Abstract
Abstract 1200
Poster Board I-222
Chemosensitive disease, as determined by computed tomography (CT) or fluorine-18-deoxyglucose positron emission tomography (FDG-PET), is required for successful autologous hematopoietic stem cell transplant (autoHSCT) in patients with aggressive non-Hodgkin's lymphoma (NHL) and Hodgkin lymphoma (HL). However, whether chemosensitivity, as determined by FDG-PET, is a requirement for successful allogeneic hematopoietic stem cell transplantation (alloHSCT) has yet to be established. Therefore, we analyzed the survival of alloHSCT recipients transplanted at MSKCC between 2001-2007 for the treatment of relapsed or refractory NHL and HL who had both FDG-PET and CT imaging to assess response prior to alloHSCT. Our hypothesis is that FDG-PET prior to alloHSCT will add prognostic information compared to CT scan alone prior to alloHSCT.
Thirty-seven lymphoma patients had combined pre-alloHSCT imaging (10 aggressive NHL, 12 indolent NHL, and 15 HL by WHO classification). Patients were scored as either complete remission (CR), partial remission (PR) or stable disease (SD) by CT according to previously published criteria (Cheson et al. JCO 1999). For the purposes of analysis, patients with PR or SD were classified together as non-CR. FDG-PET was scored as either positive, if FDG-avid disease was measurable on corresponding imaging (CT or magnetic resonance imaging), or FDG-negative prior to alloHSCT. Patients with progression of disease prior to alloHSCT by either FDG-PET and/or CT were excluded in view of their historically poor survival following alloHSCT.
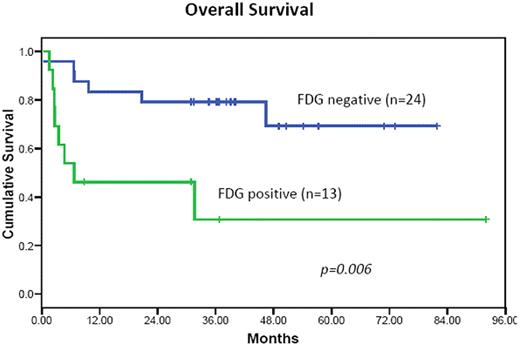
The median age was 42 years (range 18-66) with 5 patients receiving myeloablative (MA) conditioning while the remainder received non-myeloablative (NMA) conditioning. Seventeen (46%) had received prior autologous transplants. Thirteen patients were transplanted with HLA-identical related donors (1 mismatched related donor) and the remaining 23 patients from unrelated donors (12 fully HLA-matched and 11 mismatched). Twenty-four (65%) of the patients were FDG-negative and 16 (43%) were in CR by CT prior to alloHSCT. Disparity between CT and FDG-PET response was observed in 8 FDG-PET negative patients (5 SD and 3 PR by CT). With a median follow-up for survivors of 38 months (range 9-92), the Kaplan-Meier estimates of overall (OS) and progression free survival (PFS) at 3 years post-alloHSCT were 64% and 56%, respectively. There was no significant difference in survival according to age < or ≥ 40 years, prior autoHSCT, conditioning intensity (MA or NMA) or WHO classification. FDG-negative patients had significant OS (Figure) and PFS improvement compared to FDG-positive patients (p=0.006 and p=0.02, respectively). Patients in CR had improved OS compared to those in PR/SD by CT imaging (p=0.02), however improvement in PFS was not significant (p=0.13). Patients that were FDG-PET negative and CT CR (n=16) had 88% OS at 3 years compared to 63% in the 8 patients that were FDG-PET negative and CT non-CR, although this difference was not significant (p=0.22).
Response to therapy prior to alloHSCT as determined by FDG-PET offers critical prognostic information beyond traditional cross-sectional CT imaging considering the significant improvement in both OS and PFS. These data suggests that the goal of therapy prior to alloHSCT should be to normalize FDG-PET independent of tumor bulk. Prospective investigation is warranted to validate this conclusion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal