac, that products of PI3K activation stimulate the conversion from inactive Rac-GDP to active Rac-GTP, and that Rac2 is hematopoietic specific. Furthermore, SCF-stimulated hyperproliferation of murine mast cells heterozygous for neurofibromin (Nf1+/−) was normalized upon genetic disruption of Rac2,41 providing additional support for the hypothesis that Rac2 is a potential therapeutic target in oncogenic KIT-induced diseases. HSC/Ps and MCps expressing KITD814V on a Rac2−/− background demonstrated reduced ligand-independent and cytokine-stimulated proliferation to near wild-type levels. Given that Rac2 is a hematopoietic-specific Rho GTPase and that Rac2−/− mice demonstrate only modest hematopoietic abnormalities, these studies suggest that Rac2 may be a specific therapeutic target in oncogenic KIT-bearing diseases. We also examined the effect of combined genetic deletion of p85α and Rac2 in HSC/Ps and MCps. Although genetic deletion of each individual molecule did effectively normalize both ligand-independent hyperproliferation and promiscuous cooperation with multiple cytokines, combined genetic deletion did not further normalize the transformed phenotype. These findings suggest that p85α-induced activation in KITD814V-bearing cells is likely to regulate other downstream molecules, such as mTOR, in addition to Rac GTPases.
Recent studies using a mast cell line (HMC-1) derived from an individual with mast cell leukemia bearing both the juxtamembrane domain mutant KITV560G and the activation loop mutant KITD816V demonstrated resistance to treatment with imatinib but response to rapamycin,49 suggesting that pharmacologic inhibition of KIT effectors may serve as a rational therapeutic approach in SM and CBF-AML. Therefore, to expand our genetic findings, we examined the effect of pharmacologic inhibition of Rac or mTor in HSC/P proliferation using NSC23766 or rapamycin, respectively. NSC23766 was specifically developed as a Rac inhibitor and displays minimal inhibition of the related Rho GTPases, Cdc42 or RhoA.50 Treatment of KITD814V-expressing wild-type HSC/Ps with NSC23766 significantly reduced ligand-independent and SCF-induced hyperproliferation with minimal effect on KITD814V-bearing Rac2−/− cells or on WT KIT-expressing cells. The proliferation of KITD814V-bearing Rac2−/− cells was also susceptible to inhibition by NCS23766, although to a lesser extent than that of wild-type cells, suggesting that while hematopoietic-specific Rac2 contributes significantly to KITD814V-induced hyperproliferation, Rac1 or Rac3 may partially contribute to this process. Thus, it is conceivable that in vivo loss of Rac2 in the setting of KITD814V expression may not completely correct KITD814V-induced transformation. Studies are currently ongoing to address the relative contribution of Rac1, Rac2, and Rac3 in KITD814V-induced transformation. Proliferation of KITD814V-bearing HSC/Ps was also dramatically reduced by nanomolar concentrations of rapamycin, which was not observed in cells expressing WT KIT, suggesting that the mutant-bearing cells are particularly sensitive to the cytotoxic effects of rapamycin. Treatment of individuals with refractory or secondary AML with rapamycin has yielded promising results,51 and currently clinical trials are ongoing to use rapamycin in elderly leukemia patients or in children with relapsed acute leukemia (www.clinicaltrials.gov). Our in vitro findings suggest that Rac inhibitors and rapamycin, or a combination of these agents, may also be efficacious in KITD814V-bearing hematologic malignancies, including AML and SM. Future studies will examine the effect of these compounds as well as p85α and Rac2 deficiency in murine in vivo models of oncogenic KIT-bearing leukemia and mastocytosis.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by R01 HL075816 (R.K.), R01 HL077177 (R.K.), and R01 HL082981 (R.J.C.)
We thank Marilyn Wales for assistance in preparation of the paper and expert administrative assistance.
Authorship
Contribution: V.M. designed and performed research; E.C.S. performed research; J.B. performed research; R.J.C. wrote the paper; R.K. designed research and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Reuben Kapur, Herman B Wells Center for Pediatric Research, Indiana University School of Medicine, Cancer Research Institute, 1044 W Walnut St, Rm 425, Indianapolis, IN 46202; e-mail: rkapur@iupui.edu.

![Figure 2. Expression of KITD814V in HSC/Ps results in ligand-independent growth and promiscuous proliferation in response to multiple cytokines. (A) Bone marrow LDMNCs were transduced with empty vector, WT KIT, or KITD814V. Top panel demonstrates the relative transduction efficiency from one of several experiments as determined by EGFP expression (x-axis). After 48 hours of culture, cells were pulsed with [3H] thymidine in the absence of growth factors for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector or WT KIT. (B) Lin− LDMNCs were transduced with empty vector or KITD814V (top panel). EGFP-positive cells were subjected to thymidine incorporation in the absence of growth factors as described in panel A. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 3 independent experiments performed in quadruplicate. *P < .05, KITD814V versus vector. Bone marrow LDMNCs were transduced with empty vector or KITD814V (C) or with WT KIT or KITD814V (D). EGFP-positive cells were subjected to thymidine incorporation in the presence of indicated cytokines: no growth factor (NO GF), SCF 50 ng/mL, M-CSF 50 ng/mL, G-CSF 20 ng/mL, or IL-3 5 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from one of several experiments performed in quadruplicate. *P < .05, KITD814V versus vector (C) or KITD814V versus WT KIT (D).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/110/5/10.1182_blood-2006-10-053058/6/m_zh80160705870002.jpeg?Expires=1767761950&Signature=h7ehS2xfqu4IraRCEZ0Z6RfLKf~7JvTr5TM7Asq3-e31fDNzZQDJaIZ6fDFh-D9Fmje~kn5KIYAuyKa4cAbyfmsu93N92jFHwUSzrwQkRngoAq8O1CGxgI8ZbIlZN7FvNDg4VEPb3LIJMeNr2h9jxOO5W9183MUSEU9xojMPi6p-8wjRGZ2yz2VBmIUr09PnIldIVxmTNsQm3Bw7s4U9uG1eRsxBrZQD9tiA5LR7M99qZ7j3VJUnIZBMCwuQyQFLRt1W2esqwPWstFXZ8-oYmAY06E8N6ckHoxc62pRTimckIr~akU~1AUS-PHkeMdhLIuLq-HpbsbwE4J~IEG8PiQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. Ligand-independent growth due to KITD814V expression in wild-type HSC/Ps is abrogated in the absence of p85α subunit of class IA PI3K, but not in the absence of p85β subunit of class IA PI3K. (A,B) Vector- or KITD814V-expressing wild-type, p85α−/−, or p85β−/− HSC/Ps were subjected to a thymidine incorporation assay in the absence of cytokine stimulation. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of at least 5 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing p85α−/− cells versus wild-type cells. (C,D) Vector- or KITD814V-transduced cells were subjected to an in vitro methylcellulose progenitor colony assay in the absence (C) or presence (D) of SCF 100 ng/mL. Colonies were counted after 10 days of culture. Bars denote the average number of colonies ± SD from 1 of 2 independent experiments performed in triplicate. *P < .05, KITD814V-expressing p85α−/− cells versus wild-type cells.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/110/5/10.1182_blood-2006-10-053058/6/m_zh80160705870004.jpeg?Expires=1767761950&Signature=HdBmqR~zcW8Y1IhbIfMUmS4MkmNTIM8EBb5Wb5pZnzGeXRAb2zNAi43sJrEOIIm85OQTIJ5tcVb8JkRy7BFVFWchW6NmWe-QWQ4WRCwLXrOzyxoQPLWaHFcUhym44-u6M8M2KT6H4q6tc3TxSXmWwUlPWQli3o7ZJpyM8KHFtNttu1VOkTbs2rHAgY67qnk4jX4mQYs9u-XJ7W9nuBZ0pmd0u18Hr-rz9cwfiKRIRCK8lezTXGO7LqCL8yA4knl0fXtHYWqqfKRLeJjZegaIy3plWxluaDMagnhtks5n3LOpBlmkcoodgDVOpKZcKy-0c5jPkDtm2L6FVLBWGuP3~w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. KITD814V-induced ligand-independent growth and promiscuous cooperation with other cytokines is inhibited in the absence of Rac2 GTPase in HSC/Ps. (A) Wild-type or Rac2−/− bone marrow LDMNCs were transduced with a retrovirus expressing the empty vector or KITD814V. Transduction efficiency of various constructs in wild-type and Rac2−/− progenitors is shown. (B) EGFP-positive cells in panel A were sorted to homogeneity and subjected to thymidine incorporation assay in the presence of indicated cytokines: no growth factor (NO GF), SCF 50 ng/mL, M-CSF 50 ng/mL, or G-CSF 20 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 3 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing Rac2−/− cells versus wild-type cells in response to indicated stimuli.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/110/5/10.1182_blood-2006-10-053058/6/m_zh80160705870005.jpeg?Expires=1767761950&Signature=RuDt7S3YyPeeEGApIbFze76hByuov2baRuWJEzPKyKid57zkGUccimhK-ncexRYb3-SPWBA~AeR~08ddSNQYWKv0s6EVrlZT5-Y075FLxX7L7vZ5EjvFkJ4sPL8oohE48TJkcq43JCN65ywN6fAMlk8iptK~TYLlH6yRCLBu0h4kqvD6AZGc4eZNoZvQdEWM4UTOVhNkze-VhSgpcNCRkUwY66V7DqLm8wydjvFf4DQ0tTRL3fxI7Kpk9hyalQwVtaLDqtuzF~saGvW~lkKbG2Q3nKU7-UNdC-EmcHIt0TXN6AqTe3TdFO8OA-zoKrj0lNoyrT4Tj6jNPmn-Xd8Fog__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. KITD814V-induced ligand-independent growth and promiscuous cooperation with other cytokines is inhibited in the absence of p85α or Rac2 GTPase in MCps. KITD814V-expressing wild-type, p85α−/−, Rac2−/−, or Rac2−/−:p85α−/− MCps were subjected to a thymidine incorporation assay in the absence of cytokine stimulation (NO GF) or in the presence of IL-4 10 ng/mL, IL-10 10 ng/mL, or SCF 50 ng/mL plus IL-4 10 ng/mL. After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 2 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing p85α−/−, Rac2−/−, or p85α−/−:Rac2−/− cells versus wild-type cells.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/110/5/10.1182_blood-2006-10-053058/6/m_zh80160705870006.jpeg?Expires=1767761950&Signature=TqouO4krthNobuRN4m8czubtKOS35CqKjqay8Hji3E0ag6Amm9LiFux1ve0ABnvP3VmgpQk4LcoNaKlmYHCCwMQVvb19hiBKsw~4AgQTJ7yu~NuT5hTbo-nb~FffFrXCmJE9GUk3Mhd430ISUeQqlPltcLhFv107vnRq1B4dCkczHBrEqCY8XcHbSOegukE0OPKDdiV0NPoj6NFlK3nrITinKb81d4UvO19GDjsw1tzXd~bd9UvIpRIcSikt2OuHgQbLoayE00~CnrlRdNRrVcnmn9H2WS5Jusf-3GSj5LaW4DVsMP8ihEq80-KctUX1prKp814fOdmrsFkp9Bu6PA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 7. KITD814V-induced ligand-independent and SCF-stimulated growth of hematopoietic progenitors is sensitive to the Rac-GTPase inhibitor, NSC23766, and the mTor inhibitor, rapamycin. (A) KITD814V-expressing wild-type or Rac2−/− bone marrow progenitors were treated with the indicated concentrations of NSC23766 and subjected to a thymidine incorporation assay in the absence of cytokine stimulation (NO GF, left panel) or in the presence of SCF 50 ng/mL (right panel). After 48 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± S.D). *P < .05, KITD814V-expressing wild-type cells treated with 50, 100, or 200 μM NSC23766 versus vehicle (water). (B) WT KIT- or KITD814V-expressing cells were treated with vehicle (ethanol), SCF 50 ng/mL, or the indicated concentrations of rapamycin and subjected to a thymidine incorporation assay. WT KIT-expressing cells treated with rapamycin were also treated with SCF 50 ng/mL. After 24 hours of culture, cells were pulsed with [3H] thymidine for an additional 6 hours. Bars denote the mean thymidine incorporation (cpm ± SD) from 1 of 2 independent experiments performed in quadruplicate. *P < .05, KITD814V-expressing cells treated with 1 nM or 2 nM rapamycin versus vehicle (ethanol).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/110/5/10.1182_blood-2006-10-053058/6/m_zh80160705870007.jpeg?Expires=1767761950&Signature=D4Uczv9WIOPsK4iwv7GFAnnZDBYj0UBVF~bP85B3JoezHN2OPqd5hbiBSzyfs5S8J--kM1Kk5PTk4JZ9olANf82RaZos~hkGofrb1IDlN8EoaqfZhMb7VRZb6nnYVO8w3W9CekeXd4IZw9rryv31IKV2k6e4MhJ4yVMUjI1wdpyYLZDIl~Im6OjcRdsKjwbg2IN-ml~xzWrz4FqIqe3pVmQoaNWoHRDc5Vv736j4q16CF0-rQ-LTvEQWXYBB-vmpgS0J2DCnoa952ezzFLj0llV3OE4GYuFK1LA~XhrA7NH3fxkiVapuRav02lT6ttR2-ZY-G6lmr8j8nvH1LfdIBw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal