Abstract
Members of the caudal (cdx) family of homeobox proteins are essential regulators of embryonic blood development in zebrafish. Previously, we reported that the murine homologues (Cdx1, Cdx2, and Cdx4) affect formation and differentiation of embryonic stem cell (ESC)–derived hematopoietic progenitor cells. Consistent with the notion that embryonic pathways can reactivate during adult oncogenesis, recent studies suggest involvement of CDX2 in human acute myeloid leukemia (AML). Here we study CDX2 in healthy and leukemic human lymphoid cells, and show that a majority of leukemic samples display various degrees of aberrant CDX2 expression. Analysis of a cohort of 37 childhood acute lymphoblastic leukemia (ALL) patients treated in our hospital reveals that high CDX2 expression levels at diagnosis correlate with persistence of minimal residual disease (MRD) during the course of treatment. Thus, CDX2 expression levels may serve as a marker for adverse prognosis in pediatric ALL.
Introduction
Cdx genes are classically known as regulators of axial elongation and anterior-posterior patterning during early embryogenesis. Recent studies have revealed an unsuspected role during hematopoietic development: in zebrafish embryo, cdx1a and cdx4 redundantly induce blood formation via activation of specific posterior hox genes.1,2 During in vitro differentiation of embryonic stem cells (ESCs), the 3 murine Cdx genes (Cdx1, Cdx2, and Cdx4) also modulate Hox gene expression,3-6 thereby participating in mesodermal patterning to blood fate4 and regulation of preformed hematopoietic progenitors.5
Little is yet known about the role of CDX genes in human hematopoiesis. The ETV-CDX2 fusion gene has been identified in a patient with acute myeloid leukemia (AML) carrying the rare translocation t(12;13)(p13;q12).7 Recently, aberrant CDX2 expression was detected in most cases of AML.8,9 Currently available studies have focused on CDX2 in AML, possibly because retroviral overexpression of Cdx2 in murine bone marrow promotes AML.8 However, during hematopoietic development from ESCs, Cdx4 overexpression enhances formation of progenitors with lymphoid repopulation capacity,6 suggesting involvement of Cdx genes in lymphopoiesis. Moreover, aberrant expression of potential (HOX) target genes has been observed in acute lymphoblastic leukemia (ALL).10-12 Here we determine CDX2 expression in healthy and leukemic lymphoid cells, and explore the prognostic impact of CDX2 transcript quantitation for the clinical course of pediatric ALL by analyzing a cohort of 37 patients.
Methods
Bone marrow (BM) and peripheral blood (PB) samples were collected from healthy donors and patients presenting with leukemia. All patients, or when appropriate their legal guardian, gave their written informed consent form in accordance with the Helsinki protocol, and the study was performed according to the guidelines of the Ethics Committee of the University of Tuebingen, Tuebingen, Germany. In pediatric ALL, we followed a cohort of 37 patients treated in our hospital between 2003 and 2008. Induction therapy was applied according to the ALL-BFM protocol, and minimal residual disease (MRD) diagnosis performed as previously described.13,14 Patients' characteristics are shown in Table S1, available on the Blood website; see the Supplemental Materials link at the top of the online article. Here we describe only briefly the processing of samples that is presented in more detail in Document S1: a LightCycler carousel-based system and LightCycler TaqMan Master chemistry (Roche, Mannheim, Germany) were used for real-time reverse-transcription polymerase chain reaction. Relative CDX2 expression levels were calculated after normalization to the housekeeping gene PBGD. Statistical analysis was performed using the Wilcoxon rank test (SAS system, procedure NPAR1WAY; SAS Institute, Cary, NC) and the Fisher exact test (SAS system, FREQ Procedure).15 The significance level α equals .04 for all tests.
Results and discussion
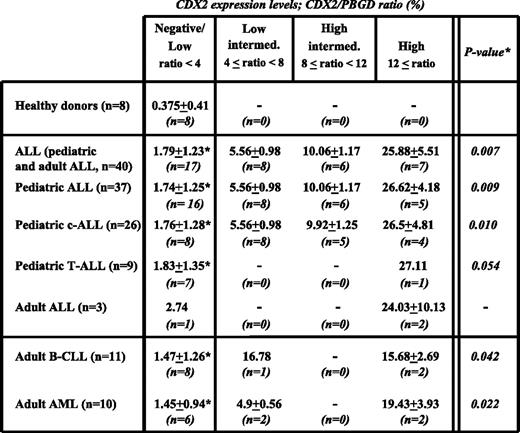
Cdx genes regulate hematopoiesis by modulating posterior Hox genes during embryonic development.1-6,16 In adults, Cdx4 but not Cdx2 expression was detected in murine bone marrow.8,17 CDX2 was not expressed in healthy human BM mononuclear cells (MNCs), isolated CD34+, or myeloid progenitor cells.8 In our laboratory, analysis of healthy donor BM, PB, and purified B (CD19+), T (CD3+), or natural killer (NK; CD56+) cells showed negative or very low CDX2 expression (defined as CDX2/PBGD [%] 0 < ratio < 1; Figure S1A), whereas MNCs collected from patients presenting with AML expressed CDX2 in 9 of 10 cases, which is line with previously reported results8 (Table 1A). In contrast, aberrant CDX2 (defined as CDX2/PBGD ratio [%] 1 ≤ ratio) was found in 3 of 7 analyzed lymphoid neoplastic cell lines, with highest levels in NALM-16 cells derived from a patient with pediatric ALL (Figure S1B). Translation into aberrant CDX2 protein was confirmed (Figure S1C). Next, we determined CDX2 transcripts in primary samples collected from patients with pediatric ALL. CDX2 expression was detected in all common ALL (c-ALL), and the majority of analyzed T-cell ALL (T-ALL) samples (78%). Overall, only 6 of 37 pediatric ALL patients (16%) showed negative or very low CDX2 expression comparable with levels in healthy donors. CDX2 expression was similarly high in 3 adult ALL samples (Figure 1). Two samples from pediatric ALL patients revealed extremely high expression (CDX2/PBGD ratio 288.16% and 107.46%, respectively) and were thus considered outliers and not included in the statistical analysis. Among the remaining 35 pediatric ALL patients, mean expression was 7.59 (expression range, 0 to 32.88). Patients were divided into 4 groups: negative/low expressers (CDX2/PBGD ratio [%] 0 ≤ ratio < 4), low-intermediate expressers (4 ≤ ratio < 8), high-intermediate expressers (8 ≤ ratio < 12), and high expressers (12 ≤ ratio). The negative/low expressers group comprised all samples from healthy donors (Figure 1). Even in this group, mean CDX2/PBGD ratio (%) in pediatric ALL patients (1.74 ± 1.25) was significantly higher than in healthy controls (0.375 ± 0.41) (Wilcoxon rank test, 1-sided, P = .009), whereas no significant differences were noted among c-ALL (1.76 ± 1.28), T-ALL (1.83 ± 1.35), and AML (1.45 ± 0.94) (Figure 1). To explore whether CDX2 was specific to acute leukemia or also a feature of other lymphatic neoplasias, samples from 11 patients with chronic lymphocytic leukemia (CLL) were included in the study. More frequently than ALL patients, CLL patients belonged to the negative/low expressers group (72% vs 43%; Figure 1). Our data suggest that high CDX2 levels may correlate with more aggressive disease. However, analysis of more CLL samples is needed for conclusive comparisons.
High CDX2 transcript levels correlate with poor elimination of MRD in pediatric ALL
| CDX2 expression . | Pediatric ALL, no. of patients . | ||
|---|---|---|---|
| MRD point in time 1 . | MRD point in time 2 . | ||
| Positive . | Negative . | ||
| CDX2/PBGD ratio, % 0 ≤ ratio < 4 | 8 | 3 | 5 |
| CDX2/PBGD ratio, % 4 ≤ ratio | 9 | 9 | 0 |
| CDX2 expression . | Pediatric ALL, no. of patients . | ||
|---|---|---|---|
| MRD point in time 1 . | MRD point in time 2 . | ||
| Positive . | Negative . | ||
| CDX2/PBGD ratio, % 0 ≤ ratio < 4 | 8 | 3 | 5 |
| CDX2/PBGD ratio, % 4 ≤ ratio | 9 | 9 | 0 |
Negative/low CDX2 expressers convert significantly better from positive MRD status at MRD point in time 1 to negative MRD status at MRD point in time 2, in comparison with pediatric ALL patients showing higher initial CDX2 transcripts (CDX2/PBGD ratio [%] 4 ≤ ratio). (SAS procedure FREG; Fisher exact test, P = .016).
CDX2 expression in leukemic and healthy control primary BM and PB samples. Patients presenting with leukemia show significantly higher CDX2 expression than healthy controls. CDX2/PBGD ratio (%) was analyzed for leukemia and healthy donor BM or PB samples. Healthy donors and leukemia patients were grouped according to their CDX2/PBGD ratio (%): low expressers (0 ≤ ratio < 4); low-intermediate expressers (4 ≤ ratio < 8); high-intermediate expressers (8 ≤ ratio < 12); and high expressers (12 ≤ ratio). Numbers represent mean CDX2/PBGD ratio (%) ± SD in each subgroup consisting of n patients. *Significant differences between low expressers from leukemia groups compared with the healthy controls, as determined by Wilcoxon 2-sample, 1-sided test, SAS system, NPAR1WAY procedure. ALL indicates acute lymphoblastic leukemia; c-ALL, common acute lymphoblastic leukemia; T-ALL, T-cell acute lymphoblastic leukemia; B-CLL, B-cell chronic lymphocytic leukemia; and AML, acute myeloid leukemia.
CDX2 expression in leukemic and healthy control primary BM and PB samples. Patients presenting with leukemia show significantly higher CDX2 expression than healthy controls. CDX2/PBGD ratio (%) was analyzed for leukemia and healthy donor BM or PB samples. Healthy donors and leukemia patients were grouped according to their CDX2/PBGD ratio (%): low expressers (0 ≤ ratio < 4); low-intermediate expressers (4 ≤ ratio < 8); high-intermediate expressers (8 ≤ ratio < 12); and high expressers (12 ≤ ratio). Numbers represent mean CDX2/PBGD ratio (%) ± SD in each subgroup consisting of n patients. *Significant differences between low expressers from leukemia groups compared with the healthy controls, as determined by Wilcoxon 2-sample, 1-sided test, SAS system, NPAR1WAY procedure. ALL indicates acute lymphoblastic leukemia; c-ALL, common acute lymphoblastic leukemia; T-ALL, T-cell acute lymphoblastic leukemia; B-CLL, B-cell chronic lymphocytic leukemia; and AML, acute myeloid leukemia.
Pediatric ALL is the most common malignancy of childhood, and is treated with chemotherapy alone or in combination with radiation therapy and, in selected cases, with allogeneic stem cell transplantation. Long-term cure and survival rates have significantly improved by adapting therapy intensity to prognostic factors associated with disease aggressiveness and recurrence. Currently, the most important prognostic parameter represents the early in vivo evaluation of therapy response by measuring leukemic cell persistence after induction therapy (minimal residual disease, MRD).13,14,18 We questioned whether CDX2 expression at diagnosis could predict course of the disease by analyzing association with MRD13,14 measured at the point in time 1 (day 33 after start of chemotherapy—first regeneration during induction therapy) and the point in time 2 (2 weeks after completion of induction around day 80). MRD assessment was performed in 30 of 37 patients. At the point in time 1, 17 of 30 analyzed patients were MRD positive. At the point in time 2, 5 of these 17 patients became MRD negative, whereas in 12 patients leukemic cells persisted. There was no MRD-positive patient at the point in time 2 who was previously MRD negative. MRD positivity at the point in time 1 was seen in a comparable number of CDX2 negative/low expressers (n = 8) and patients with initial CDX2/PBGD ratio (%) 4 ≤ ratio (n = 9). However, conversion rates between MRD points in time 1 and 2 were significantly better for negative/low CDX2 expressers, compared with patients with higher initial CDX2 expression (conversion to MRD negativity 62.5% vs 0%, P = .016, Fisher exact test; Table 1). Our data suggest that CDX2 expression levels at disease manifestation may be used to anticipate therapy response in patients showing positive MRD at day 33. At this point, it remains speculative whether leukemic blasts with low CDX2 expression levels may have a different biology than blasts with high CDX2 expression, and whether the latter are specifically resistant to the chemotherapy regimen applied between MRD points in time 1 and 2 (consisting mainly of cyclophosphamide and low-dose cytarabine), rather than to the intensive induction regimen applied prior to day 33 (consisting of high-dose steroids, daunorubicine, asparaginase, and vincristine). Analysis of larger cohorts of patients and replication in independent samples from different populations should further support the validity of this association and determine whether patients with higher CDX2 expression would benefit from alterations of current treatment protocols.
In summary, our study demonstrates that aberrant CDX2 expression is not a specific feature of myeloid neoplasia, but also extends to lymphoid neoplasia. CDX2 expression at diagnosis can be correlated with the clinical course of pediatric ALL and may be useful as a risk stratification marker in patients with pediatric ALL.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study was supported by the Max-Eder-Program of the Deutsche Krebshilfe (Bonn, Germany), and grants from the Deutsche Forschungsgemeinschaft SFB773 (Bonn, Germany), the University of Tuebingen Fortüne Program, and the Wilhelm-Schuler-Foundation (Tuebingen, Germany) for C.L.
Authorship
Contribution: T.R., M.E., and F.G. designed and performed experiments, and analyzed results; H.R.S. contributed critical samples; J.T. performed statistical analysis; L.K. designed the research and reviewed the paper; R.H. designed the research; C.L. designed the research, analyzed results, and composed this paper; and all authors contributed to editing of the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Claudia Lengerke, Department of Hematology/Oncology, University of Tuebingen Medical Center II, Otfried-Mueller Strasse 10, 72076 Tuebingen, Germany; e-mail: claudia.lengerke@med.uni-tuebingen.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal