To the editor:
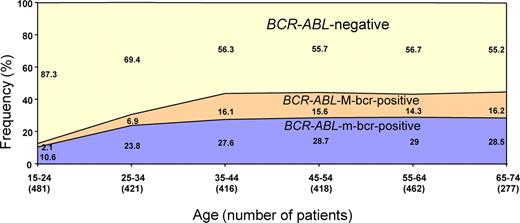
The frequency of BCR-ABL is higher in adults than in children with acute lymphoblastic leukemia (ALL). We analyzed data from a large number of patients obtained within the framework of the central diagnostics of various GMALL (German Multicenter ALL) study group trials between 1990 and 2007 (www.ClinicalTrials.gov: NCT00199069, NCT00199056, NCT00198991). Investigations were done primarily at the central diagnostic laboratory of the GMALL study group in Berlin and, from 1990 to 2000, also in part at the University of Heidelberg. Overall, 2544 primary cell samples from patients with B-precursor (pro-B, common, pre-B) ALL (age 15-74 years) were diagnosed and investigated for BCR-ABL transcripts with 2 different polymerase chain reaction (PCR) methods as previously described in detail.1,2 Forty-six (1.8%) cases showed an ambiguous result and were not considered for further analysis. Of the remaining 2498 cases, 904 (36.2%) were BCR-ABL+ (599 = 24% minor breakpoint region [m-bcr] and 282 = 11.3% major breakpoint region [M-bcr], 15 = 0.6% both, M-bcr and m-bcr, and 8 atypical transcripts), and 1594 were BCR-ABL−. Atypical transcripts were not systematically detected before 20001 and thus had to be excluded from further analysis. We grouped patients into age cohorts at 10-year intervals according to their age at diagnosis, each comprising between 277 and 481 patients and found a remarkable increase of BCR-ABL frequency in adolescents and young adults (Figure 1). It increased from 12.7% in adolescents (15-24 years) to 30.6% and 43.7% in patients aged 25 to 34 and 35 to 44 years, respectively. In patients older than 44 years, the BCR-ABL frequency showed no further increment and ranged between 42% and 44%. The increase of BCR-ABL frequency was paralleled by a relative increase of M-bcr transcripts. These transcripts accounted for 16.4% of all BCR-ABL-positive cases in adolescents (15-24 years). Their relative frequency increased to 22.5% in 25- to 34-year-olds and to 36.8% in 35- to 44-year-olds and remained between 33% and 36.2% from then on.
Frequencies of BCR-ABL in B-precursor ALL according to age groups. Fifteen (0.6%) patients showed both types of transcripts (M-bcr and m-bcr) and were not included in this diagram.
Frequencies of BCR-ABL in B-precursor ALL according to age groups. Fifteen (0.6%) patients showed both types of transcripts (M-bcr and m-bcr) and were not included in this diagram.
The reason for this age dependency is not obvious. The relative frequencies of immunologic subtypes (78.2% common, 19.9% pre-B, 1.9% pro-B) of BCR-ABL+ patients did not differ significantly across the age groups. Moreover, the frequency of BCR-ABL was also not significantly different in woman compared with men. Our study excluded lymphatic blast crises in patients with known chronic myeloid leukemia (CML). Previous work has indicated that M-bcr– and m-bcr–positive ALL may arise from different sets of hematopoietic progenitor cells,3 but this does not explain the age dependency. A number of genetic markers in ALL show a marked age dependency (reviewed in Armstrong and Look4 ), eg, TEL-AML1, TLX1, and TLX3, MLL aberrations (especially in infant ALL). Our data provide additional information on the biology of BCR-ABL-positive ALL and substantiate evidence of age-dependent variation in the genetic background of ALL.
Authorship
This work was supported in part by the Deutsche Krebshilfe (German Cancer Aid), Bonn, Germany.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dr Thomas Burmeister, Charité Universitätsmedizin Berlin, Campus Benjamin Franklin, Medizinische Klinik III, Hindenburgdamm 30, 12200 Berlin, Germany; e-mail: thomas.burmeister@charite.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal