Abstract
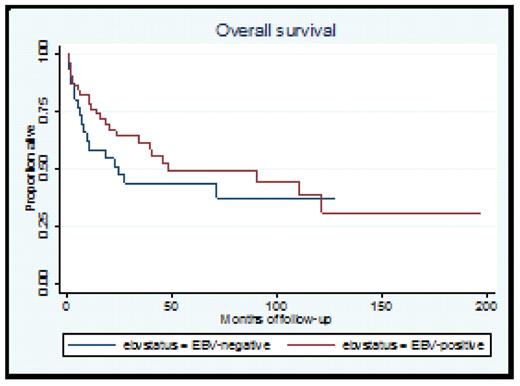
PTLD is a heterogeneous group of neoplasms arising in patients after solid-organ or allogeneic stem-cell transplantation. Although most cases of PTLD are related to Epstein - Barr virus (EBV) infection, a subset (10–20%) shows no association with EBV infection. Anecdotal uncontrolled studies have described EBV-negative PTLD as appearing late in the post-transplant period and having poor response to reduction of immunosuppression and poor outcome in general. We identified 30 patients who were diagnosed with EBV-negative PTLD in the University of Pennsylvania between November 1990 and April 2008. We compared the clinical and pathological characteristics, response to therapy and survival of these patients with 51 control patients matched by organ type who had EBVpositive PTLD. The average age at diagnosis was 53.1 in the EBV (−) group and 49.2 in the EBV (+) group (p=NS). 3/30 (10%) of the EBV (−) cases and 16/51 (31.4%) appeared within the first year after transplant (p<0.05). 7/30 (23%) of the EBV (−) patients and none of the EBV (+) patients had multiple transplants in their history (p<0.005). Presenting signs and symptoms, stage at diagnosis, extranodal involvement and involvement of the allograft were similar in both groups but patients with EBV (−) PTLD were more likely to present with “allograft failure”. Pathological characteristics were significantly different. 27/30 (90%) of EBV(−) cases and 25/38 (66%) of EBV (+) cases had monomorphic PTLD (p<0.05). The majority of the EBV (−) cases were subtyped as diffuse large B-cell lymphoma. 23/30 (76.7%) of EBV (−) PTLD cases and 41/51 (80.4%) of EBV (+) PTLD cases were treated with reduction of immunosuppression (RI) alone as initial therapy. Overall response rates to RI were 47.6% and 58.5% in the EBV (−) and EBV (+) groups respectively (p=NS). Overall response rates to the monoclonal anti-CD-20 antibody rituximab when it was used as a single agent were 47% and 48% in the EBV(−) and EBV (+) groups respectively. In both groups, less than 20% of the patients encountered allograft rejection during therapy and a total of 6 patients (3 in each group) underwent another transplant without having a relapse of their PTLD. 2-year survival rates for EBV (−) and EBV (+) PTLD were 48% and 67% respectively (p<0.05). Kaplan-Meier survival analysis showed a trend towards higher early mortality in EBV (−) patients; however overall survival and disease-free survival were not affected by EBV status by log-rank test (p=0.35 & p=0.84 respectively). Median follow-up on living patients was 60 months (range 3.9–196.9 months). Univariate analysis using the Cox proportional hazards model revealed that stage at diagnosis, B symptoms, initial albumin level, bulky disease and age>60 were significant predictors for poor prognosis in both groups, verifying that some of the classic risk factors for lymphoid malignancies are valid in PTLD. The strongest predictor of mortality was the type of transplanted organ, where lung transplant recipients had the worst outcome and kidney transplant recipients did well (log rank p-value=0.02 for both overall survival and disease-free survival). We conclude that in our single-center series, EBV-negative PTLD is a distinct subtype which appears later in the post-transplant period. Compared with EBV-positive PTLD, it is more likely to be monomorphic and similar to common B-cell malignancies; however it still responds well to reduction of immunosuppression and specific anti-B-cell immunotherapy without compromising allograft survival. It does not necessarily require chemotherapy and can be cured similarly to EBV-positive PTLD.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal