Abstract
Radioimmunotherapy (RIT) options for T-cell non-Hodgkin lymphomas (T-NHLs) are limited. We evaluated anti-CD45-RIT in human (h) and murine (m) T-NHL. CD45 was highly expressed on hT-NHL patient samples (median, 2.3 × 105 antigen-binding capacity units/cell) and hT-NHL cell lines (3.4 × 105 CD45 antigen-binding capacity units/cell). Biodistribution studies in hTNHL xenografts showed that 131I-labeled BC8 (anti-hCD45) delivered 154% (P = .01) and 237% (P = .002) more radioiodine to tumor sites over control antibodies at 24 hours and 48 hours, respectively. Importantly, tumor sites targeted with 131I-BC8 exhibited 2.5-fold (P = .05), 3.0-fold (P = .007), and 3.6-fold (P = .07) higher 131I retention over the nontarget organs of lungs, liver, and kidneys, respectively (24 hours). Because the clinical use of anti-hCD45 would target both T-NHL and other hematolymphoid tissues, we evaluated the ability of anti-mCD45 to target mT-NHL. mT-NHL grafts targeted with anti-mCD45 correspondingly retained 5.3 (P < .001), 5.4 (P < .001), and 8.7 (P < .001) times the radioactivity in tumor sites compared with nontarget organs of lung, liver, and kidney. 131I-labeled BC8 therapy yielded improved complete remission rates (75% vs 0%, P < .001) and progression-free survivals (median, 23 days vs 4.5 days, P < .001) compared with controls. These data indicate that the high CD45 expression of T-NHL allows reliable tumor targeting and disease control supporting anti-CD45 RIT for T-NHL patients.
Introduction
T-cell non-Hodgkin lymphomas (T-NHLs) encompass a heterogeneous group of high-risk diseases characterized by inferior response rates, remission durations, and survivals compared with their B-NHL counterparts.1-5 Radioimmunotherapy (RIT) has emerged as one of the most efficacious new treatment approaches for B-NHL,6-10 yet for T-NHL this strategy has been thwarted in part because of the lack of a successful, widely applicable radioimmunoconjugate for this antigenically diverse group of malignancies.11 CD45, a panhematopoietic antigen, represents an attractive target for RIT based on its lack of shedding or internalization and its reported expression by the majority of T-NHL.12-15 The broad hematopoietic expression of CD45, though requiring hematopoietic stem cell transplantation (HSCT), also carries the theoretical advantage of amplifying the radiation dose to minimal disease sites via the “crossfire effect” from targeting adjacent CD45-bearing cells
We hypothesize and test in a preclinical model the potential efficacy of anti-CD45 RIT for the treatment of T-NHL. In a succession of experiments, we first demonstrate that CD45 is reliably expressed in high concentrations on T-NHL cell lines and patient samples to facilitate targeting. Furthermore, we illustrate that anti-CD45 RIT results in preferential radiation exposure to tumor sites and limits exposure to nontarget tissues in both xenogeneic and syngeneic systems. Finally, we show that anti-CD45 RIT yields effective tumor control and improved progression-free survival (PFS) in preclinical models. These findings set the stage for translating this strategy into a clinical application of anti-CD45 RIT for patients with T-NHL.
Methods
Cells
The human T-NHL lines CCRF-CEM, HUT-78, and Karpas 299 were purchased from ATCC (Manassas, VA). All cell lines were kept in log growth phase in RPMI 1640 supplemented with 10% fetal bovine serum, 100 U/mL penicillin, 100 U/mL streptomycin (Invitrogen, Carlsbad, CA), and 1% 100× L-glutamine (Invitrogen). Cell viability was kept at more than 95% as measured by trypan blue exclusion. Patient samples were obtained using University of Washington Institutional Review Board–approved methods.
Antibodies and radiolabeling
BC8 (a murine anti–human IgG1) was produced from a hybridoma using a hollow fiber bioreactor system in the Biological Production Facility at the Fred Hutchinson Cancer Research Center. BHV-1 (a murine IgG1, isotype-matched nonbinding control for BC8) was produced using the ascities method and purified using a HiTrap protein G column (GE Healthcare, Little Chalfont, United Kingdom).16 30F11 (rat anti–murine IgG2b) was purchased from BD Biosciences PharMingen (San Diego, CA). BHV-1 and 30F11 were iodinated with Na131I or Na125I (PerkinElmer Life and Analytical Sciences, Waltham, MA) by the chloramine T method as previously described.17
Antigen density of cell lines and patient samples
All samples were evaluated on a modified 4-laser, 10-color BD Biosciences LSRII flow cytometer (San Jose, CA) using the following laser-fluorochrome combinations: (1) 405 nm violet laser (one color), Pacific Blue (PB); (2) 488 nm blue laser (5 colors), fluorescein isothiocyanate (FITC), phycoerythrin (PE), PE–Texas Red (ECD/PE-TR), PE–Cyanine-5 (PE-Cy5), Pe-Cy5.5, and PE-Cy7; (3) 594 nm yellow laser (1 color), Alexa Fluor 594; and (4) 633 nm red laser (3 colors), allophycocyanin (APC), APC–Alexa Fluor 700 (APC-A700), and APC-Cy7.
CD45 antigen density (measured as antigen-binding capacity [ABC]/cell) on neoplastic cells from human blood, bone marrow, and lymph node suspension samples and cell lines were performed according to the manufacturer's protocol (www.bangslabs.com). The microbeads (Quantum Simply Cellular anti–mouse IgG; Bangs Laboratories, Fishers, IN) used in these studies are coated with known quantities of goat anti–mouse IgG which, when mixed with saturating quantities of mouse anti–CD45-PE, produced a standard to measure CD45 density on the CD45-PE–labeled cells of interest.
To create the standard curve, 1 drop of blank and each of the labeled components (beads 1-4), were individually added to 50 μL phosphate-buffered saline/bovine serum albumin (PBS/BSA). A total of 20 μL (titered previously to determine amount of antibody required for saturation) of anti–CD45-PE antibody (clone J33; Beckman Coulter, Fullerton, CA) was added to all mixtures except for the blank. After 30 minutes of incubation in the dark, 2 mL PBS/BSA was added to each tube, and the tubes were centrifuged (> 3500g for 5 minutes). The pellets were then washed twice with PBS/BSA, centrifuged, and resuspended in 100 μL PBS/BSA for analysis.
For each patient specimen or cell line, a custom combination of fluorescently labeled antibodies were used to uniquely identify the neoplastic T-cell population based on the previously determined neoplastic immunophenotype (eg, CD2-FITC, CD34-ECD, CD8-PECy5.5, CD3-PECy7, CD4-A594, CD7-APC, and CD5-APC-Cy7). To approximately 300 000 cells, the custom antibody combinations and anti-CD45-PE were added, and the mixture incubated for 15 minutes at 25°C in 100 μL RPMI, lysed, and fixed with 0.15 M ammonium chloride (Polysciences, Warrington, PA), pH 4.8, containing 0.25% formaldehyde for 15 minutes, washed with 3 mL PBS/BSA, and incubated with 0.1 mL PBS before analysis. Standards and patient samples or the cell line cells were then evaluated by flow cytometry. For the standards, a plot of mean fluorescent intensity in the PE channel versus log (ABC) defined a standard curve. The antigen density of the patient specimen or cell line was determined from this standard curve after the mean fluorescent intensity of the neoplastic population was measured. Both the cell lines and the patient specimens were measured in triplicate.
In vivo studies
Biodistribution.
For all mouse studies, female athymic nude mice, 6 to 8 weeks of age, were purchased from Harlan Sprague-Dawley (Indianapolis, IN) and housed and cared for according to protocols approved by the Fred Hutchinson Cancer Research Center Institutional Animal Care and Use Committee. CCRF-CEM (2 × 107) or Karpas (2 × 107) cells were injected subcutaneously in the right flank and palpable xenografts developed within approximately 10 days. EL-4 (107) cells were injected as in the previous sentence and palpable xenografts developed within 3 days.
Groups of at least 5 mice were coinjected with 200 μg 131I-BC8 and 125I-BHV-1 or 125I-30F11 labeled with 10 μCi radioisotope via the tail vein. The mice were killed 24 or 48 hours after radiolabeled antibody injection, and blood, normal organs (lungs, liver, spleen, kidneys, stomach, large intestine, and small intestine), and tumors were harvested and weighed. Residual radioactivity in the harvested tissues was determined via gamma counter measurements. Using an aliquot of the injectate, the percentage-injected dose of 131I and 125I per gram (%ID/g) of blood, tumor, and normal organs was calculated, and corrections for radioactive decay and crossover were made. Tumor-to-normal organ ratios of absorbed radioactivity were calculated from these data.
Therapy.
T-NHL xenografts were established as in “Biodistribution.” When tumors were measurable (∼100 mm3), groups of at least 9 mice each were injected via tail vein with 200 μg BC8 labeled with 300 or 400 μCi 131I or BHV-1 labeled with 300 μCi 131I. Tumor size and body weight were measured sequentially approximately 3 times weekly after injections. Tumor progression was scored after 2 consecutive increases in tumor volume. Mice were killed when they experienced weight loss more than 20% or tumor size more than 16 mm × 16 mm × 9 mm, per animal health guidelines.
Statistical considerations
Continuous variables with normal distributions were compared using the Student t test. Simple proportions were evaluated using the χ2 or Fisher exact test as appropriate. Time-dependent variables (eg, survival, disease progression) were estimated using the method of Kaplan and Meier, and comparisons between these estimates were made using the log-rank test.18
Results
CD45 is readily expressed on T-NHL lines and patient samples
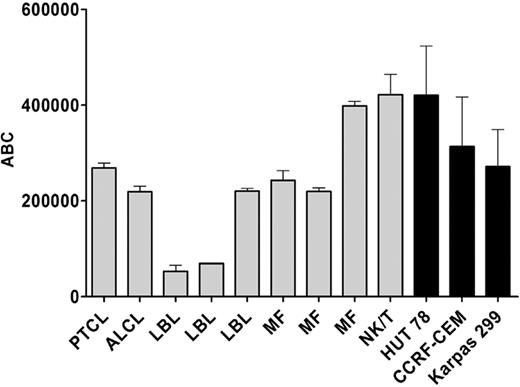
We first quantified the surface density of CD45 on T-NHL lines and T-NHL patient tumor samples to determine whether CD45 expression would be sufficient to serve as a target for RIT and whether subsequent animal models using T-NHL lines would be representative of clinical T-cell lymphoma. The antigen density (ABC) of CD45 was determined for T-NHL lines (CCRF-CEM, Karpas 299, HUT-78) and bone marrow, blood, and lymph node samples from patients with known T-NHL (T-lymphoblastic leukemia/lymphoma [T-LBL], anaplastic large cell lymphoma [ALCL], peripheral T-cell lymphoma, mycosis fungoides [MF], and NK/T-cell lymphoma) as described in “Methods.” CD45 was expressed in high copy numbers on the surface of human T-NHL samples and T-NHL cell lines with a median of 3.4 × 105 ABC units/cell on T-NHL lines (CCRF-CEM, Karpas 299, HUT-78) and 2.3 × 105 ABC units/cell on 9 patient-derived T-NHL specimens (Figure 1). Taken together, these data indicate that the high CD45 expression in cell lines recapitulates most patient-derived T-NHL and, thus, should represent a viable target for RIT.
Mean and SDs of antigen density (ABC) of CD45 on T-NHL patient samples and T-NHL lines.  indicates patient samples; and ■, T-NHL lines. PTCL indicates peripheral T-cell lymphoma; ALCL, anaplastic large cell lymphoma; LBL, T-lymphoblastic leukemia/lymphoma; MF, mycosis fungoides; and NK/T, NK/T-cell lymphoma, nasal type.
indicates patient samples; and ■, T-NHL lines. PTCL indicates peripheral T-cell lymphoma; ALCL, anaplastic large cell lymphoma; LBL, T-lymphoblastic leukemia/lymphoma; MF, mycosis fungoides; and NK/T, NK/T-cell lymphoma, nasal type.
Mean and SDs of antigen density (ABC) of CD45 on T-NHL patient samples and T-NHL lines.  indicates patient samples; and ■, T-NHL lines. PTCL indicates peripheral T-cell lymphoma; ALCL, anaplastic large cell lymphoma; LBL, T-lymphoblastic leukemia/lymphoma; MF, mycosis fungoides; and NK/T, NK/T-cell lymphoma, nasal type.
indicates patient samples; and ■, T-NHL lines. PTCL indicates peripheral T-cell lymphoma; ALCL, anaplastic large cell lymphoma; LBL, T-lymphoblastic leukemia/lymphoma; MF, mycosis fungoides; and NK/T, NK/T-cell lymphoma, nasal type.
Anti–human CD45 RIT targets human T-NHL xenografts
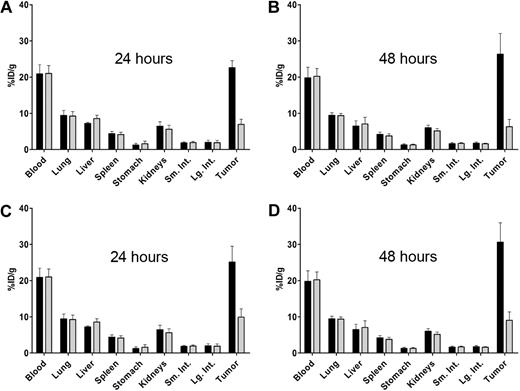
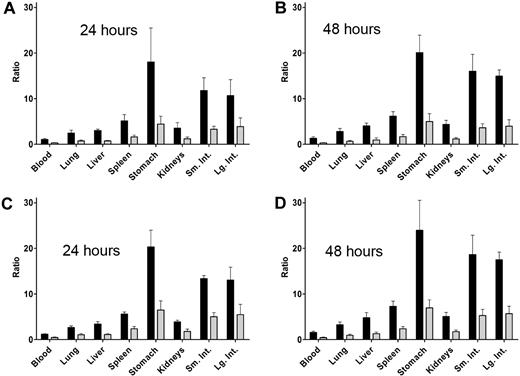
We next determined whether the high expression of CD45 in T-NHL could be used to target human T-NHL xenografts in mouse models. Groups of more than or equal to 5 mice with palpable human T-NHL (Karpas 299, CCRF-CEM) xenografts were coinjected via the tail vein with 200 μg 131I-BC8 (anti-CD45) and 200 μg 125I-BHV-1 (control) labeled with 10 μCi radioisotope followed by tumor and normal organ harvest at 24 and 48 hours. CCRF-CEM xenografts targeted with 131I-BC8 demonstrated 154% (P = .01) and 237% (P = .002) more radioiodine retention at 24 hours and 48 hours, respectively (Figure 2A,B). Likewise, when Karpas 299 xenografts were targeted with BC8, they retained 223% (P = .002) and 313% (P < .001) more radioiodine than the isotype-matched control BHV-1 (Figure 2C,D). More importantly, tumor sites retained more activity than the critical nontarget organs. For example, T-NHL (CCRF-CEM) xenografts exhibited 2.5-fold (P = .05), 3.0-fold (P = .007), and 3.6-fold (P = .07) higher 131I retention compared with the lungs, liver, and kidneys, respectively, at 24 hours (Figure 3A). Similar preferential tumor targeting was observed at 48 hours and in Karpas 299 xenografts (Figure 3B-D).
Biodistribution of 131I-BC8 (anti-CD45) and 125I-BHV-1 (control) in a human T-NHL xenograft model. Biodistributions quantified as percentage injected radioiodine dose/g tissue (%ID/g) of 131I-BC8 (anti-CD45, ■) and 125I-BHV-1 (control,  ) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
Biodistribution of 131I-BC8 (anti-CD45) and 125I-BHV-1 (control) in a human T-NHL xenograft model. Biodistributions quantified as percentage injected radioiodine dose/g tissue (%ID/g) of 131I-BC8 (anti-CD45, ■) and 125I-BHV-1 (control,  ) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
Tumor-to-normal organ ratios of retained radioactivity following targeting of human T-NHL xenografts with 131I-BC8 (anti-CD45) and I-125-BHV-1 (control). Tumor-to-normal organ ratios of percentage injected radioiodine/g tissue of 131I-BC8 (anti-CD45, ■) and 125I-BHV-1 (control,  ) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
Tumor-to-normal organ ratios of retained radioactivity following targeting of human T-NHL xenografts with 131I-BC8 (anti-CD45) and I-125-BHV-1 (control). Tumor-to-normal organ ratios of percentage injected radioiodine/g tissue of 131I-BC8 (anti-CD45, ■) and 125I-BHV-1 (control,  ) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
) in mice with CCRF-CEM (A,B) and Karpas 299 (C,D) xenografts after 24 and 48 hours.
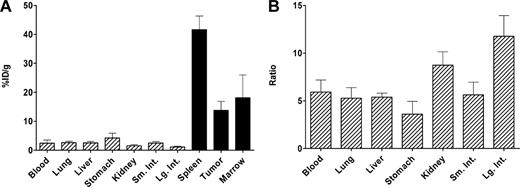
Antimurine CD45 RIT targets murine T-NHL
Because CD45 is also expressed on normal hematopoietic cells, we hypothesized that the inability of BC8 to bind mCD45 in the spleen and marrow may have favorably influenced our biodistribution results in the xenograft models. To address this question in a model that would more directly replicate the probable clinical use of this agent, namely, expression of CD45 both on T-NHL sites and normal hematolymphoid tissues, we evaluated the ability of anti-CD45 RIT to preferentially target tumor sites in a syngeneic model. Mice with palpable EL-4 (mT-NHL) xenografts were injected with 200 μg 131I-30F11 (anti-mCD45) followed by harvest of tumor sites and normal organs. Hematopoietic target sites (tumor, marrow, and spleen) retained 14% to 42% of the injected 131I dose/g tissue compared with 1.2% to 4.2% in nontarget tissues (Figure 4A) despite the broad expression of CD45 on hematolymphoid tissues. This preferential targeting by anti-CD45 RIT in a syngeneic model translated into favorable tumor-to-normal organ ratios of radioisotope retention, indicating that 3.6 to 11.8 times more radiation would be delivered to tumor sites compared with nontarget tissues at 24 hours (Figure 4B). The precise ratios of %ID/g and P values comparing target to nontarget sites are detailed in Table 1.
Biodistribution of 131I-30F11 (antimurine CD45) in a syngeneic murine T-NHL model. (A) Percentage injected 131I dose/g tissue (%ID/g) in target (■) and nontarget (▨) organs after 131I-30F11 (antimurine CD45) in an EL-4 (murine T-NHL) model. (B) The resultant tumor-to-normal organ ratios (24 hours).
Biodistribution of 131I-30F11 (antimurine CD45) in a syngeneic murine T-NHL model. (A) Percentage injected 131I dose/g tissue (%ID/g) in target (■) and nontarget (▨) organs after 131I-30F11 (antimurine CD45) in an EL-4 (murine T-NHL) model. (B) The resultant tumor-to-normal organ ratios (24 hours).
Ratios of percentage injected 131I dose/g between target (tumor, marrow, spleen) and nontarget organs after 131I-30F11 (antimurine CD45) in a EL-4 (murine T-NHL) model (24 hours)
| Nontarget organ . | Tumor/organ . | P . | Bone marrow/organ . | P . | Spleen/organ . | P . |
|---|---|---|---|---|---|---|
| Blood | 5.9 | .00050 | 9.6 | .00843 | 19.0 | .00005 |
| Lung | 5.3 | .00095 | 10.6 | .01180 | 16.1 | .00004 |
| Liver | 5.4 | .00071 | 8.8 | .01092 | 16.9 | .00005 |
| Stomach | 3.6 | .00165 | 4.9 | .02690 | 11.3 | .00006 |
| Kidney | 8.7 | .00065 | 15.6 | .00861 | 27.3 | .00004 |
| Small intestine | 5.6 | .00102 | 10.9 | .01279 | 17.2 | .00004 |
| Large intestine | 11.8 | .00070 | 21.8 | .00875 | 36.2 | .00004 |
| Nontarget organ . | Tumor/organ . | P . | Bone marrow/organ . | P . | Spleen/organ . | P . |
|---|---|---|---|---|---|---|
| Blood | 5.9 | .00050 | 9.6 | .00843 | 19.0 | .00005 |
| Lung | 5.3 | .00095 | 10.6 | .01180 | 16.1 | .00004 |
| Liver | 5.4 | .00071 | 8.8 | .01092 | 16.9 | .00005 |
| Stomach | 3.6 | .00165 | 4.9 | .02690 | 11.3 | .00006 |
| Kidney | 8.7 | .00065 | 15.6 | .00861 | 27.3 | .00004 |
| Small intestine | 5.6 | .00102 | 10.9 | .01279 | 17.2 | .00004 |
| Large intestine | 11.8 | .00070 | 21.8 | .00875 | 36.2 | .00004 |
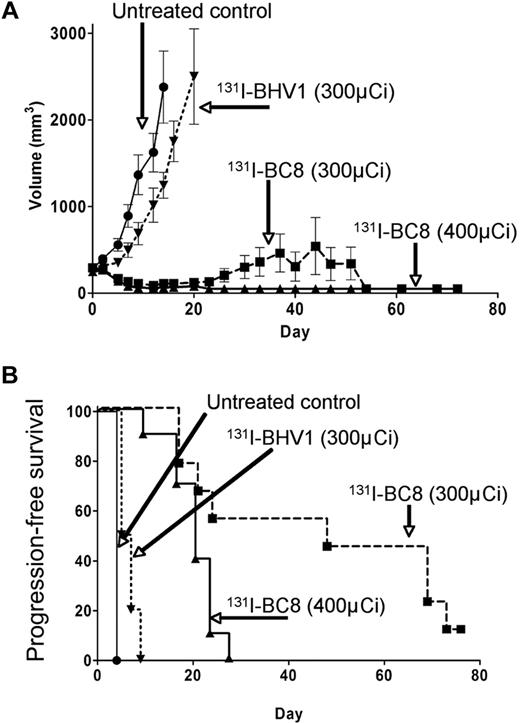
Anti-CD45 RIT controls T-NHL tumor growth and improves survival
We next sought to determine whether the biodistribution results could translate into improved tumor control and survival. Mice with palpable T-NHL xenografts (CCRF-CEM) were randomly assigned to receive 200 μg BC8 labeled with either 300 or 400 μCi 131I, 200 μg BHV-1 (control) labeled with 300 μCi 131I, or no treatment. Tumor dimensions and survival were tracked. By day 9, complete remissions (CRs) were attained in 90% of mice treated with 400 μCi of 131I-BC8 and 67% of mice that received 300 μCi 131I-BC8 (Figure 5A). In contrast, none of the untreated control mice or mice that received 300 μCi of 131I-BHV-1 achieved CR (P < .001). This improved tumor control translated into longer progression-free survival (PFS) for the BC8-treated mice versus the controls (median PFS, 23 days BC8 vs 4.5 days controls, log-rank P < .001; Figure 5B). All 20 mice in the 2 control groups required death because of tumor growth, whereas only 4 of 20 of the mice in the experimental arms needed to be killed because of disease progression and unmaintained remissions persisted for more than 72 days after therapy. A dose-response relationship was noted between the 300-μCi and 400-μCi 131I-BC8 groups, but because transplantation was not used to abrogate the expected hematologic toxicity of high doses of radioiodine, the 400-μCi 131I-BC8–treated animals experienced inferior PFS because of nonrelapse mortality from the expected pancytopenia as evidenced by petechiae, pallor, and weight loss.
Antitumor efficacy of 131I-BC8 (anti-CD45) in a human T-NHL xenograft model. Tumor volume (A) and progression-free survival (B) in mice bearing human T-NHL xenografts (CCRF-CEM) after no treatment, BHV1 labeled with 300 μCi 131I (control), BC8 labeled with 300 μCi 131I, or BC8 labeled with 400 μCi 131I.
Antitumor efficacy of 131I-BC8 (anti-CD45) in a human T-NHL xenograft model. Tumor volume (A) and progression-free survival (B) in mice bearing human T-NHL xenografts (CCRF-CEM) after no treatment, BHV1 labeled with 300 μCi 131I (control), BC8 labeled with 300 μCi 131I, or BC8 labeled with 400 μCi 131I.
Discussion
The results of this study are the first illustration of the potential efficacy of anti-CD45 RIT for the treatment of T-NHL. In this series of experiments, we initially demonstrated that CD45 was expressed in high copy number in both T-NHL cell lines and a spectrum of T-NHL patient samples. The surface density of CD45 was reliably expressed on the majority of T-NHLs at or above the concentration expected for CD20 in B-NHL, indicating that sufficient antigen should be available for successful targeting.19 Interestingly, 2 of 3 T-LBL specimens exhibited significantly lower CD45 expression, suggesting that CD45 may not be optimal for targeting precursor T-cell neoplasms.20
The subsequent murine studies confirmed that this strategy can yield higher retained activity and, thus, radiation exposure in CD45-bearing tumor sites while sparing normal nontarget tissues. It is this favorable tumor-to-normal organ ratio that provides the therapeutic index of RIT. This therapeutic index was maintained, even in the more clinically relevant and scientifically rigorous syngeneic tumor model where both CD45-bearing T-NHL sites and normal CD45-bearing hematolymphoid tissues were targeted. Despite the broad expression of CD45, tumor sites, spleen, and marrow retained 3.6 to 11.3 times the radioactivity as the highest nontarget organ at 24 hours. These ratios appeared superior to published biodistribution data when targeting CD20 in B-NHL and translated into 131I dose-related improved response rates and remission durations.6,16
Unlike with the B-NHLs, targeted therapies for T-NHLs are less broadly used. This may be in part the result of the heterogeneity of ideal antigens expressed in these diseases and the potential requirement to develop novel agents for each group of T-cell malignancies.13 The first commercially available monoclonal antibody targeting antigens found on some T-NHLs was alemtuzumab (Campath 1H). Alemtuzumab targets CD52, an antigen expressed on approximately 50% of T-NHLs, and can induce responses 6 to 12 months in duration in 36% to 55% of patients with relapsed T-NHL or MF.21-23 A second targeted agent directed against the IL-2 receptor (CD25), denileukin diftitox (Ontak), has been approved for the treatment of MF and has been shown to yield response rates of 30% lasting a median of 6.9 months.24 Further improvement on targeted therapies for T-NHL has been limited, although pilot data exist regarding the use of anti-CD30 antibodies in ALCL as well as 90Y-anti-CD25, 90Y-anti-CD5, and 131I-antiCD5 antibodies in T-cell leukemia/lymphoma.25-28 Unfortunately, to date, there are no Food and Drug Administration–approved anti–T-NHL radioimmunoconjugates. More importantly, most T-NHL RIT programs in development may be limited to a subset of T-lymphoid malignancies because of the varied antigen expression (eg, CD5, CD25, CD30) in these diseases.13,29 Thus, a pan–T-cell antigen target would be ideal to develop a successful, widely applicable RIT-based approach for T-NHL.
Our preclinical results are particularly applicable to therapy for T-NHL, where it is estimated that less than 15% of patients with more than one adverse factor at diagnosis will be alive and in remission at 5 years.3,4 Despite the poor prognosis, even the most refractory subtypes of T-NHL (angiocentric T-NHL and NK/T-NHL) remain radiation-sensitive, with local control being attainable when absorbed doses of more than or equal to 40 Gy are applied.30 Likewise, HSCT has been used to improve outcomes.31-33 Unfortunately, less than one-third of patients with relapsed, chemosensitive T-NHL will achieve long-term remission with this strategy, with the major cause of failure being recurrent disease.31-33 One could hypothesize that escalation of the radiation dose to tumor sites before HSCT by the use of anti-CD45 RIT could deliver potentially curative radiation exposure to multifocal disease beyond that which could be administered with external beam therapy. Because CD45 is also expressed on most cells of hematopoietic origin, HSCT would be required with any use of this strategy. Dual targeting of both specific tumor sites and hematolymphoid tissues, however, may also prove advantageous for the control of both measurable and minimal disease sites because the radiation exposure to individual tumor cells could be amplified via crossfire from targeting adjacent CD45-bearing tissues.
In conclusion, these results in conjunction with other preclinical and clinical data from our group indicate the potential efficacy of anti-CD45 RIT in T-NHL and support the rapid translation of this strategy to the clinic.34,35 We anticipate opening a clinical trial to test these hypotheses in patients with relapsed T-NHL in 2009.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Anju Thomas for antigen density quantification.
This work was supported by the National Institutes of Health (grants P01CA44991, R01CA76287, R01CA109663, K23CA85479, and K08CA095448), the Leukemia & Lymphoma Society (SCOR Grant 7040), the Lymphoma Research Foundation Mantle Cell Lymphoma Research Initiative, and a donation from Frank and Betty Vandermeer. A.K.G. is a Scholar in Clinical Research of the Leukemia & Lymphoma Society.
National Institutes of Health
Authorship
Contribution: A.K.G. conceived the project, designed experiments, analyzed data, and wrote and edited the manuscript; J.M.P. and O.W.P. designed experiments and edited the manuscript; J.R.F. designed experiments and analyzed data for antigen-binding studies and edited the manuscript; and S.W. designed, performed, and analyzed mouse experiments and edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ajay K. Gopal, University of Washington /Seattle Cancer Care Alliance, 825 Eastlake Ave E, G3-200, Seattle, WA 98195; e-mail: agopal@u.washington.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal