Abstract
Introduction: High-dose melphalan (HDM) with autologous hematopoietic stem cell transplantation (SCT) is an effective treatment for patients (pts) with systemic light chain (AL) amyloidosis. The goal is to achieve complete remission (CR) of the underlying clonal plasma cell disorder which leads to organ response and prolongs overall survival (OS). Most centers use granulocyte colony-stimulating factor (G-CSF) to mobilize stem cells and proceed directly to SCT. However, it is not well investigated whether induction chemotherapy (IC) prior to HDM might improve the long-term results of this intensive treatment approach (Perz et al., BJH 2004; Sanchorawala et al, BMT 2004).
Patients and methods: We performed a retrospective analysis in 100 AL amyloidosis pts transplanted in our centre since 1998. 94 pts received HDM as part of an upfront treatment. Major eligibility criteria were cardiac disease < NYHA stage III and performance status (PS) < 3. Median age of pts at SCT was 57 years (range 35–69 years). Fifty-five pts received a median of 2 IC cycles using VAD-like chemotherapy or pulsed high-dose dexamethasone within two prospective clinical trials. In 93 pts stem cell collection was performed after mobilization chemotherapy. Due to age >65 years or reduced PS (Karnofsky performance score <80%) the HDM dosage was reduced from 200 to 140 mg/m2 in 16 pts. HDM dosage was adapted to impaired renal function (creatinine clearance <60 ml/min to 85%, <45 ml/min to 75%, <30 ml/min to 70%, in dialysis pts to 50%) in 27 pts. Hematological remission (HR: CR or partial remission (PR)) and organ response were evaluated using Consensus Criteria (Gertz et al. Am J Hematol 2005).
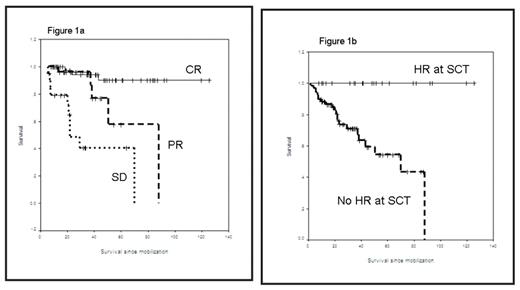
Results: Median follow-up since stem cell mobilization is 28 months (range 10–126). Transplant-related mortality was very low with 3% and could be reduced significantly since 2004 (1998 – 2004 vs 2005 – 2007, 7% vs. 0%, p=0.05). Median OS has not been reached. CR after HDM was achieved in 42/95 evaluable pts (44%) and PR in 35%. This resulted in an improved OS for HR pts (CR vs. PR vs. SD: median OS not reached vs. 88 vs. 22 months, respectively, p<0.001, Figure 1a). HR post SCT led to organ response in 40/92 evaluable pts (43%) and stabilization of organ function in 47% of pts. Of the 55 pts with IC 23 pts (42%) had achieved HR at SCT. Patients with IC had a higher CR rate after HDM (58% vs 29%, p<0.01). Consecutively, pts with HR at SCT showed an increased CR rate post HDM (70% vs 33%, p<0.005). This resulted in a significant prolonged OS (median not reached vs. 5 years, p<0.0001, Figure 1b). Pts receiving full-dose HDM had a longer OS (p=0.02) as well.
Conclusion: Patients with AL amyloidosis who respond to pre-transplant IC have an excellent prognosis after HDM. This finding facilitates identification of those patients who particularly benefit from SCT and warrant prospective studies with new and more effective drugs for induction therapy to confirm and even improve these promising results.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal