Abstract
Growing evidence indicates antibody-dependent cellular cytotoxicity (ADCC) contributes to the clinical response to monoclonal antibody (mAb) therapy of lymphoma. Recent in vitro analysis suggests C3b can inhibit mAb-induced natural killer (NK)–cell activation and ADCC. Further studies were conducted to assess the effect of C3 depletion on mAb-induced NK activation and therapy of lymphoma. Normal human serum inhibited the ability of rituximab-coated lymphoma cells to activate NK cells as previously reported. Serum did not inhibit NK-cell activation when it was preincubated with cobra venom factor (CVF) to deplete C3. Similar results were found when transudative pleural fluid or nonmalignant ascites was used as surrogates for extravascular fluid, suggesting the inhibitory effect of complement may be present in the extravascular compartment, in which many malignant lymphocytes reside. In vivo, C3 was depleted before mAb treatment in a syngeneic murine model of lymphoma. Survival of lymphoma-bearing mice after treatment with CVF plus mAb and with a human C3 derivative with CVF-like functions (HC3-1496) plus mAb was both superior to that of mAb alone. These studies show that complement depletion enhances NK-cell activation induced by rituximab-coated target cells and improves the efficacy of mAb therapy in a murine lymphoma model.
Introduction
Monoclonal antibody (mAb)–based therapies are now standard treatment for various malignancies. The chimeric anti-CD20 mAb, rituximab, remains the “gold standard” with respect to clinically effective mAbs. Antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) both have been shown to contribute to the antitumor activity of mAbs in preclinical models. However, their relative importance in the clinical efficacy of rituximab and other mAbs remain unclear. Data from both laboratory models and correlative clinical studies suggest that ADCC plays a significant role in the antitumor effects of mAbs. Clynes et al1,2 showed that the therapeutic effect of mAbs is lost in Fcγ-receptor knockout mice. In clinical investigations, 3 independent studies have shown that single-agent rituximab is more effective in patients with Fcγ receptor III (CD16) polymorphisms associated with higher affinities for human IgG. Patients homozygous for the V158 polymorphism (VV) on CD16 have higher clinical response rates to rituximab than do patients who are carriers for F158 (VF or FF), suggesting that Fc receptors on effector cells play a key role in the therapeutic effect of rituximab.3-5
Rituximab has also been shown by in vitro studies to be highly efficient in mediating CDC of various B-cell lines as well as fresh samples.6-9 Several in vivo tumor models suggest that the antitumor activity of rituximab is dependent, at least in part, on complement.10-12 In addition, clinical observations provide evidence that complement is activated during treatment with rituximab.13 In a small study, complement activation was found to correlate with the infusional toxicity often seen in patients with high numbers of circulating B cells.14 However, it is unclear whether this is a causative relationship. Recently, Tawara et al15 reported that complement activation plays a key role in the antibody-induced infusion toxicity of mAbs in animal models. Those studies have shown that modified mAbs with limited complement fixing ability resulted in reduced infusion reactions. However, the lack of complement activation did not affect the antitumor activity.15 In addition, a clinical study found that expression levels of complement inhibitors failed to predict the clinical outcome of rituximab treatment.9 Although there is solid laboratory evidence that complement may be important for the antitumor effect of mAbs, the clinical evidence is less clear.
We previously described an in vitro assay that measures mAb-induced natural killer (NK) activation through assessing NK cell–surface phenotypes.16 This system was used to evaluate the relationship between complement fixation and the ability of rituximab-coated targets to induce NK-cell activation. Using this assay, we found that complement interferes with the binding of NK cells to rituximab, preventing the activation of NK cells as measured by the down-modulation of CD16 and the up-regulation of the activation markers, CD54 and CD69. This inhibition was dependent on C3b. NK cell–mediated lysis of rituximab-coated target cells was also inhibited by complement fixation.17 These results suggest that, if ADCC is indeed the central mechanism of action, complement activation may actually be limiting the therapeutic effect of rituximab in contrast to the traditional assumption that complement activation contributes to the efficacy of rituximab.
In our current studies, we used transudative pleural fluid and nonmalignant ascites as surrogates for extravascular fluid to determine whether the inhibitory effects of complement might be important in the extravascular compartment as well as in the circulation. We also evaluated the effect of complement depletion on the ability of rituximab-coated target cells to activate NK cells and on the efficacy of a mAb in a murine model previously used to study ADCC. Complement was present in transudative pleural fluid and nonmalignant ascites, and it inhibited NK-cell activation induced by rituximab-coated targets. MAb-coated murine lymphoma cells activated murine NK cells in vitro as they did in the human system. The use of complement-depleting agents enhanced NK-cell activation in vitro and improved the efficacy of a mAb therapy in vivo in a murine model. These results suggest that complement activity in both the circulation and the extravascular compartment may be inhibiting rituximab-induced NK-cell activation and that limiting complement activity may be an appropriate strategy to enhance the therapeutic efficacy of anticancer mAbs.
Methods
Antibodies and reagents
Rituximab (Biogen-Idec and Genentech) was purchased commercially. The therapeutic murine mAb, MS11G6 (IgG2a), was obtained from tissue culture supernatant by protein A affinity chromatography.18 Cobra venom factor (CVF) was prepared from lyophilized venom from Naja kaouthia as previously described.19 HC3-1496 is a human C3/CVF hybrid protein containing a 168–amino acid residue substitution of CVF sequence at the C terminus of the α-chain of C3 (humanized CVF; InCode Biopharmaceutics Inc). The plasmid preparation, protein expression, and purification were performed essentially as previously described.20
Samples from human subjects
Informed consent from subjects was obtained in accordance with the Declaration of Helsinki before use of all human samples, which were obtained under protocols approved by the institutional review board of the University of Iowa. Normal human serum and peripheral blood mononuclear cells (PBMCs) were obtained from healthy volunteers and processed and analyzed as previously reported.16 Briefly, mononuclear cells were isolated, and red blood cells were removed by resuspending cells in 5 mL of red cell lysis buffer according to standard procedures. Pleural fluid samples were obtained from patients with congestive heart failure and determined to be transudative, based on a pleural fluid LDH-to-serum LDH ratio of less than 0.60. Nonmalignant ascites samples were obtained from patients with liver disease and were also found to be transudates. Fluid samples were cryopreserved. Few cells were present at the time of cryopreservation, and no viable cells were noted on microscopic evaluation of thawed samples. Aliquots of serum, pleural fluid, and ascites were used unmodified or heated to 57°C for 30 minutes to produce heat-inactivated serum, pleural fluid, and ascites, respectively.
C1q Enzyme-linked immunosorbent assay
Samples of serum, pleural fluid, and ascites were analyzed for C1q protein by enzyme-linked immunosorbent assay (ELISA). Flat-bottomed 96-well EIA/RIA plates (Corning Inc) were coated with 0.5 μg/mL anti-C1q IgY (GenWay Biotec) overnight at 4°C. Wells were washed with 0.05% Tween-20 and blocked with 1% BSA-PBS for 1 hour. After washing, 100 μL of standards and samples were applied to the plate for 2 hours. Known concentrations of C1q protein (BioDesign) was used as the standard. Monoclonal mouse IgG anti-C1q from the hybridoma 4A4B11 (ATCC) was added for 1 hour to detect bound C1q. After washing, goat anti–mouse Ig(H+L)–HRP (Southern Biotechnology Associates) was added for 30 minutes. TMB substrate solution (Sigma-Aldrich) was added after washing and read at 450 nm on a THERMOmax microplate reader. Results were analyzed with the use of SOFTmax software (Molecular Devices) and reported in micrograms per milliliter (μg/mL). Assays were performed in triplicate per sample.
C3b deposition
Raji cells were incubated at a density of 2.5 × 106 cells/mL with 5 μg/mL rituximab in the presence of various concentrations of serum, heat inactivated serum, pleural fluid, or ascites fluid at 37°C for 4 hours. Cells were washed and stained with anti–human C3b-A488 (clone 3E7) for 15 minutes at 4°C. Cells were washed and analyzed by flow cytometry.
NK-cell activation
NK cell activation was measured by using a phenotypic assay as previously reported. This assay uses fresh normal donor PBMCs as a source of NK cells and Raji cells as CD20-positive target cells.16 PBMCs and Raji cells were mixed at a 1:1 effector-to-target ratio at a final concentration of 106 PBMCs and 106 Raji cells/mL. Various concentrations of rituximab, serum, ascites, or pleural fluid (untreated, heat-inactivated, or treated with CVF) were added as indicated. Samples were then cultured for 20 hours at 37°C before phenotypic analysis.
NK-cell phenotypic analysis
Immunofluorescent staining was performed on cocultured cells to assess changes in NK-cell phenotype. Briefly, in the human system, cells were washed and stained with directly conjugated commercial antibodies, including anti–human CD56 Alexa Fluor 647, CD54 PE (BD PharMingen), CD16 FITC (Serotec), and CD3 PE-Cy7 (Invitrogen) per the manufacturer's protocol for 15 minutes on ice. Cells were washed twice, fixed in 2% formaldehyde solution, and stored at 4°C for flow cytometry within 24 hours. Flow cytometric analysis (4-color) was performed on the LSR II (BD Immunocytometric Systems). Data were analyzed with the use of FlowJo software (TreeStar Inc). CD16 and CD54 expression of NK cells was determined by gating on CD3−CD56+ lymphocytes; CD16 expression was reported as median fluorescence. In prior studies, we found that NK-cell expression of CD54 was bimodal, with activated NK cells expressing bright CD54. Therefore, NK-cell activation is reported as the percentage of NK cells that were CD54bright.
In the murine model, splenocytes obtained from B6C3F1 mice (female C57BL/6 × male C3H; Harlan) were used as the source for NK cells because NK cells from purebred C3H mice are NK1.1 negative. 38C13 lymphoma cells were used as the target cells. Splenocytes and 38C13 cells were cocultured in 1:1 ratio along with various concentrations of MS11G6 antilymphoma mAb in the presence of 20% syngeneic mouse serum or heat-inactivated syngeneic mouse serum in RPMI complete medium. After 20 hours of incubation at 37°C, cells were washed and stained with anti–mouse NK1.1-PE, DX5-APC, CD16/32-APC-Cy7, CD54-FITC, and CD69-PerCP-Cy5.5 (BD PharMingen) per the manufacturer's recommendations. For measurement of IFNγ, cells were treated with Brefeldin A for an additional 4 hours. Cells were washed, fixed, and then permeabilized and stained with anti–mouse IFNγ-PE-Cy7 (BD PharMingen). NK cells were identified as NK1.1+DX5+ cells. CD54 and CD69 expression was reported as median fluorescence. Intracellular IFNγ was reported as the percentage of positive cells.
38C13 murine lymphoma model
The 38C13 murine lymphoma tumor model has been described previously.18,21-23 Female C3H mice were purchased from Harlan and housed in the University of Iowa Animal Care Facility. The 38C13 cells (5 × 103) growing in log phase were injected intraperitoneally into 6- to 9-week-old mice. Day 0 was defined as the day of tumor inoculation. Mice were injected with 10 μg of CVF or HC3-1496 in 0.1 mL of PBS on day 3 and day 5. Mice were treated with doses of 0.1 mg of MS11G6 antilymphoma mAb in 0.2 mL of PBS intraperitoneally 4 hours after the initial CVF or HC3-1496 injection on day 3. Survival was determined for each group, and difference in time to death was assessed by using the log-rank test (Mantel-Cox). The University of Iowa Animal Care and Use committees approved all of the mice experiments.
Determination of complement in murine serum
Complement activity in murine serum was determined by using the hemolytic assay as previously described.19 Briefly, 15 μL mouse serum was diluted 2-fold with VBS++. Aliquots (10 μL) were then incubated with 20 μL antibody-sensitized rabbit erythrocytes (5 × 108 cells/mL) for 30 minutes at 37°C in VBS++. After incubation, the reaction was stopped by dilution with cold VBS++, intact erythrocytes were pelleted by centrifugation (425g for 8 minutes), and the amount of lysis was measured spectrophotometrically at 412 nm.
Results
Complement activity in extravascular fluid surrogates
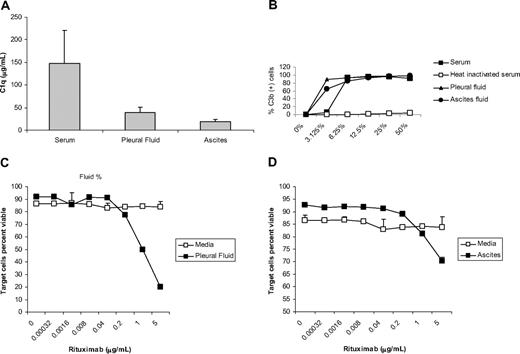
We have demonstrated previously that complement in serum inhibits NK-cell activation induced by rituximab-coated target cells.17 However, most malignant cells in most patients with lymphoma are in the lymph nodes, ie, in the extravascular compartment. Remarkably, little is known about the presence or activity of complement in the extravascular compartment. We, therefore, assessed complement activity in extravascular fluid by using transudative pleural fluid and ascites from nonmalignant patients as surrogates. An ELISA showed that C1q is present in pleural fluid and ascites, although at concentrations of C1q lower that that seen in serum (Figure 1A). C3 was deposited on rituximab-coated Raji cells incubated with pleural fluid and ascites, even at very low (3.125%) concentrations of fluid (Figure 1B). In contrast, pleural fluid and ascites had insufficient complement to lyse red blood cells in a traditional CH50 assay (data not shown). This suggests pleural fluid and ascites have enough of the early components of complement to activate C3, but lower amounts of the later components of complement that form the complement membrane attack complex. The ascites and pleural fluid were able to mediate lysis of rituximab-coated Raji cells after a 20-hour incubation, which is longer than that used in the CH50 assay (Figure 1C-D). No lysis was seen when fluids were heat inactivated (data not shown), providing further evidence that complement was responsible for the observed lysis.
Transudative pleural fluid and nonmalignant ascites contain active complement. ELISA analysis showing C1q is detectable in transudative pleural and ascitic fluid but at levels lower than that seen in serum (A). Raji cells were incubated with 5 μg/mL rituximab and various concentrations of serum, heat-inactivated serum, ascites, or pleural fluid, and the percentage of cells showing deposition of C3b was determined by flow cytometry. Deposition of C3b was seen on the cell surface in all samples except heat-inactivated serum (B). The percentage of viable target cells remaining after the addition of pleural fluid (C) or ascites (D) was determined with the use of flow cytometry by counting remaining annexin V– and propidium iodide–negative target cells (n = 3). Error bars represent SD of the mean.
Transudative pleural fluid and nonmalignant ascites contain active complement. ELISA analysis showing C1q is detectable in transudative pleural and ascitic fluid but at levels lower than that seen in serum (A). Raji cells were incubated with 5 μg/mL rituximab and various concentrations of serum, heat-inactivated serum, ascites, or pleural fluid, and the percentage of cells showing deposition of C3b was determined by flow cytometry. Deposition of C3b was seen on the cell surface in all samples except heat-inactivated serum (B). The percentage of viable target cells remaining after the addition of pleural fluid (C) or ascites (D) was determined with the use of flow cytometry by counting remaining annexin V– and propidium iodide–negative target cells (n = 3). Error bars represent SD of the mean.
Extravascular fluid surrogates inhibit NK cell CD16 down-modulation and CD54 up-regulation induced by rituximab-coated target cells
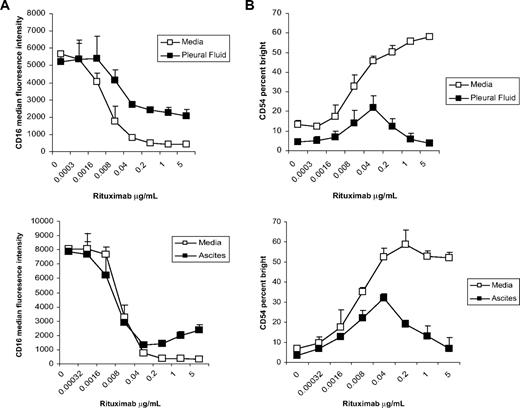
To determine whether complement activity in extravascular fluid inhibits NK-cell activation, PBMCs from healthy donors were cultured with Raji cells and rituximab in the presence of pleural fluid or ascites. As with serum, pleural fluid and ascites inhibited the down-modulation of NK cell CD16 induced by rituximab-coated targets at rituximab concentrations greater than 0.04 μg/mL (Figure 2A). Both pleural fluid and ascites also inhibited the up-regulation of NK cell CD54 at rituximab concentrations greater than 0.04 μg/mL (Figure 2B). Similar results were seen when CD69 and IFN-γ were used as markers of NK-cell activation (data not shown). These data suggest that complement activity in pleural fluid and ascites both inhibit NK-cell activation induced by rituximab-coated target cells. These results were not limited to Raji cells as targets. Similar results were found when other B-cell lines or single-cell suspensions of primary lymphoma cells were used as target cells (data not shown).
Transudative pleural fluid and nonmalignant ascites inhibit rituximab-induced NK cell CD16 down-modulation and CD54 up-regulation. PBMCs and Raji cells were mixed at a 1:1 ratio for 20 hours in the presence or absence of 50% pleural fluid or ascites with various concentrations of rituximab. NK cell–surface marker expression was determined by flow cytometry with gating on CD3−, CD56+ lymphocytes. (A) NK cell CD16, expressed as median fluorescence, in the absence and presence of pleural fluid or ascites fluid (n = 3 samples per group). (B) NK cell CD54, expressed as a percentage of CD54 bright, in the absence and presence of pleural fluid or ascites fluid (n = 3 samples per group). Error bars represent SD of the mean.
Transudative pleural fluid and nonmalignant ascites inhibit rituximab-induced NK cell CD16 down-modulation and CD54 up-regulation. PBMCs and Raji cells were mixed at a 1:1 ratio for 20 hours in the presence or absence of 50% pleural fluid or ascites with various concentrations of rituximab. NK cell–surface marker expression was determined by flow cytometry with gating on CD3−, CD56+ lymphocytes. (A) NK cell CD16, expressed as median fluorescence, in the absence and presence of pleural fluid or ascites fluid (n = 3 samples per group). (B) NK cell CD54, expressed as a percentage of CD54 bright, in the absence and presence of pleural fluid or ascites fluid (n = 3 samples per group). Error bars represent SD of the mean.
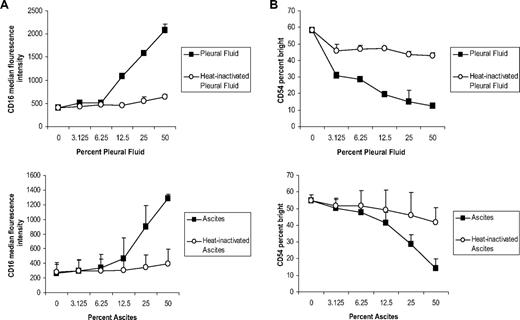
Inhibitory effects of extravascular fluid surrogates are dose dependent and abrogated by heat inactivation
To investigate whether the effects of extravascular fluid were dose dependent, the amount of pleural fluid and ascites was titrated in vitro. The inhibitory effects on NK cell CD16 down-modulation were greater as the concentration of pleural and ascites fluid was increased (Figure 3A). Similarly, the inhibition of NK cell CD54 was also dependent on the concentration of extravascular fluid, with greater inhibition at higher concentrations of pleural fluid or ascites (Figure 3B). As with serum and the deposition of C3, the inhibitory effects of pleural fluid or ascites were abrogated by heat inactivation, suggesting that the inhibition is due to complement activity.
Inhibitory effect of transudative pleural fluid and nonmalignant ascites is dose dependent and abrogated by heat inactivation. PBMCs and Raji cells were mixed at a 1:1 ratio for 20 hours in various concentrations of pleural fluid, ascites, or heat-inactivated samples in the presence of 5 μg/mL rituximab. NK cell–surface marker expression was determined by using flow cytometry with gating on CD3−, CD56+ lymphocytes. (A) NK cell CD16, expressed as median fluorescence, after incubation with various concentrations of pleural fluid, ascites, or heat-inactivated samples (n = 3 samples per group). (B) NK cell CD54, expressed as a percentage of CD54 bright, after incubation with various concentrations of pleural fluid, ascites, or heat-inactivated samples (n = 3 samples per group). Error bars represent SD of the mean.
Inhibitory effect of transudative pleural fluid and nonmalignant ascites is dose dependent and abrogated by heat inactivation. PBMCs and Raji cells were mixed at a 1:1 ratio for 20 hours in various concentrations of pleural fluid, ascites, or heat-inactivated samples in the presence of 5 μg/mL rituximab. NK cell–surface marker expression was determined by using flow cytometry with gating on CD3−, CD56+ lymphocytes. (A) NK cell CD16, expressed as median fluorescence, after incubation with various concentrations of pleural fluid, ascites, or heat-inactivated samples (n = 3 samples per group). (B) NK cell CD54, expressed as a percentage of CD54 bright, after incubation with various concentrations of pleural fluid, ascites, or heat-inactivated samples (n = 3 samples per group). Error bars represent SD of the mean.
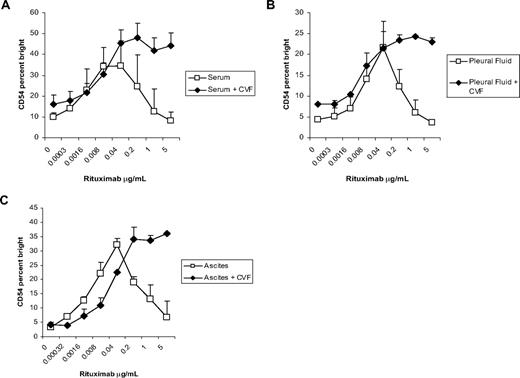
Depletion of complement enhances NK cell CD54 up-regulation in the presence of extravascular fluid surrogates
CVF is a structural and functional analog of the complement component, C3, which forms a bimolecular enzyme able to proteolytically activate C3 and C5 (C3/C5 convertase). In contrast to the C3b-containing enzyme, the CVF-containing enzyme is stable and resistant to control mechanisms, resulting in depletion of complement activity.24 To determine whether depletion of complement activity enhances NK cell activation, pleural fluid and ascites were incubated with CVF before use in the assay. In the absence of CVF treatment, NK cell CD54 up-regulation was inhibited by both the pleural fluid and ascites. When serum (Figure 4A), pleural fluid (Figure 4B), or ascites (Figure 4C) was incubated with CVF, the inhibitory effect was abrogated, resulting in increased NK cell CD54 up-regulation at rituximab concentrations greater than 0.04 μg/mL. CVF had no effect on mAb-induced NK activation in the absence of complement-containing fluid (data not shown). These results suggest that depletion of C3 enhances NK-cell activation in the presence of rituximab-coated target cells and provide further evidence that the observed inhibitory effect on NK activation is due to complement activity.
CVF enhances NK cell CD54 up-regulation in the presence of complement and rituximab-coated target cells. PBMCs and Raji cells were mixed at a 1:1 ratio for 20 hours in the presence of 50% serum, pleural fluid, or ascites with or without the addition of CVF in various concentrations of rituximab. NK cell–surface marker expression was determined by using flow cytometry with gating on CD3−CD56+ lymphocytes. (A) NK cell CD54, expressed as a percentage of CD54bright, after culture in serum or serum plus CVF (n = 3 samples per group). (B) NK cell CD54, expressed as a percentage of CD54 bright, after culture in pleural fluid or pleural fluid plus CVF (n = 3 samples per group). (C) NK cell CD54, expressed as a percentage of CD54 bright, after culture in ascites or ascites plus CVF (n = 3 samples per group). Error bars represent SD of the mean.
CVF enhances NK cell CD54 up-regulation in the presence of complement and rituximab-coated target cells. PBMCs and Raji cells were mixed at a 1:1 ratio for 20 hours in the presence of 50% serum, pleural fluid, or ascites with or without the addition of CVF in various concentrations of rituximab. NK cell–surface marker expression was determined by using flow cytometry with gating on CD3−CD56+ lymphocytes. (A) NK cell CD54, expressed as a percentage of CD54bright, after culture in serum or serum plus CVF (n = 3 samples per group). (B) NK cell CD54, expressed as a percentage of CD54 bright, after culture in pleural fluid or pleural fluid plus CVF (n = 3 samples per group). (C) NK cell CD54, expressed as a percentage of CD54 bright, after culture in ascites or ascites plus CVF (n = 3 samples per group). Error bars represent SD of the mean.
Murine serum blocks mAb-induced activation of murine NK cells in a manner similar to that seen in the human system
We previously demonstrated that the in vivo therapeutic activity of murine anti-idiotype mAb (MS11G6) against the murine 38C13 B-cell lymphomas is dependent, at least in part, on NK cells.22 This model also has the advantage of using an antilymphoma mAb in syngeneic immunocompetent mice. Initial studies were done to assess whether mAb-coated murine cells can induce phenotypic changes in murine NK cells in a manner similar to that seen in the human system. These studies have shown that 38C13 murine lymphoma cells coated with anti-idiotype mAb can activate murine NK cells as indicated by up-regulation of CD69 and production of IFNγ. Up-regulation of CD54 was also observed, but it was less pronounced than observed in the human system. In contrast to the human system in which mAb-coated target cells induce down-modulation of NK cell CD16, mAb-coated murine target cells induced no significant change in murine NK cell CD16/32, probably because of the inherent differences between human and murine systems. No changes in NK phenotype were observed when 38C13 lymphoma cells that lack the idiotype target antigen were used as target cells (data not shown).
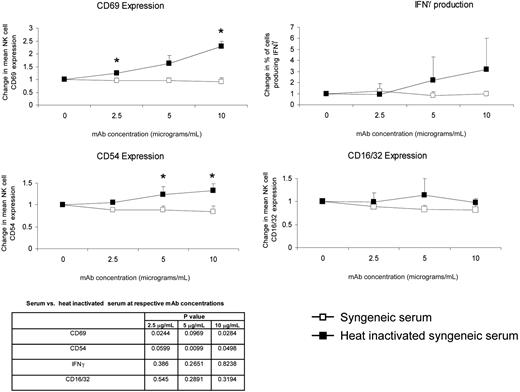
We then evaluated the effect syngeneic murine serum and heat-inactivated syngeneic murine serum has on the ability of mAb-coated murine target cells to activate murine NK cells. As shown in Figure 5, mAb-coated target cells induced NK-cell activation in the presence of heat-inactivated murine serum as indicated by CD69 up-regulation, IFNγ production by NK cells, and more modest up-regulation of CD54. Changes indicative of NK activation were blocked by untreated serum. The finding in the murine model that serum blocks phenotypic evidence of NK activation mirrors that observed in the human system.
mAb-coated syngenetic murine lymphoma cells induce phenotypic changes indicative of murine NK activation. As in the human system, this effect is blocked by murine serum but not heat-inactivated murine serum. *P < .05 between serum and heat-inactivated serum.
mAb-coated syngenetic murine lymphoma cells induce phenotypic changes indicative of murine NK activation. As in the human system, this effect is blocked by murine serum but not heat-inactivated murine serum. *P < .05 between serum and heat-inactivated serum.
Depletion of complement improves the efficacy of mAb therapy in a murine B-cell lymphoma model
We used the 38C13 model to determine whether depletion of complement affects the efficacy of an antilymphoma mAb therapy. Mice were depleted of complement with the use of CVF or HC3-1496, a human C3 derivative protein with CVF-like functions. HC3-1496 resembles CVF in its C3-cleaving activity, but it does not activate C5. In vivo administration of both CVF and HC3-1496 has been shown to safely deplete complement in murine models.24,25
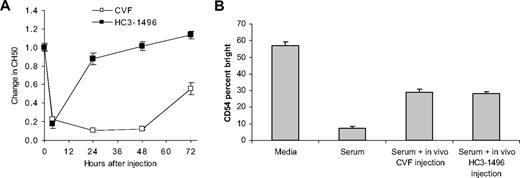
Single intraperitoneal injections of both CVF and HC3-1496 depleted complement. The depletion lasted longer with CVF than with HC3-1496 (Figure 6A). Serum from untreated mice inhibited the ability of mAb-coated target cells to activate NK cells, whereas serum obtained 6 hours after treatment of mice with CVF or HC3-1496 did not inhibit NK activation (Figure 6B), confirming in vivo depletion of complement can affect mAb-induced NK activation.
In vivo depletion of complement. Mice were treated with a single dose of CVF or HC3-1496 (n = 3 mice per group), and serum was harvested and evaluated for complement activity. Changes in CH50 from baseline were evaluated (A). Serum obtained at 6 hours was evaluated for its ability to inhibit activation of NK cells by mAb-coated target cells as indicated by up-regulation of CD54 (B). Error bars represent SD of the mean.
In vivo depletion of complement. Mice were treated with a single dose of CVF or HC3-1496 (n = 3 mice per group), and serum was harvested and evaluated for complement activity. Changes in CH50 from baseline were evaluated (A). Serum obtained at 6 hours was evaluated for its ability to inhibit activation of NK cells by mAb-coated target cells as indicated by up-regulation of CD54 (B). Error bars represent SD of the mean.
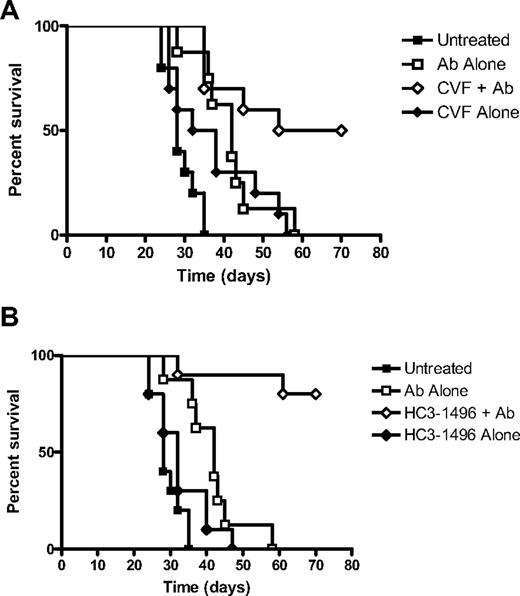
Mice were inoculated with 38C13 lymphoma cells and treated with a single dose of intraperitoneal MS11G6 three days after the tumor inoculation. Complement was depleted by intraperitoneal treatment of mice with either CVF or HC3-1496 four hours before MS11G6 treatment and once again on day 5. All untreated mice developed tumor and died with a median survival of 28 days. MS11G6 treatment alone increased the median survival to 42 days (untreated vs mAb alone; P < .001). CVF alone had a borderline effect on survival (untreated vs CVF alone; P = .05). Treatment with CVF enhanced the efficacy of the antilymphoma mAb therapy with 50% of mice remaining tumor-free (mAb alone vs mAb plus CVF; P = .03; Figure 7A). HC3-1496 alone had no statistically significant effect on survival (untreated vs HC3-1496; P = .15). HC3-1496 treatment enhanced the efficacy of mAb with 80% of mice remaining tumor free (mAb alone vs mAb plus HC3-1496; P < .001; Figure 7B). These data suggest that complement depletion alone may have a modest antitumor effect and that the depletion of complement by CVF or HC3-1496 improves the efficacy of a mAb therapy in this model.
CVF and HC3-1496 enhance the efficacy of monoclonal antibody therapy in vivo. Mice were inoculated intraperitoneally with 38C13 tumor cells on day 0. Select groups of mice were treated with antilymphoma IgG2a (MS11G6) on day 3, CVF on day 3 and day 5, or HC3-1496 on day 3 or day 5. (A) Survival of mice treated with MS11G6 alone, MS11G6 plus CVF, CVF alone, or untreated. (B) Survival of mice treated with MS11G6 alone, MS11G6 plus HC3-1496, HC3-1496 alone, or untreated (n = 10 mice per group)
CVF and HC3-1496 enhance the efficacy of monoclonal antibody therapy in vivo. Mice were inoculated intraperitoneally with 38C13 tumor cells on day 0. Select groups of mice were treated with antilymphoma IgG2a (MS11G6) on day 3, CVF on day 3 and day 5, or HC3-1496 on day 3 or day 5. (A) Survival of mice treated with MS11G6 alone, MS11G6 plus CVF, CVF alone, or untreated. (B) Survival of mice treated with MS11G6 alone, MS11G6 plus HC3-1496, HC3-1496 alone, or untreated (n = 10 mice per group)
Discussion
The role complement plays in mediating the clinical antitumor activity of mAb remains unclear. Various studies have shown that complement can induce in vitro lysis of mAb-coated target cells.6-9 However, we previously reported that complement can also inhibit the killing of target cells by blocking NK cell–mediated ADCC.17 The current studies were designed to begin evaluation of whether complement can paradoxically limit the efficacy of mAb therapy by suppressing NK activation and whether depletion of complement can actually enhance the efficacy of mAb. In the laboratory, normal human serum has been traditionally used to study mechanisms involving complement. However, most malignant lymphocytes reside in the extravascular compartment, where protein concentrations differ from those in circulation. The lack of available methods for obtaining extravascular fluid prevented the direct evaluation of complement activity in such fluid. Both transudative pleural fluid and ascites from patients with nonmalignant disease are filtered through the normal endothelial barrier in a manner similar to extravascular fluid. We, therefore, used transudative pleural fluid from patients with congestive heart failure and ascites from patients with nonmalignant liver disease as surrogates to assess how complement in the extravascular fluid affects the antitumor effects of mAbs.
Both congestive heart failure and cirrhosis has been known to induce systemic inflammation, resulting in complement protein consumption.26,27 Thus, pleural fluid and ascites are not ideal surrogates for extravascular fluid. The concentration of active complement in these surrogates may be less than what is expected to be found in the extravascular compartments. Indeed, we found that complement in both pleural fluid and ascites failed to mediate lysis in a traditional CH50 assay, although they did mediate CDC of rituximab-coated target cells after prolonged incubation. These fluids contained the components of complement responsible for initiating the complement cascade. C1q was detectable in both pleural fluid and ascites. C3b deposition on rituximab-coated target cells was at least as pronounced with these fluids as it was with serum. Most relevant to the underlying hypothesis that complement in the extravascular compartment might limit ADCC was the finding that the fluids inhibited NK-cell activation induced by rituximab-coated targets.
One of the more challenging aspects of evaluating the interactions between complement and ADCC is that both mechanisms can cause lysis of target cells. Determining whether ADCC or CDC is responsible for observed lysis is not possible by using traditional chromium release assays if both complement and effector cells are present. We previously demonstrated that C5-depleted serum blocks ADCC in a traditional chromium release assay.17 For the current studies, it was not practical to produce C5-depleted pleural fluid or ascites. We, therefore, used a change in NK-cell phenotype as a surrogate for NK activation and ADCC, because our previous studies have shown that changes in NK-cell phenotype (up-regulation of CD54 and down-modulation of CD16) correlate strongly with ADCC as measured by chromium release assays.16
If NK cell–mediated ADCC plays an important role in the therapeutic effects of rituximab and other mAbs and if complement fixation inhibits NK-cell activation and ADCC, then complement depletion could either decrease (by limiting CDC) or enhance (by increasing NK-mediated ADCC) the efficacy of mAb therapy. In vivo testing of this hypothesis requires a model in which NK cells, and not complement alone, contribute to the effects of therapy. The 38C13 model was selected because it is a syngeneic murine lymphoma system that targets an antigen known to be a good therapeutic target in humans (the idiotype) and has been extensively studied.18,21-23,28,29 Furthermore, as is the case with rituximab therapy in humans, there is evidence that the therapeutic effect of mAb in the 38C13 model is mediated in part by NK cells.22 Although there were quantitative differences in NK-cell phenotypic changes induced by mAb-coated target cells in the human and murine systems, we found the same general markers of NK activation (up-regulation of CD54 and CD69 and production of IFNγ) were found in both the human and murine systems. Thus, although the target antigen in the murine model we used is not CD20, the 38C13 lymphoma model represents a reasonable model to evaluate the in vivo role complement plays on mAb efficacy. As in the human system, murine serum blocked activation of murine NK cells induced by mAb-coated target cells. Most importantly, depletion of complement enhanced the efficacy of mAb therapy.
The data outlined in this report provide the first in vivo evidence that complement can inhibit the efficacy of mAb therapy and that depletion of complement is an alternative strategy for enhancing the efficacy of mAb therapy. Whether the enhanced ADCC seen with complement depletion is significant enough to counterbalance the therapeutic contribution of CDC in clinical therapy remains to be determined. There is probably a balance between the relative importance of CDC and ADCC in mediating the antitumor effects of mAb. Factors such as target antigen, epitope specificity, antigen affinity, Fc receptor affinity, mAb dose, location of malignant cells, presence of complement, and presence of infiltrating effector cells could all affect whether complement enhances, or reduces, the efficacy of mAb therapy.
Our data suggest that the effects of complement may be present in both the intravascular and extravascular compartments. It is also important to avoid oversimplifying the complexity of the complement system. The presence of early components of complement (C1-C4), with their ability to block NK activation and limit ADCC, may be distinct from the presence of the components of complement (C5-C9) involved in development of the membrane attack complex. Our findings indicating that pleural fluid and ascites can result in deposition of C3b on target cells, but not mediate cell lysis in traditional CH50 assays, suggest that complement could indeed have different effects in different compartments, even in a single person. Additional studies are needed to explore in more detail the actual levels of various complement proteins and activities in various fluid compartments. Further evaluation, including correlative studies in humans, is needed before we know whether complement is “friend or foe” related to the therapeutic effects of mAb in a particular clinical scenario.
Despite these limitations to the studies presented here, complement depletion remains a previously unappreciated potential strategy for enhancing the efficacy of mAb. CVF has been widely used in animal models to deplete complement, but it is highly immunogenic, which limits its potential clinical application. To address this issue, we engineered a hybrid protein in which a portion of the α chain at the C terminus of human C3 is replaced with homologous regions of the CVF β chain crucial to activity (HC3-1496).20,30 Using both CVF and HC3-1496, we found that depletion of complement in the 38C13 model improved the efficacy of mAb therapy. Complement depletion after CVF lasted longer than that seen with HC3-1496; however, the enhanced therapeutic response was similar for both agents, suggesting prolonged depletion of complement may not be necessary to enhance the therapeutic response to mAb therapy.
Mice treated with CVF or HC3-1496 alone had slightly prolonged survival compared with untreated mice. The biologic activities of complement are complex and include effects on B-cell activation and survival.31,32 Thus, it is not possible to fully rule out a direct antitumor effect of complement depletion in the 38C13 in vivo model that is independent of mAb therapy. However, the magnitude of the antitumor activity of mAb plus complement depletion relative to that of complement depletion alone suggests the antitumor effects of mAb plus complement depletion are not simply additive.
If complement indeed limits the clinical response to mAb therapy, then the use of agents such as HC3-1496 to deplete complement before mAb therapy may enhance therapy. Alternative strategies to addressing the effect of complement include the use of complement inhibitors (as opposed to enzymatically depleting complement with CVF or HC3-1496) or the use of modified antitumor mAbs lacking complement-fixing capabilities. Each of these approaches is currently under evaluation in our laboratory, as is the assessment of the relationship between complement and NK-cell activation in patients undergoing rituximab treatment.
In summary, we previously reported that complement in serum can limit the ability of mAb-coated targets to activate NK cells. Our results here suggest that the complement present in extravascular fluid has similar effects. In addition, the ability of mAb-coated targets to activate NK cells in the presence of serum or extravascular fluid is enhanced by complement depletion. Most importantly, in vivo depletion of complement enhanced the efficacy of an antilymphoma mAb therapy in a syngeneic mouse model. These studies provide further evidence that complement fixation can impede the antitumor effects of mAbs. They also suggest that reversing the inhibitory effects of complement may be a potential approach to enhance NK cell–mediated lysis of malignant cells and improve the efficacy of mAbs. Clinical studies will need to be performed before we can fully understand how to take advantage of the complex interactions between complement and effector cell–mediated mechanisms of mAb therapy.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Brian K. Link and other members of the Weiner laboratory for helpful discussion; Laura Jacobus, Tina Knutson, and Allison Knutson for assistance in obtaining clinical samples; and Katina Wong and June Lee from the University of Hawaii for expert technical assistance.
This work was supported in part by National Institutes of Health (grant P50 CA97274), by a Translational Research Grant from the Leukemia & Lymphoma Society at the University of Iowa, and by a research grant from InCode Biopharmaceutics at the University of Hawaii.
National Institutes of Health
Authorship
Contribution: S.-Y.W. performed research, analyzed data, and wrote the manuscript; E.R. helped design research and analyzed data; J.C. and S.V. performed research; D.C.F. and C-W.V. contributed a vital reagent and designed research; W.S.J. contributed a vital reagent; and G.J.W. provided oversight of the research project, designed research, analyzed data, and wrote the manuscript.
Conflict-of-interest disclosure: W.S.J. is employed by InCode BioPharmaceutics, whose potential product was studied in the present work. W.S.J., C.-W.V. and D.C.F. have declared a financial interest in a company whose potential product was studied in the present work. G.J.W. is a consultant to InCode BioPharmaceutics, whose potential product was studied in the present work. This study was supported in part by research funding from InCode BioPharmaceutics to D.C.F. and C.-W.V. The remaining authors declare no competing financial interests.
Correspondence: George Weiner, 5970Z JPP, 200 Hawkins Dr, Iowa City, IA 52242; e-mail: george-weiner@uiowa.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal