Abstract
Abstract 1013
Poster Board I-35
AKI is a common complication in pts with hematologic malignancies. However, its precise incidence, predisposing factors and the clinical outcome associated with AKI in these pts have not been studied. The RIFLE criteria (R= risk, I = injury; F= failure, L= loss of kidney function, and E = end-stage kidney disease), is a multilevel classification system for AKI. The RIFLE system was proposed with the objective to define and classify AKI and to predict mortality.
a) to study the incidence of AKI in pts with AML and HR-MDS undergoing intensive chemotherapy (IC); 2) to describe the risk factors for the development of AKI 3) to assess the RIFLE criteria to predict mortality.
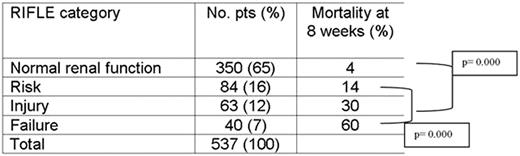
Retrospective review of pts with AML or HR-MDS who underwent IC from 1999 to 2007. Pts with chronic kidney disease (baseline serum creatinine [Cr] > 1.5 mg/dL) were excluded. Backward stepwise logistic regression was used to determine predictors of AKI, defined as at least a 50% rise in Cr from baseline during IC. Severity of AKI was further defined by the RIFLE criteria (Risk = >50% rise in Cr, Injury = >100% rise in Cr, and Failure = >200% rise in Cr or requiring dialysis). Kaplan-Meier estimates for 8-week cumulative mortality were determined for each RIFLE category.
537 pts were included. Median age was 55 yo (range 17-84), 52% were male, 88% were treated for AML, 97% had good performance status. All the pts received high-dose cytarabine (HD-AC) containing regimens (46% in combination with idarubicin; 18% with daunorubicin; 17 with fludarabine, 10% with clofarabine and 9% with cytoxan + topotecan). Fifty-two percent of the pts received vancomycin at any time from day 1 of CHEMO to the day of maximum Cr, 7% received aminoglycosides, 44% amphotericin B lipid formulation, 59% diuretics, and 8% each required vasopressors or mechanical ventilation. Mortality at 8-weeks among pts in the RIFLE category was significantly higher than in pts without AKI (p=0.000). Additionally, there was a progressive increase in 8-week cumulative mortality with worsening RIFLE class (p =0.000) (Table 1).
Univariate analysis for risk factors for AKF revealed that older age, baseline bilirubin, ICU admission, mechanical ventilation, use of vasopressors, intravenous contrast, vancomycin, aminoglycosides, amphotericin B lipid formulation, diuretics, presence of infection at start chemo, and treatment with HD-ARA C + anything other than fludarabine were associated with higher risk for AKI. The following variables remained significant in the multivariate analysis: older age (OR:1.03, p<0.01), mechanical ventilation (OR:14, p=0.001); vancomycin (OR: 2.5, p=0.001); diuretics (OR: 2.8, p<0.001); vasopressors (OR: 4.5, p=0.030); Amphotericin B lipid formulation (OR: 3.0, p<0.001); and HD-AC + others vs. HD-Ara C + Fludarabine (OR: 2.3, 0.028).
1) According to the RIFLE category, 35% of pts with AML or HR-MDS developed some degree of AK impairment during IC 2) There is a progressive increase in mortality with worsening RIFLE classification, furthermore, pts with even relatively small increases in Cr have lower survival 3) Strategies to avoid drugs that are frequently used in these pts such as diuretics, amphotericin B lipid formulation and vancomycin may potentially reduce AKI.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal