Abstract
Adoptive transfer of autologous Epstein-Barr virus–specific cytotoxic T lymphocytes (EBV-CTLs) to solid organ transplant (SOT) recipients has been shown safe and effective for the treatment of EBV-associated posttransplantation lymphoproliferative disorders (PTLDs). SOT recipients, however, require the continuous administration of immunosuppressive drugs to prevent graft rejection, and these agents may significantly limit the long-term persistence of transferred EBV-CTLs, precluding their use as prophylaxis. Tacrolimus (FK506) is one of the most widely used immunosuppressive agents in SOT recipients, and its immunosuppressive effects are largely dependent on its interaction with the 12-kDa FK506-binding protein (FKBP12). We have knocked down the expression of FKBP12 in EBV-CTLs using a specific small interfering RNA (siRNA) stably expressed from a retroviral vector and found that FKBP12-silenced EBV-CTLs are FK506 resistant. These cells continue to expand in the presence of the drug without measurable impairment of their antigen specificity or cytotoxic activity. We confirmed their FK506 resistance and anti-PTLD activity in vivo using a xenogenic mouse model, suggesting that the proposed strategy may be of value to enhance EBV-specific immune surveillance in patients at high risk of PTLD after transplantation.
Introduction
Adoptive transfer of Epstein-Barr virus–specific cytotoxic T lymphocytes (EBV-CTLs) can induce the regression of EBV-associated posttransplantation lymphoproliferative diseases (EBV-PTLDs) in recipients of allogeneic hematopoietic stem cell (HSC) grafts.1,2 Moreover, prophylactic administration of EBV-CTLs can efficiently prevent the occurrence of EBV-PTLDs in these patients due to the long-term in vivo persistence of these cells after adoptive transfer.1,2
Although EBV-CTLs can also be effective to treat PTLDs occurring after solid organ transplantation,3-9 it has proven difficult to obtain reduction in morbidity in these patients using a prophylactic approach.10 Indeed, in contrast to allogeneic HSC transplantation, solid organ transplant (SOT) recipients require continued administration of immunosuppressive drugs to avoid graft rejection,11,12 and these agents may significantly impair the growth, expansion, and long-term persistence of adoptively transferred EBV-CTLs.13
Although this inhibition evidently does not preclude the short-term in vivo cytotoxic activity of adoptively transferred EBV-CTLs and hence benefit in the case of established disease,3-9 it effectively precludes their cost-effective use as prophylactic treatment for patients at high risk for PTLD development after solid organ transplantation. To overcome this obstacle and improve CTL proliferation and persistence despite continued immunosuppression, we have made EBV-CTLs resistant to the effects of tacrolimus (FK506), a commonly used immunosuppressive drug.
FK506 is widely used as an immunosuppressive drug to prevent rejection of renal, liver, and heart-lung transplant grafts.14-17 FK506 inhibits host immune responses by binding to immunophilin FK506-binding proteins (FKBPs).18 Of the 10 known mammalian FKBPs, the 12-kDa FK506-binding protein (FKBP12) appears to play a key role in mediating FK506 immunosuppression,19 forming a complex with the drug that inhibits the Ca2+-activated serine/threonine phosphatase calcineurin, and thereby preventing cytoplasmic nuclear factor of activated T cell (NFATc) dephosphorylation, which is required for interleukin-2 (IL-2) production and T-cell activation.20,21
We hypothesized that EBV-CTLs in which we prevented binding of FK506 to FKBP12 would retain their ability to proliferate even in the presence of the drug. To achieve this effect we selectively down modulated FKBP12 in EBV-CTLs using a specific small interference RNA (siRNA) expressed by a retroviral vector. We show that stable knockdown of FKBP12 in EBV-CTLs allows them to expand in the presence of therapeutic doses of FK506 without affecting their ex vivo or in vivo antigen specificity and function.
Methods
Plasmid construction and retrovirus production
We obtained the full-length human FKBP12 cDNA, by reverse-transcription polymerase chain reaction from peripheral blood mononuclear cells (PBMCs) and cloned it into the expression plasmid p.eGFP-C1 (Clontech Laboratories Inc) to generate the p-eGFP-hFKBP12-C1 plasmid. In this plasmid, FKBP12 was cloned in frame to the COOH-terminus of enhanced green fluorescent protein (eGFP) to obtain a fusion protein. We designed siRNA sequences targeting the FKBP12 mRNA using software from Ambion (http://www.ambion.com) and cloned them into the pSUPER vector (OligoEngine), containing the puromycin resistance gene, or pSUPER.eGFP vector, containing GFP as a selectable marker, as previously described.22 Control vectors encoding an irrelevant siRNA were also used.22,23 The vector encoding firefly luciferase (FFLuc) was constructed and used as previously described.24 We prepared the retroviral supernatant using 293T cells cotransfected with 3 plasmids (the retroviral construct, Peg-Pam-e encoding gag-pol, and RDF encoding the RD114 envelop25 ) using the Gene Juice transfection reagent (Novagen Brand). Supernatants were collected 48 and 72 hours later.
Screening of FKBP12-siRNAs
We cloned 17 different siRNAs that targeted FKBP12 mRNA into the pSUPER retroviral vector. To evaluate the silencing activity of these siRNAs, we cotransfected 293T cells with the reporter plasmid (p-eGFP-hFKBP12-C1) and pSUPER vectors encoding siRNAs (ratio of 1:2). Silencing mediated by the siRNAs was measured by quantifying the expression of GFP in 293T cells using a BD FACSCalibur Flow Cytometer (BD Biosciences) 48 hours after plasmid transfection.
Western blot analysis
Cell lysates were resolved on sodium dodecyl sulfate–polyacrylamide gel electrophoresis. FKBP12 was detected using a rabbit polyclonal antibody (AbCAM Inc). Immunoblots were developed using enhanced chemiluminescence detection reagents (Amersham Biosciences). To evaluate the equal loading of the proteins, membranes were reprobed with glyceraldehyde-3-phosphate dehydrogenase (GAPDH) monoclonal antibody (mAb; Santa Cruz Biotechnology). To measure the relative intensity of bands, after drawing appropriate regions of interest around the bands, we used the Kodak Molecular Imaging Software Version 4.0.
Generation and transduction of effector T cells
Human PBMCs were activated in 24-well plates coated with OKT3 (Ortho Biotech) and CD28 (Pharmingen) mAbs in the presence of recombinant human IL-2 (100 U/mL; Proleukin; Chiron). Activated T cells were transduced on day 3 in 24-well plates precoated with recombinant fibronectin fragment (FN CH-296; Retronectin; Takara Shuzo) using specific retroviral supernatant and IL-2, as previously described.24,26 T cells were then collected and expanded in T-cell medium (50% RPMI, 50% Click media [Irvine Scientific], 10% fetal bovine serum, and 2 mM l-glutamine) using IL-2 (50-100 U/mL) to obtain sufficient cells for in vitro experiments.
Generation and retroviral transduction of EBV-CTLs
EBV-CTLs were prepared by stimulating PBMCs with γ-irradiated (40 Gy) autologous EBV-transformed lymphoblastoid cell lines (EBV-LCLs) as previously described.2,7,13 Stimulations with autologous EBV-LCLs were repeated weekly and IL-2 (50 U/mL) was added twice a week from day 14 of culture.7 After the third stimulation, EBV-CTLs were transduced in Retronectin-precoated 24-well plates with the retroviral supernatant.27 Three days after transduction, EBV-CTLs were collected and then stimulated weekly with autologous EBV-LCLs in the presence of low doses of IL-2 (20 U/mL) with or without the addition of FK506 (5 or 10 ng/mL; LC Laboratories), or with or without the addition of temsirolimus (25 ng/mL; LC Laboratories).
Immunophenotyping
Phycoerythrin-, fluorescein isothiocyanate–, peridinin chlorophyll protein–, and allophycocyanin–conjugated CD3, CD4, CD8, CD56, CD19, and αβ T-cell receptor (TCR) mAbs (Becton Dickinson) were used to stain EBV-CTLs and T cells. Control samples labeled with an appropriate isotype-matched Ab were included in each experiment. We analyzed cells using a FACSCalibur with a filter set for 4 fluorescence signals and CellQuest software (BD Biosciences). For each sample, we analyzed a minimum of 10 000 events.
Multimers
The antigen specificity of EBV-CTLs was evaluated with EBV-specific multimers, as previously described.7 We chose multimers based on available donor human leukocyte antigen (HLA) types, which recognized the following EBV peptides: EBNA3B, HLA-A11: IVTDFSVIK, and EBNA3B, HLA-A11: AVFDRKSDAK; EBNA3A, HLA-B8: QAKWRLQTL; BZLF1, HLA-B8: RAKFKQLL (listed in Khanna and Burrows28 ; Houssaint et al29 ). Multimers were prepared by Proimmune. Samples were costained with CD8-allophycocyanin and CD3–peridinin chlorophyll protein mAbs. Isotype controls were included. For each sample, a minimum of 100 000 cells were analyzed using a FACSCalibur with a filter set for 4 fluorescence signals and CellQuest software.
Phosphorylation of S6K1
After transduction, T cells were stimulated overnight with bound-OKT3 mAb (1 μg/mL) in the presence of increasing concentration of temsirolimus (from 1 to 25 ng/mL). Cells were then collected, washed, fixed, permeabilized with methanol, and then stained with phospho-S6 ribosomal protein (Ser235/236) rabbit mAb Alexa Fluor 647 conjugate (Cell Signaling Technology). Control samples labeled with an appropriate isotype-matched Ab were included. Cells were then analyzed using a FACSCalibur and CellQuest software. For each sample, we analyzed a minimum of 10 000 events.
Enzyme-linked immunospot assay
The interferon-γ (IFNγ) enzyme-linked immunospot (ELIspot) assay (Mabtech, Inc) was performed as previously described.7 Briefly, EBV-CTLs were plated in triplicate at 105 in the presence of the appropriate peptides (5 μM). Negative controls included EBV-CTLs alone and EBV-CTLs plated with irrelevant peptides. As positive controls, EBV-CTLs were stimulated with autologous EBV-LCLs.
Chromium release assay
The cytotoxic activity of EBV-CTLs was evaluated in a standard 4-hour 51Cr release assay, as previously described.7 Target cells included autologous and HLA class I and II mismatched EBV-LCLs, and the K562 cell line (as a natural killer cell target). Target cells incubated in media alone or in 1% Triton X-100 (Sigma-Aldrich) were used to determine spontaneous and maximum 51Cr release, respectively. The mean percentage specific lysis of triplicate wells was calculated as follows: 100 × (test counts − spontaneous counts)/(maximum counts − spontaneous counts).
Proliferation assay
EBV-CTLs were plated in triplicate at 105 cells/well with γ-irradiated (40 Gy) autologous EBV-LCLs at an effector-target ratio of 4:1 in the presence of IL-2 (20 U/mL), with or without increasing doses of FK506 (from 5 ng/mL to 100 ng/mL). Transduced T cells were stimulated with bound-OKT3 mAb (1 μg/mL) in the presence of increasing concentrations of temsirolimus (from 5 ng/mL to 25 ng/mL). After 72 hours, CTLs or T cells were pulsed with 1 μCi (0.037 MBq) methyl-3[H]thymidine (Amersham Pharmacia Biotech), cultured for an additional 16 hours, and then harvested onto filters and dried. Thymidine uptake was measured as counts per minute in a β-scintillation counter (liquid scintillation analyzer TRI-CARB 2910 TR; Perkin Elmer). The percentage suppression was calculated using the following formula: 100 × [1 − (experimental cpm − control cpm)/(without drug cpm − negative control cpm)], as previously reported.13
Transduction of tumor cells with the luciferase vector
EBV-LCLs were transduced with the FFLuc vector on a Retronectin-coated plate and then selected using puromycin (Sigma-Aldrich) as previously described.30 To confirm transgene expression, 5 × 106 tumor cells were lysed and aliquots diluted in 100 μL of d-luciferin according to the manufacturer's instructions (Promega). Bioluminescence was measured using a luminometer (Monolight; BD Biosciences).
In vivo experiments
All mouse experiments were performed in accordance with Baylor College of Medicine Animal Husbandry and Institutional Animal Care and Use Committee guidelines and were approved by the Baylor College of Medicine's institutional review board.
Antitumor activity
To assess persistence and antitumor activity of control and genetically modified human EBV-CTLs in the presence of FK506 in vivo, we used a xenograft lymphoma severe combined immunodeficient (SCID) mouse model and the IVIS imaging system (Xenogen; Caliper Life Sciences) as previously described.27,30 Six- to 8-week-old CB17/SCID mice (Harlan-Sprague) were sublethally irradiated (230 cGy) and engrafted intraperitoneally with 3 × 106 FFLuc+ EBV-LCLs resuspended in Matrigel (BD Biosciences).30 Three or 4 days after engraftment (when the light emission of the tumor was consistently measurable) and again 1 week later, mice received 10 × 106 autologous EBV-CTLs intraperitoneally. In addition, mice also received 3 times a week intraperitoneal injections of 1000 U/mouse IL-2 (Teceleukin; Fisher Bioservices) and 10 mg/kg body weight of FK506.31 Control animals received only IL-2. Tumor growth was evaluated over time using the IVIS imaging system. Briefly, a constant region of interest was drawn over the tumor regions and the intensity of the signal measured as total photon/sec/cm2/steradian (p/s/cm2/sr) as previously described.27,30
Statistical analysis
All in vitro experiments were summarized as mean plus or minus SD. Student t test was used to determine the statistical significant differences between samples, with P value less than .05 indicating a significant difference. Survival was evaluated by Kaplan-Meier analysis (SPSS software) and the statistical significance of observed differences assessed by log-rank and Breslow testing.
Results
Selection of siRNAs targeting the human FKBP12 mRNA
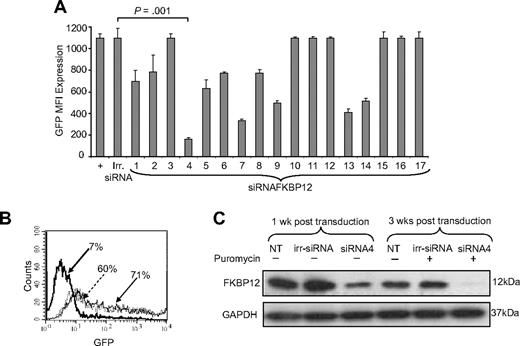
To rapidly select functional siRNAs, the 17 predicted siRNA sequences targeting the human FKBP12 mRNA were cloned in the pSUPER vector.22 FKBP12-siRNA-pSUPER or control siRNA-pSUPER (irr-siRNA) vectors were then cotransfected into 293T cells with the reporter plasmid eGFP-hFKBP12 (encoding the fusion protein eGFP-hFKBP12). GFP expression, measured by fluorescence-activated cell sorting (FACS) analysis 48 hours after transfection, was used as a surrogate marker of FKBP12 mRNA silencing by specific siRNAs. As shown in Figure 1A, the GFP mean fluorescence intensity (MFI) of eGFP-hFKBP12+ 293T cells was 1067 (± 80) and remained stable in 293T cells cotransfected with the irr-siRNA (1097 ± 89). Variable decreases of the GFP MFI were observed in 293T cells after transfecting each FKBP12-siRNA-pSUPER vector. The siRNA designated siRNA4, which targets the GATGGAAAGAAATTTGATT mRNA sequence, significantly knocked down the GFP MFI to 163 (± 33), which is equivalent to a more than 85% reduction in the FKBP12 expression compared with irr-siRNA (P = .001; Figure 1A-B). The combination of siRNA4 with other siRNAs had no further effect on GFP expression or MFI (data not shown). Hence, siRNA4 was selected for all subsequent experiments.
Identification of a siRNA vector that stably knocks down FKBP12. (A) GFP MFI of 293T cells transfected with eGFP-hFKBP12 (+) or cotransfected with eGFP-hFKBP12 and each of the 17 predicted siRNA sequences targeting the human FKBP12 mRNA or an irrelevant siRNA (irr-siRNA). siRNA4 resulted in > 85% reduction of the GFP MFI. (B) GFP was expressed by 60% of 293T cells transfected with the reporter plasmid eGFP-hFKBP12 alone, by 71% of 293T cells cotransfected with the irr-siRNA plasmid, and by 7% of 293T cells cotransfected with siRNA4 plasmid. (C) The expression of the FKBP12 in nontransduced (NT), irr-siRNA+, and siRNA4+ EBV-CTLs assessed by WB 1 week after transduction and after selection with puromycin for 3 weeks. FKBP12 expression is visibly reduced in siRNA4+ EBV-CTLs after transduction. This effect is more evident after selection in the presence of puromycin. The bottom gel shows the membrane reprobed with anti-GAPDH antibody.
Identification of a siRNA vector that stably knocks down FKBP12. (A) GFP MFI of 293T cells transfected with eGFP-hFKBP12 (+) or cotransfected with eGFP-hFKBP12 and each of the 17 predicted siRNA sequences targeting the human FKBP12 mRNA or an irrelevant siRNA (irr-siRNA). siRNA4 resulted in > 85% reduction of the GFP MFI. (B) GFP was expressed by 60% of 293T cells transfected with the reporter plasmid eGFP-hFKBP12 alone, by 71% of 293T cells cotransfected with the irr-siRNA plasmid, and by 7% of 293T cells cotransfected with siRNA4 plasmid. (C) The expression of the FKBP12 in nontransduced (NT), irr-siRNA+, and siRNA4+ EBV-CTLs assessed by WB 1 week after transduction and after selection with puromycin for 3 weeks. FKBP12 expression is visibly reduced in siRNA4+ EBV-CTLs after transduction. This effect is more evident after selection in the presence of puromycin. The bottom gel shows the membrane reprobed with anti-GAPDH antibody.
siRNA4 significantly knocked down expression of endogenous FKBP12 in EBV-CTLs
We measured the effects of siRNA4 on the expression of endogenous FKBP12 in EBV-CTL lines generated from 6 EBV-seropositive donors. These CTLs were transduced after the third antigen stimulation either with the retroviral vector pSUPER encoding the siRNA4 or with the control irr-siRNA vector. After transduction, CTLs were maintained in culture and selected with puromycin (0.1-0.5 μg/mL). As shown in Figure 1C, FKBP12 expression, assessed by Western blot (WB) analysis, was reduced by 42% in EBV-CTLs transduced with siRNA4, but not in CTLs expressing the irr-siRNA. This effect was further increased when CTLs were selected in the presence of puromycin because we observed a 94% reduction of FKBP12 in siRNA4+ EBV-CTLs (Figure 1C). FKBP12 knockdown was stable in EBV-CTLs maintained in culture for more than 2 months (data not shown).
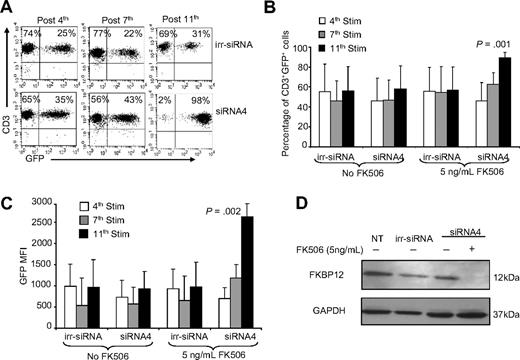
Enrichment of FKBP12-silenced EBV-CTLs in the presence of FK506
We next measured the effects of reduced FKBP12 expression on the resistance of EBV-CTLs to FK506. We transduced EBV-CTLs with either pSUPER.eGFP encoding siRNA4 or pSUPER.eGFP encoding control siRNA and determined transduction efficiency by measuring GFP expression using FACS analysis. Transduction efficiency was 46% (± 22%) for siRNA4+ CTLs and 56% (± 27%) for irr-siRNA+ CTLs. After transduction, EBV-CTLs were maintained in culture by weekly stimulation with irradiated autologous EBV-LCLs and suboptimal doses of IL-2 (20 U/mL added twice a week) because ex vivo cultured EBV-CTLs become highly dependent on IL-2 for their proliferation and no expansion is observed in the absence of exogenous cytokines (data not shown and Quintarelli et al32 ), with or without the addition of FK506 (5 ng/mL added twice a week) starting 1 week after transduction (fourth stimulation). We determined whether CTL lines were selected/enriched over time in FK506-resistant cells by monitoring changes in the percentage of GFP+ cells. As shown in Figure 2A and B, the percentage of GFP+ CTLs significantly increased over the following 7 weeks of culture for siRNA4+ EBV-CTLs cultured in the presence of FK506 (from 46% ± 22% at the fourth stimulation to 89% ± 5% at the 11th stimulation; P = .001). In contrast, the percentage of GFP+ CTLs remained stable for irr-siRNA+ EBV-CTLs cultured in the presence of FK506 (from 56% ± 27% at the 4th stimulation to 57% ± 23% at the 11th stimulation; P = not significant). In parallel with the increasing percentages of GFP+ cells, the GFP MFI significantly increased in siRNA4+ EBV-CTLs (from 692 ± 263 to 2625 ± 318; P = .002) when these cells were maintained in culture in the presence of FK506 (Figure 2C). These data show a selective enrichment of FKBP12-silenced EBV-CTLs, which suggests they had indeed become FK506 resistant. As expected, the percentage of GFP+ cells did not increase when siRNA4+ EBV-CTLs were cultured without FK506, confirming the lack of any intrinsic selective growth advantage for CTLs in which FKB12 was down-regulated (Figure 2B-C). The selection of siRNA4+ EBV-CTLs was also maintained when a higher dose of FK506 (10 ng/mL) was added to the culture (supplemental Figure 1, available on the Blood website; see the Supplemental Materials link at the top of the online article).
Selection of EBV-CTLs with a silenced FKBP12 occurs in the presence of FK506. EBV-CTLs were transduced with either the pSUPER.eGFP vector encoding the irrelevant siRNA (irr-siRNA) or pSUPER.eGFP encoding siRNA4. (A) GFP expression (as measure of transduction) of irr-siRNA+ (top plots) and siRNA4+ (bottom plots) EBV-CTLs stimulated with irradiated EBV-LCLs in the presence of IL-2 (20 U/mL) and FK506 (5 ng/mL) in a representative donor. The plots show a progressive increase of GFP+ cells for siRNA4+ CTLs, whereas the percentage of GFP+ cells is stable for irr-siRNA+ CTLs. (B) The data for the percentage of GFP+ cells for 6 CTL lines. Bars represent mean ± SD. Shown is the percentage of GFP+ cells after the 4th, 7th, and 11th stimulations, which significantly increased over time only for siRNA4+ EBV-CTLs, whereas it remained stable for irr-siRNA+ EBV-CTLs. (C) The MFI of GFP+ cells significantly increased in siRNA4+ EBV-CTLs compared with irr-siRNA+ cells when cells were maintained in culture in the presence of FK506. Bars represent mean ± SD for 6 CTL lines. (D) The expression of FKBP12 in NT and irr-siRNA+ EBV-CTLs and in siRNA4+ EBV-CTLs after 5 weeks in culture in the absence or in the presence of FK506, as assessed by WB. FKBP12 is completely undetectable by WB in siRNA4+ EBV-CTLs cultured in the presence of FK506.
Selection of EBV-CTLs with a silenced FKBP12 occurs in the presence of FK506. EBV-CTLs were transduced with either the pSUPER.eGFP vector encoding the irrelevant siRNA (irr-siRNA) or pSUPER.eGFP encoding siRNA4. (A) GFP expression (as measure of transduction) of irr-siRNA+ (top plots) and siRNA4+ (bottom plots) EBV-CTLs stimulated with irradiated EBV-LCLs in the presence of IL-2 (20 U/mL) and FK506 (5 ng/mL) in a representative donor. The plots show a progressive increase of GFP+ cells for siRNA4+ CTLs, whereas the percentage of GFP+ cells is stable for irr-siRNA+ CTLs. (B) The data for the percentage of GFP+ cells for 6 CTL lines. Bars represent mean ± SD. Shown is the percentage of GFP+ cells after the 4th, 7th, and 11th stimulations, which significantly increased over time only for siRNA4+ EBV-CTLs, whereas it remained stable for irr-siRNA+ EBV-CTLs. (C) The MFI of GFP+ cells significantly increased in siRNA4+ EBV-CTLs compared with irr-siRNA+ cells when cells were maintained in culture in the presence of FK506. Bars represent mean ± SD for 6 CTL lines. (D) The expression of FKBP12 in NT and irr-siRNA+ EBV-CTLs and in siRNA4+ EBV-CTLs after 5 weeks in culture in the absence or in the presence of FK506, as assessed by WB. FKBP12 is completely undetectable by WB in siRNA4+ EBV-CTLs cultured in the presence of FK506.
Finally, we confirmed that the positive selection of siRNA4+ EBV-CTLs in the presence of FK506 corresponded to an enrichment of EBV-CTLs with a significant down-regulation of FKBP12. As shown in Figure 2D, FKBP12 was detectable by WB in nontransduced (NT) EBV-CTLs and in those transduced with irr-siRNA cultured without FK506. In contrast, FKBP12 was completely undetectable in EBV-CTLs transduced with siRNA4 and maintained in culture for 5 weeks with antigen stimulation and in the presence of FK506 (Figure 2D). We have further supported the significance of this finding by exploring the NFAT pathway, which was partially preserved only in T cells expressing siRNA4 when stimulated in the presence of FK506 (supplemental Figure 1D).
siRNA4+ EBV-CTLs retain antigen-specific expansion in the presence of FK506
To discover whether enrichment of CTLs with knocked-down FKBP12 observed in the previous experiments was determined by a preserved proliferation of siRNA4+ EBV-CTLs in the presence of FK506, we measured EBV-CTL proliferation and numeric increase after antigen stimulation by a thymidine uptake assay and counting viable cells using trypan blue exclusion, respectively. Figure 3A shows the thymidine uptake of EBV-CTLs expressing either irr-siRNA or siRNA4 and cultured in the presence of increasing concentration of FK506. We observed that concentrations of FK506 as low as 5 ng/mL significantly reduced the proliferative capacity of NT and irr-siRNA+ EBV-CTLs. In contrast, siRNA4+ CTLs retained most of their proliferative capacity when FK506 was added, irrespective of the dose. Figure 3B shows data for 6 EBV-CTL lines cultured in the presence of 5 ng/mL FK506. Proliferation of both control NT and irr-siRNA+ EBV-CTLs (3.2 × 104 ± 0.7 × 104 cpm and 3.6 × 104 ± 1.4 × 104 cpm, respectively) was significantly reduced in the presence of 5 ng/mL FK506 (0.9 × 104 ± 0.5 × 104 cpm and 1.5 × 104 ± 0.9 × 104 cpm, respectively; P = .003), which translates to 70% (± 14%) inhibition for NT EBV-CTLs and 60% (± 20%) inhibition for irr-siRNA+ EBV-CTLs. By contrast, proliferation of siRNA4+ EBV-CTLs in the presence of FK506 was substantially preserved. Thymidine incorporation in presence of FK506 was 3.3 × 104 (± 1.3 × 104) cpm, which was only slightly reduced from that of siRNA4+ EBV-CTLs cultured in the absence of FK506 (4.4 × 104 ± 1.5 × 104 cpm; P = .06). Indeed, the percentage of inhibition of siRNA4+ EBV-CTLs was 29% (± 7%) inthe presence of FK506 (Figure 3B). This maintenance of thymidine uptake was significantly greater than that observed in NT or irr-siRNA+ EBV-CTLs cultured in the presence of FK506 (P < .01).
siRNA4+ EBV-CTLs retain proliferative activity in the presence of FK506. (A) The thymidine uptake of NT, irr-siRNA+, and siRNA4+ EBV-CTLs after stimulation with autologous EBV-LCLs in the presence of increasing concentration of FK506. In the presence of FK506, proliferation of both NT and irr-siRNA+ EBV-CTLs is significantly reduced compared with siRNA4+ EBV-CTLs. (B) The percentage inhibition for NT, irr-siRNA+, and siRNA4+ EBV-CTLs grown in the presence of FK506. Bars represent mean ± SD of 4 CTL lines. (C) The expansion in cell numbers of NT, irr-siRNA+, and siRNA4+ EBV-CTLs stimulated weekly with EBV-LCLs and IL-2 (20 U/mL) with or without the addition of FK506 (5 ng/mL). T-cell numbers increased for all CTLs in the absence of FK506, but in the presence of FK506 increased only for siRNA4+ CTLs. Shown are median ± SEM for 6 CTL lines.
siRNA4+ EBV-CTLs retain proliferative activity in the presence of FK506. (A) The thymidine uptake of NT, irr-siRNA+, and siRNA4+ EBV-CTLs after stimulation with autologous EBV-LCLs in the presence of increasing concentration of FK506. In the presence of FK506, proliferation of both NT and irr-siRNA+ EBV-CTLs is significantly reduced compared with siRNA4+ EBV-CTLs. (B) The percentage inhibition for NT, irr-siRNA+, and siRNA4+ EBV-CTLs grown in the presence of FK506. Bars represent mean ± SD of 4 CTL lines. (C) The expansion in cell numbers of NT, irr-siRNA+, and siRNA4+ EBV-CTLs stimulated weekly with EBV-LCLs and IL-2 (20 U/mL) with or without the addition of FK506 (5 ng/mL). T-cell numbers increased for all CTLs in the absence of FK506, but in the presence of FK506 increased only for siRNA4+ CTLs. Shown are median ± SEM for 6 CTL lines.
When control EBV-CTLs and siRNA4+ EBV-CTLs were maintained in culture for more than 7 weeks using weekly stimulation with EBV-LCLs, suboptimal doses of IL-2 (20 U/mL twice a week), with or without the addition of FK506 (5 ng/mL twice a week), only EBV-CTLs expressing siRNA4 numerically expanded in the presence of FK506 (median fold increase, 24; range, 3-70; Figure 3C). By contrast, the expansion of NT and irr-siRNA+ EBV-CTLs was almost completely inhibited in the presence of FK506 (median fold expansion, 1; range 0-2; Figure 3C). Similar results were obtained when a dose of 10 ng/mL FK506 was added to the culture (supplemental Figure 2).
Silencing of FKBP12 does not affect EBV-CTL functionality
We evaluated the immunophenotype, cytotoxic activity, and EBV-antigen specificity of FKBP12-silenced EBV-CTLs using FACS analysis, 51Cr release assay, and multimers and IFNγ ELIspot assay, respectively. As shown in Figure 4A, NT and irr-siRNA+ EBV-CTLs were predominantly CD3+CD8+ T lymphocytes (88% ± 8% and 87% ± 6%, respectively). The majority of CTLs expressed the αβTCR (90% ± 1% and 88% ± 11%), with less than 2% of natural killer cells (CD3−CD56+). Selective expansion of siRNA4+ EBV-CTLs in the presence of FK506 did not alter their phenotype (CD3+CD8+ = 83% ± 12%; αβTCR+ = 82% ± 14%;and CD3−CD56+ = 0.3% ± 0.2%; Figure 4A). We evaluated the cytotoxic activity of EBV-CTLs using a standard 4-hour 51Cr release assay. As shown in Figure 4B, EBV-CTLs expressing siRNA4 and cultured for 4 weeks in the presence of FK506 still retained major histocompatibility complex–restricted cytotoxic activity against EBV+ targets (66% ± 22% lysis of autologous EBV-LCLs and 16% ± 12% of allogeneic EBV-LCLs, at a 20:1 E/T ratio). This was similar to irr-siRNA+ EBV-CTLs (61% ± 12% lysis of autologous EBV-LCLs and 15% ± 10% of allogeneic EBV-LCLs, at a 20:1 E/T ratio). As expected, addition of FK506 during the 4-hour incubation did not impair CTL cytotoxic activity (data not shown).13 To ensure that EBV-CTLs retained the broad EBV-specific reactivity necessary for effective control of EBV-PTLDs, we analyzed the specificities of 4 CTL lines with informative HLA typing, using their binding of EBV-specific HLA multimers and their IFNγ production in response to EBV-derived peptides in an ELIspot assay. Figure 4C shows a representative donor in whom siRNA4+ EBV-CTLs grown in the presence of FK506 for 3 weeks maintained the same frequency of T cells recognizing EBV-associated antigen. EBV-specific T cells were also functional as they specifically released IFNγ in response to EBV-derived peptides (Figure 4D). In all 4 CTL lines, the broad repertoire of the EBV-CTLs was retained with detection of specific IFNγ production against lytic and latent EBV-associated proteins (Table 1).
siRNA4+ EBV-CTLs retain their immunophenotype, cytotoxic activity, and EBV-antigen specificity. (A) The immunophenotype of NT and irr-siRNA+ EBV-CTLs and of siRNA4+ EBV-CTLs cultured in the presence of FK506. Means ± SD are shown for the 6 CTL lines. No significant phenotypic differences were observed for siRNA4+ CTLs expanded in the presence of FK506. (B) The results of a standard 51Cr release assay of NT and irr-siRNA+ EBV-CTLs and of irr-siRNA+ and siRNA4+ EBV-CTLs cultured in the presence of FK506. Targets were K562, autologous LCLs, and allogeneic LCLs. Shown is the CTL/tumor cell ratio of 20:1. Bars represent the mean ± SD of the EBV-CTLs generated from 6 donors. No significant differences in cytotoxic activity were observed for siRNA4+ CTLs versus NT or irr-siRNA+ CTLs. (C) The frequencies of multimers recognizing latent EBV-associated antigens (EBNA3B-AVF and EBNA3B-IVT) in NT (left plots) and irr-siRNA+ (middle plots) EBV-CTLs and in siRNA4+ (right plots) EBV-CTLs cultured in the presence of FK506 for 3 weeks in 1 representative donor. (D) The frequency of CTLs responding to the indicated EBV-specific peptides assessed by IFNγ ELIspot assay in another representative donor.
siRNA4+ EBV-CTLs retain their immunophenotype, cytotoxic activity, and EBV-antigen specificity. (A) The immunophenotype of NT and irr-siRNA+ EBV-CTLs and of siRNA4+ EBV-CTLs cultured in the presence of FK506. Means ± SD are shown for the 6 CTL lines. No significant phenotypic differences were observed for siRNA4+ CTLs expanded in the presence of FK506. (B) The results of a standard 51Cr release assay of NT and irr-siRNA+ EBV-CTLs and of irr-siRNA+ and siRNA4+ EBV-CTLs cultured in the presence of FK506. Targets were K562, autologous LCLs, and allogeneic LCLs. Shown is the CTL/tumor cell ratio of 20:1. Bars represent the mean ± SD of the EBV-CTLs generated from 6 donors. No significant differences in cytotoxic activity were observed for siRNA4+ CTLs versus NT or irr-siRNA+ CTLs. (C) The frequencies of multimers recognizing latent EBV-associated antigens (EBNA3B-AVF and EBNA3B-IVT) in NT (left plots) and irr-siRNA+ (middle plots) EBV-CTLs and in siRNA4+ (right plots) EBV-CTLs cultured in the presence of FK506 for 3 weeks in 1 representative donor. (D) The frequency of CTLs responding to the indicated EBV-specific peptides assessed by IFNγ ELIspot assay in another representative donor.
Analysis of EBV specificity within the healthy donor CTL lines
| Peptide . | Lytic . | EBNA1 . | EBNA3 . | Irrelevant . |
|---|---|---|---|---|
| Donor 1 | ||||
| NT CTLs | 243 ± 47 | 1202 ± 154 | 257 ± 47 | 0 ± 0 |
| irr-siRNA+ CTLs | 242 ± 4 | ND | 109 ± 4 | 1 ± 1.7 |
| siRNA4+ CTLs + FK506 | 319 ± 61 | 1050 ± 77 | 248 ± 61 | 1.7 ± 2.1 |
| Donor 2 | ||||
| NT CTLs | 12 ± 1.5 | ND | 143 ± 23 | 0 ± 0 |
| irr-siRNA+ CTLs | 14 ± 3.1 | ND | 224 ± 16 | 0.3 ± 0.6 |
| siRNA4+ CTLs + FK506 | 5 ± 1.2 | ND | 230 ± 16 | 0.7 ± 0.6 |
| Donor 3 | ||||
| NT CTLs | 111 ± 10 | ND | 0 ± 0 | 1.3 ± 1.5 |
| irr-siRNA+ CTLs | 41 ± 10 | ND | 0 ± 0 | 0.7 ± 0.6 |
| siRNA4+ CTLs + FK506 | 64 ± 15 | ND | 0 ± 0 | 2 ± 1 |
| Donor 4 | ||||
| NT CTLs | ND | ND | 701.3 ± 89.5 | 0 ± 0 |
| irr-siRNA+ CTLs | ND | ND | 356 ± 48.1 | 0 ± 0 |
| siRNA4+ CTLs + FK506 | ND | ND | 611 ± 95 | 0 ± 0 |
| Peptide . | Lytic . | EBNA1 . | EBNA3 . | Irrelevant . |
|---|---|---|---|---|
| Donor 1 | ||||
| NT CTLs | 243 ± 47 | 1202 ± 154 | 257 ± 47 | 0 ± 0 |
| irr-siRNA+ CTLs | 242 ± 4 | ND | 109 ± 4 | 1 ± 1.7 |
| siRNA4+ CTLs + FK506 | 319 ± 61 | 1050 ± 77 | 248 ± 61 | 1.7 ± 2.1 |
| Donor 2 | ||||
| NT CTLs | 12 ± 1.5 | ND | 143 ± 23 | 0 ± 0 |
| irr-siRNA+ CTLs | 14 ± 3.1 | ND | 224 ± 16 | 0.3 ± 0.6 |
| siRNA4+ CTLs + FK506 | 5 ± 1.2 | ND | 230 ± 16 | 0.7 ± 0.6 |
| Donor 3 | ||||
| NT CTLs | 111 ± 10 | ND | 0 ± 0 | 1.3 ± 1.5 |
| irr-siRNA+ CTLs | 41 ± 10 | ND | 0 ± 0 | 0.7 ± 0.6 |
| siRNA4+ CTLs + FK506 | 64 ± 15 | ND | 0 ± 0 | 2 ± 1 |
| Donor 4 | ||||
| NT CTLs | ND | ND | 701.3 ± 89.5 | 0 ± 0 |
| irr-siRNA+ CTLs | ND | ND | 356 ± 48.1 | 0 ± 0 |
| siRNA4+ CTLs + FK506 | ND | ND | 611 ± 95 | 0 ± 0 |
Numbers are mean ± SD of interferonγ (IFNγ) spot-forming cells/105 cytotoxic T lymphocytes (CTLs).
EBV indicates Epstein-Barr virus; NT-CTLs, nontransduced cytotoxic T lymphocytes; siRNA, small interfering RNA; irr-siRNA, irrelevant si-RNA; and ND, not determined.
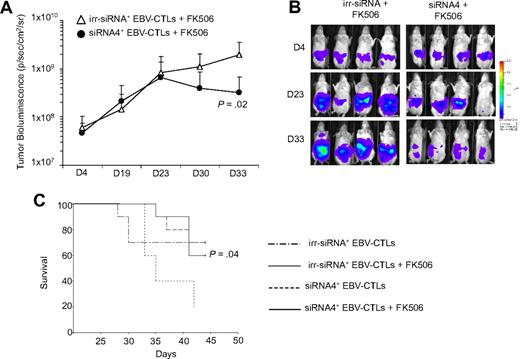
siRNA4+ EBV-CTLs have improved control of tumor growth in vivo in the presence of FK506
To assess whether siRNA4+ EBV-CTLs could control the growth of EBV+ lymphomas in the presence of FK506 in vivo, we used a SCID mouse xenograft model.30 Eight-week-old sublethally irradiated SCID mice (8 mice/group) were implanted with FFLuc-labeled EBV+ lymphomas in the peritoneal cavity. Light emission by tumor cells was monitored as an indication of tumor growth. Once progressive increase of bioluminescence occurred (usually 3-4 days after tumor injection) mice were treated intraperitoneally either with 2 doses of irr-siRNA+ EBV-CTLs or siRNA4+ EBV-CTLs, followed by intraperitoneal injection of IL-2 (1000 U/mice) and FK506 (10 mg/kg) 3 times a week.30 Control groups received an equivalent amount of IL-2 but not FK506. As shown in Figure 5A and B, the tumor bioluminescence of mice treated with irr-siRNA+ CTLs and FK506 progressively increased (from 6 × 107 ± 4 × 107 to 1.9 × 109 ± 1.6 × 109 p/s/cm2/sr by day 33) compared with mice receiving siRNA4+ CTLs and FK506 (from 5.3 × 107 ± 2 × 107 to 3.2 × 108 ± 3.6 × 108 p/s/cm2/sr by day 33; P = .02). Control of tumor growth by siRNA4+ CTLs in presence of FK506 was similar to that obtained in mice treated with irr-siRNA+ EBV-CTLs or siRNA4+ EBV-CTLs without FK506 (tumor bioluminescence 3.3 × 108 ± 2.8 × 108 and 4.4 × 108 ± 1.9 × 108, respectively, by day 33). The control of tumor growth in mice receiving siRNA4+ EBV-CTLs in the presence of FK506 translated into an improved survival of these mice by day 40 after tumor injection (P = .04) compared with mice receiving irr-siRNA+ CTLs and FK506 (Figure 5C). Hence, siRNA4+ EBV-CTLs can control tumor growth in vivo in the presence of FK506.
siRNA4+ EBV-CTLs retain their function in vivo in the presence of FK506. To evaluate in vivo antitumor activity, irr-siRNA+ and siRNA4+ EBV-CTLs were injected intraperitoneally in SCID mice bearing EBV+ lymphoma labeled with FFLuc. EBV-CTLs were transferred 4 and 11 days after intraperitoneal tumor implant. Tumor growth was monitored using the IVIS in vivo imaging system. IL-2 and FK506 were injected intraperitoneally 3 times per week. (A) By 33 days after CTL infusion, tumor growth, measured as maximum photon/sec/cm2/steradian (p/s/cm2/sr), was significantly greater in mice receiving irr-siRNA+ EBV-CTLs and FK506 compared with mice (8 mice per group) receiving siRNA4+ EBV-CTLs and FK506. Lines represent the average light emission ± SD. (B) Pictures of 4 representative mice per group. (C) The survival curve for SCID mice bearing EBV+ lymphoma that received irr-siRNA+ or siRNA4+ EBV-CTLs and IL-2 and FK506 intraperitoneally 3 times/week. Control mice received irr-siRNA+ or siRNA4+ EBV-CTLs and IL-2 but not FK506.
siRNA4+ EBV-CTLs retain their function in vivo in the presence of FK506. To evaluate in vivo antitumor activity, irr-siRNA+ and siRNA4+ EBV-CTLs were injected intraperitoneally in SCID mice bearing EBV+ lymphoma labeled with FFLuc. EBV-CTLs were transferred 4 and 11 days after intraperitoneal tumor implant. Tumor growth was monitored using the IVIS in vivo imaging system. IL-2 and FK506 were injected intraperitoneally 3 times per week. (A) By 33 days after CTL infusion, tumor growth, measured as maximum photon/sec/cm2/steradian (p/s/cm2/sr), was significantly greater in mice receiving irr-siRNA+ EBV-CTLs and FK506 compared with mice (8 mice per group) receiving siRNA4+ EBV-CTLs and FK506. Lines represent the average light emission ± SD. (B) Pictures of 4 representative mice per group. (C) The survival curve for SCID mice bearing EBV+ lymphoma that received irr-siRNA+ or siRNA4+ EBV-CTLs and IL-2 and FK506 intraperitoneally 3 times/week. Control mice received irr-siRNA+ or siRNA4+ EBV-CTLs and IL-2 but not FK506.
Discussion
We have shown that EBV-CTLs can be made resistant to FK506, the most common immunosuppressive drug used for liver, heart, and renal transplant recipients.14 This effect is obtained by a selective siRNA-mediated knockdown of FKBP12,19 a key protein that, after FK506 biding, blocks the activation of the calcineurin pathway, which in turn inhibits NFAT activation.18 As a consequence, even at doses of FK506 that inhibited EBV-CTLs with unmodified levels of FKBP12, gene-modified CTLs continue to proliferate and function as antitumor effector cells in vitro and in vivo in a xenograft model. This strategy can therefore preserve the function of desirable T cells, while maintaining suppression of alloreactive T cells. The approach could be adapted for the control of PTLDs or for other viral infections that cause morbidity and mortality in patients receiving solid organ transplantation.11,33-35
Recipients of SOT receive life-long immunosuppression to prevent rejection of the transplanted organ.12 As a result, they have increased susceptibility to a range of viral infections,11,33,35 and in particular EBV infection can induce the occurrence of often fatal lymphomas.36 Although adoptive transfer of virus-specific T cells have proven safe in SOT as well as HSC transplant recipients,11 the continuous immunosuppressive environment in SOT recipients limits proliferation and persistence of these cells in distinction to their expansion after HSC transplantation.1,2 Although the short-term effects of adoptively transferred EBV-CTLs may control lymphoproliferative diseases in SOT recipients, they act imperfectly to control the high virus load in these patients,7 and their lack of persistence means they cannot readily be used as prophylaxis to provide long-term control of EBV reactivation. The immunosuppressive drugs received by subject after SOT are designed specifically to inhibit T cells and reduce their ability to secrete and respond to cytokines upon stimulation.
We chose to block the function of FK506 by stably silencing the expression of FKBP12 using retroviral transduction with a specific siRNA vector, based on previous work in knockout mice showing that FK506-induced growth inhibition was abolished in FKBP12-deficient T cells and that these cells had normal function in response to antigen stimulation.19 FK506 is an immunophilin-binding drug that specifically targets FKBP12.19 Down-regulation of FKBP12 should prevent the formation of the FK506-FKBP12 complex that binds to calcineurins A and B and inhibits the dephosphorylation of cytoplasmic nuclear factor of activated T cells (NFAT), which translocates to the nucleus to initiate IL-2 transcription in activated T cells.18 FKBP12, however, is an abundant protein and therefore it was not clear whether it would be susceptible to knockdown. Indeed of 17 siRNAs only 5 produced more than 50% inhibition and only 1 induced more than 80% inhibition, and was chosen for further studies. Our data demonstrate that silencing of FKBP12 in EBV-CTLs allows them to proliferate in the presence of the drug, so that their functionality should not be impaired in vivo when patients continue on their immunosuppressive regimen. Although other FKBPs (such as FKBP12.6 and FKBP51) are present in T cells, their role in mediating FK506-induced immunosuppression is dispensable, likely due to the their limited accessibility or lower binding affinity to the drug.19 The substantial retained proliferation of our FKBP12-silenced CTLs in the presence of FK506 supports this interpretation.
Although previous studies showed that FKBP12-deficient murine T cells were not dysfunctional,19 down-regulation of this protein in human EBV-CTLs may alter critical effector T-cell functions, such as cytotoxic activity, activation, and expansion after antigen-specific stimulation, or may alter phenotype or antigen specificity. Our data show that FKBP12-silenced EBV-CTLs have no such alterations. Hence, siRNA4+ EBV-CTLs retain their major histocompatibility complex–restricted cytotoxic activity, produce IFNγ on exposure to EBV-associated antigens, and proliferate in the presence of FK506. As a result, the control of lymphoma growth in our in vivo xenogenic mouse model was significantly prolonged in mice receiving FK506.
FK506 is not an exclusive ligand for FKPB12. Rapamycin, another immunosuppressive agent used in SOT recipients,37 also binds to the FKBP12 to produce T-cell inhibition.18 Although rapamycin acts through the mammalian target of rapamycin rather than the calcineurin pathway,18 the beneficial effects of FKBP12-silenced T cells may also be extended to patients receiving rapamycin immunosuppression (supplemental Figure 3).
We conclude that the down-regulation of FKBP12 in EBV-CTLs can be used to sustain their proliferative activity even in the presence of FK506, and provide efficient control of EBV-related lymphomas. A similar approach may be of value for protecting other pathogen-specific T cells such as cytomegalovirus- and adenovirus-specific CTLs38 that could be infused in patients after solid organ transplantation, thereby helping reduce morbidity and mortality from infection in these patients,33-35 while retaining organ engraftment. Combinations of pharmacologic immunosuppression, including mycophenolate and steroids in addition to calcineurin inhibitors, are often used and resistance to multiple immunosuppressive drugs may be explored. Obviously other obstacles to adoptive EBV-CTL therapy in solid organ transplantation would remain, including cytokine dependency of CTLs and the role and direct immunosuppressive effects of the tumor environment, and will need further elucidation. The combination of different strategies will help in designing the most successful approach.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported in part by P50CA126752 from the National Institutes of Health, and a Leukemia & Lymphoma Society Specialized Center of Research. B.S. is supported by National Institutes of Health RO1 R01CA131027 and by a Leukemia & Lymphoma Society Translational Research grant. G.D. is supported by the Doris Duke Charitable Foundation/Clinical Scientist development award and by a Leukemia & Lymphoma Society Translational Research grant. B.D.A. is the recipient of a fellowship from the Società Italiana di Ematologia Sperimentale.
National Institutes of Health
Authorship
Contribution: B.D.A. designed the research, performed the majority of the experiments, analyzed the data, and wrote the manuscript; G.D. designed the research, supervised the generation of the retroviral vectors, analyzed the data, and wrote the manuscript; C.Q. and L.E.H. performed some in vitro experiments; L.Z. and M.Z. provided technical assistance for some of the in vitro experiments; F.P., H.E.H., M.K.B., and C.M.R. provided assistance in the design of the research and critically reviewed the manuscript; B.S. designed the research, analyzed the data, and wrote the manuscript; and all authors approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Barbara Savoldo, Center for Cell and Gene Therapy, Baylor College of Medicine, 6621 Fannin St, MC 3-3320, Houston, TX 77030; e-mail: bsavoldo@bcm.tmc.edu.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal