To determine the clinical fate of patients with de novo deletion 17p13.1 (17p−) chronic lymphocytic leukemia (CLL), we retrospectively studied the outcome of 99 treatment-naive 17p− CLL patients from the M. D. Anderson Cancer Center (n = 64) and the Mayo Clinic (n = 35). Among 67 asymptomatic patients followed for progression, 53% developed CLL requiring treatment over 3 years. Patients who had not progressed by 18 months subsequently had stable disease, with 3 of 19 patients progressing after follow-up of up to 70 months. Risk factors for progressive disease were Rai stage of 1 or higher and unmutated immunoglobulin variable region heavy chain (IgVH). The overall survival rate was 65% at 3 years. Rai stage 1 or higher, unmutated IgVH, and 17p− in 25% or more of nuclei were adverse factors for survival. The 3-year survival rates of patients with 1 or fewer, 2, and 3 of these factors were 95%, 74%, and 22%, respectively (P < .001). Response rates to therapy with rituximab (n = 6); purine analogues and rituximab (n = 25); and purine analogues, rituximab, and alemtuzumab (n = 16) combinations were 50%, 72%, and 81%, respectively. Patients with 17p− CLL exhibit clinical heterogeneity, with some patients experiencing an indolent course. Survival can be predicted using clinical and biologic characteristics.
Introduction
Cytogenetic abnormalities are a major determinant of outcome in patients with chronic lymphocytic leukemia (CLL). Until recently, the study of CLL cytogenetics had been hampered by the low mitotic activity of CLL cells in vitro, with abnormal metaphases being recovered in less than one-third of patients.1 The advent of interphase fluorescent in situ hybridization (FISH) studies has shown that more than 80% of CLLs harbor recurrent genetic aberrations, and that the most common aberrations can be arranged in a hierarchical classification strongly predictive of survival.2 In this classification, patients with the chromosome 17p13.1 deletion (17p−, as identified by loss of TP53) had the worst prognosis, with a median survival of 2 to 3 years from initial diagnosis.2,3 In addition, based on experience with small groups of patients, it was suggested that 17p− CLL may be particularly resistant to treatment with purine analogues3 or rituximab.4
This reputation of 17p− CLL as a chemoresistant disease with short survival was reinforced by reports of poor overall survival (OS) in 2 large prospective studies of initial therapy in CLL. In the German CLL Study Group CLL4 trial comparing fludarabine to fludarabine plus cyclophosphamide (FC), median OS was only 16 months for the 15 patients with 17p− CLL.5 The United Kingdom Leukemia Research Foundation (LRF) CLL4 trial of chlorambucil versus fludarabine versus FC found similar results and made the observation that the dosage of 17p− may be relevant, with patients having 5% to 20% of nucleated cells with 17p− showing similar chemotherapy response rates and survival as patients without 17p−.6 In contrast, patients with 20% or more of nucleated cells with 17p− had a dismal outcome, with a response rate of 13% and a median OS of 11 months.6 More recently, an analysis of patients treated in the US Intergroup trial E2997, which compared fludarabine and FC, showed that patients with 17p− experienced a short median progression free survival (PFS) of 11 months, although the impact on OS was not reported.7
Due to these observations, it has been suggested that patients with 17p− CLL should be treated differently from other patients with CLL,8 with an emphasis on therapy using alternative agents such as alemtuzumab9 or high-dose methylprednisolone.10 However, the response rate to these agents was only 40% to 50%, with responses lasting a median of 12 months or less. Recent evidence suggests that the graft-versus-leukemia effect may be potentially curative in CLL with 17p− or other poor risk markers11,–13 leading some groups to advocate consideration of early allogeneic transplantation for such patients.8,14
Despite their importance, nearly all observations on the clinical outcome of CLL patients with 17p− have come from patients with progressive disease enrolling in first-line therapy trials. In this regard, a prospective, longitudinal study by investigators at the Mayo Clinic demonstrated that new cytogenetic abnormalities are often acquired during the course of the disease and that 17p− is frequently acquired as a secondary event.15 The clinical implications of having 17p− in this study depended on when it was identified: patients with de novo 17p− identified within 1 year of diagnosis had a median OS of 4.7 years,15 whereas those who acquired 17p− during follow-up had a median OS of 1.3 years.16 Accordingly, a better understanding of the implications of 17p− in asymptomatic, early-stage patients is needed. To evaluate the natural history of 17p− CLL in chemotherapy-naive patients, and to define their treatment outcomes after rituximab-containing therapy, we reviewed our experience with a combined cohort of de novo 17p− CLL patients recruited from 2 large academic centers.
Methods
This study was a retrospective chart review of patients with 17p− CLL diagnosed before initial therapy (“de novo 17p deletion”), to identify those patients where 17p− occurred as part of the natural history of the disease, and not due to the effects of treatment. Following approval from the relevant institutional review boards, the CLL databases at the M. D. Anderson Cancer Center (MDACC) and the Mayo Clinic were queried for the results of treatment-naive patients who had 17p− by FISH. The baseline characteristics (at the time of FISH testing), date of initial therapy, treatment response, and long-term outcome of these patients were confirmed by manual chart review and, where needed, by follow-up telephone calls. All patients had CLL as defined by the World Health Organization classification.17
At the MDACC, interphase FISH studies were performed on 200 nuclei obtained from freshly collected bone marrow samples after culturing cells for 24 hours without stimulation, using the Vysis CLL probe panel (Vysis) according to the manufacturer's recommendations. The panel includes probes specific to TP53 (17p13.1), ATM (11q22.3), D13S319 (13q14.3), LAMP1 (13q34), and the centromeric region of chromosome 12 (12p11.1-q11). At the Mayo Clinic, interphase FISH studies were performed by standard cytogenetic methods on freshly collected blood or bone marrow specimens after fixation of uncultured cells. Interphase FISH was done on 200 nuclei with a set of FISH probes designed to detect anomalies of chromosomes 6, 11, 12, 13, 14, and 17 as previously described.18 Prognostic testing performed as part of clinical or research studies, including evaluation of the immunoglobulin variable region heavy chain (IgVH) gene mutation analysis, ZAP-70 expression, and CD38 expression, was performed as previously described.15,19
Patients not meeting National Cancer Institute Working Group (NCI-WG) 1996 criteria to initiate treatment20 at the time of FISH testing were observed. Patients meeting NCI-WG criteria to initiate therapy commenced CLL therapy with the choice of a regimen at the discretion of the treating physician. CLL therapy was classified as follows: (1) rituximab-based, which included rituximab monotherapy at a standard dosage (375 mg/m2 per week),21 rituximab plus high-dose methylprednisone, and rituximab plus GMCSF22 ; (2) combinations of purine analogues and rituximab (“FCR-like” regimens), which included fludarabine, cyclophosphamide, and rituximab (FCR),23 FCR plus mitoxantrone (FCMR),24 fludarabine plus rituximab,25 pentostatin plus rituximab or pentostatin, cyclophosphamide plus rituximab (PCR)26 ; (3) a combination of FCR and alemtuzumab (CFAR)27 ; (4) alkylating-agent regimens, which included R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone), R-CVP (rituximab plus cyclophosphamide, vincristine, and prednisone), and chlorambucil; and (5) lenalidomide.28 The NCI-WG criteria20 were used to classify treatment response in patients enrolled on protocol therapy and for patients who had adequate marrow restaging. Marrow specimens were evaluated by multicolor flow cytometry and were classified as flow-cytometry negative if there were fewer than 1% CD5/19 coexpressing cells in the lymphoid gate, without evidence of light chain restriction. Several patients treated off protocol achieved complete resolution of clinical and laboratory disease manifestations but did not undergo marrow restaging, and were classified as having unconfirmed complete remissions.
Time to first therapy (TTFT) and OS were calculated from the date of the FISH documenting 17p− to the date of therapy and death, respectively. Time to progression (TTP) for patients responding to treatment was calculated from the date of therapy. Survival distributions were calculated using the method of Kaplan and Meier, and univariate comparisons were made using the log-rank test and Cox regression analysis, as appropriate. Multivariate analysis was performed with Cox regression analysis using a backward selection strategy. Categorical and continuous variables were compared using the χ2 or Fisher exact tests, or the Mann-Whitney test, as appropriate. All P values were 2-sided.
Results
Baseline characteristics
Baseline characteristics at the time of FISH testing are listed in Table 1. All patients were previously untreated at the time 17p− was documented. Sixty-four patients (64%) were from the MDACC, and 35 (35%) were from the Mayo Clinic. There were significant differences in patient characteristics between the 2 institutions, possibly reflecting differences in referral patterns. Specifically, patients from the Mayo Clinic were older (median age, 69 years vs 61 years for MDACC, P = .03), whereas patients from MDACC had more advanced disease features, including a greater proportion with performance status of 1 or more (48% vs 17% for the Mayo Clinic, P = .002), higher white cell counts (median 44 × 109/L vs 19 × 109/Ln for the Mayo Clinic, P = .002), and a greater proportion requiring therapy (72% vs 31% for the Mayo Clinic, P < .001). Patients diagnosed with asymptomatic Rai stage 0 CLL constituted 28% and 43% of the MDACC and Mayo Clinic cohorts, respectively (P = .18). The median percentage of nuclei with 17p− was 55% (range, 8%-97%), being slightly higher in the Mayo cohort than the MDACC cohort (median 64% and 46%, respectively, P = .05). Results of conventional cytogenetics were available in 61 patients, of which 24 (39%) showed rearrangements of chromosome 17, usually in the context of a complex karyotype. Median follow-up was 28 months at both institutions.
Patient characteristics at time of 17p− documentation
| Characteristic . | M. D. Anderson (n = 64) . | Mayo Clinic (n = 35) . | P . |
|---|---|---|---|
| Median survivor follow-up after 17p− documentation, mos (range) | 28 (7-60) | 28 (1-70) | NA |
| Median age, y (range) | 61 (40-84) | 69 (45-87) | .03 |
| Age ≥ 60 y, n (%) | 34 (53) | 25 (71) | NS |
| Male sex, n (%) | 39 (61) | 20 (57) | NS |
| Median months since diagnosis (range) | 9 (0–142) | 13 (0–313) | NS |
| Performance status ECOG 1 or higher, n (%) | 31 (48) | 6 (17) | .002 |
| B-symptoms, n (%) | 13 (20) | 3 (9) | NS |
| Rai stage 0, n (%) | 18 (28) | 15 (43) | NS |
| Rai stage 1 or 2, n (%) | 32 (50) | 16 (46) | NS |
| Rai stage 3 or 4, n (%) | 14 (22) | 4 (11) | NS |
| Median white cell count, ×109/L (range) | 44 (6-281) | 19 (8-150) | .002 |
| β2m ≥ 2 × upper limit of normal, n (%) | 26 (41) | 8 (40) | NS |
| Median FISH 17p deletion % (range) | 46 (8-97) | 64 (10-96) | .05 |
| FISH 17p deletion < 25%, n (%) | 21 (33) | 7 (20) | NS |
| FISH 17p deletion 25%-49%, n (%) | 11 (17) | 5 (14) | NS |
| FISH 17p deletion 50%-74%, n (%) | 10 (16) | 8 (23) | NS |
| FISH 17p deletion ≥ 75%, n (%) | 22 (34) | 15 (43) | NS |
| FISH 17p deletion only, n (%) | 25 (39) | 6 (17) | NS |
| FISH 11q deletion in addition, n (%)* | 9 (14) | 8 (23) | NS |
| FISH trisomy 12 in addition, n (%)* | 7 (11) | 3 (9) | NS |
| FISH 13q deletion in addition, n (%)* | 23 (36) | 18 (51) | NS |
| Abnormal 17p on karyotype, n (%) | 23 (40) | 1 (25) | NS |
| CD38+†, n (%) | 17 (29) | 13 (35) | NS |
| ZAP-70+†, n (%) | 19 (58) | 11 (39) | NS |
| Unmutated IgVH, n (%) | 39 (70) | 15 (57) | NS |
| Commenced CLL therapy, n (%) | 46 (72)‡ | 11 (31)‡ | <.001 |
| First CLL therapy type, n (%) | |||
| Rituximab without chemotherapy | 5 (11) | 1 (9) | NA |
| PA + rituximab based | 22 (48) | 3 (27) | NA |
| PA, alemtuzumab, + rituximab based | 14 (30) | 2 (18) | NA |
| Other | 5 (11) | 5 (45) | NA |
| Characteristic . | M. D. Anderson (n = 64) . | Mayo Clinic (n = 35) . | P . |
|---|---|---|---|
| Median survivor follow-up after 17p− documentation, mos (range) | 28 (7-60) | 28 (1-70) | NA |
| Median age, y (range) | 61 (40-84) | 69 (45-87) | .03 |
| Age ≥ 60 y, n (%) | 34 (53) | 25 (71) | NS |
| Male sex, n (%) | 39 (61) | 20 (57) | NS |
| Median months since diagnosis (range) | 9 (0–142) | 13 (0–313) | NS |
| Performance status ECOG 1 or higher, n (%) | 31 (48) | 6 (17) | .002 |
| B-symptoms, n (%) | 13 (20) | 3 (9) | NS |
| Rai stage 0, n (%) | 18 (28) | 15 (43) | NS |
| Rai stage 1 or 2, n (%) | 32 (50) | 16 (46) | NS |
| Rai stage 3 or 4, n (%) | 14 (22) | 4 (11) | NS |
| Median white cell count, ×109/L (range) | 44 (6-281) | 19 (8-150) | .002 |
| β2m ≥ 2 × upper limit of normal, n (%) | 26 (41) | 8 (40) | NS |
| Median FISH 17p deletion % (range) | 46 (8-97) | 64 (10-96) | .05 |
| FISH 17p deletion < 25%, n (%) | 21 (33) | 7 (20) | NS |
| FISH 17p deletion 25%-49%, n (%) | 11 (17) | 5 (14) | NS |
| FISH 17p deletion 50%-74%, n (%) | 10 (16) | 8 (23) | NS |
| FISH 17p deletion ≥ 75%, n (%) | 22 (34) | 15 (43) | NS |
| FISH 17p deletion only, n (%) | 25 (39) | 6 (17) | NS |
| FISH 11q deletion in addition, n (%)* | 9 (14) | 8 (23) | NS |
| FISH trisomy 12 in addition, n (%)* | 7 (11) | 3 (9) | NS |
| FISH 13q deletion in addition, n (%)* | 23 (36) | 18 (51) | NS |
| Abnormal 17p on karyotype, n (%) | 23 (40) | 1 (25) | NS |
| CD38+†, n (%) | 17 (29) | 13 (35) | NS |
| ZAP-70+†, n (%) | 19 (58) | 11 (39) | NS |
| Unmutated IgVH, n (%) | 39 (70) | 15 (57) | NS |
| Commenced CLL therapy, n (%) | 46 (72)‡ | 11 (31)‡ | <.001 |
| First CLL therapy type, n (%) | |||
| Rituximab without chemotherapy | 5 (11) | 1 (9) | NA |
| PA + rituximab based | 22 (48) | 3 (27) | NA |
| PA, alemtuzumab, + rituximab based | 14 (30) | 2 (18) | NA |
| Other | 5 (11) | 5 (45) | NA |
Percentages were calculated based on the total number of patients with evaluable information. Therapies listed under “Other” were: for M.D. Anderson, lenalidomide (n = 4), and R-CHOP (n = 1); for the Mayo Clinic, chlorambucil (n = 1), pentostatin plus cyclophosphamide (n = 1), R-CVP (n = 2) and R-CHOP (n = 1).
ECOG indicates Eastern Cooperative Oncology Group; FISH, fluorescent in situ hybridization; CLL, chronic lymphocytic leukemia; PA, purine analogue; NA, not applicable; and NS, not significant.
Patients were ranked in the hierarchical classification proposed by Dohner et al.2 For example, a patient with concomitant deletions of 11q and 13q would be classified as having 11q deletion.
Defined as ≥ 30% for CD38 and ≥ 20% for ZAP-70.
Excluding patients enrolled in early intervention trials for disease not meeting National Cancer Institute Working Group treatment criteria.
Time to first therapy
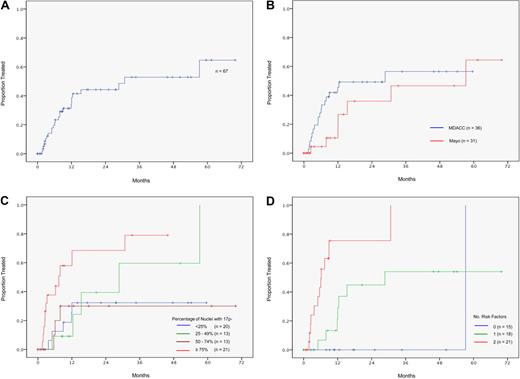
Sixty-seven asymptomatic, early-stage patients did not require immediate treatment and were assessable for time to progression requiring first therapy. Eleven patients entered clinical trials of early intervention with anti-idiotype vaccination (n = 2) or rituximab plus alemtuzumab (n = 9) without meeting NCI-WG treatment criteria and were censored on the date of trial entry. The actuarial rate of TTFT was 53% at 3 years (Figure 1A), and was similar for patients at MDACC and at the Mayo Clinic (Figure 1B). The majority of patients who progressed to first therapy did so in the first 18 months, whereas those patients who had not progressed by 18 months had relatively stable disease, with only 3 of 19 such patients subsequently progressing at a follow-up of up to 70 months.
Progression to therapy requirement for asymptomatic patients after diagnosis of 17p− CLL. (A) The 3 year progression rate to therapy requirement was 53% for the study cohort. (B) Progression to therapy requirement by institution. The 3-year progression rate to therapy requirement was 56% for patients from MDACC and 47% for patients from the Mayo Clinic (P = .17). (C) Progression to therapy requirement, effect of clone size. Patients with 75% or more nuclei with 17p− were at increased risk of progression (79% at 3 years vs 40% for the remaining patients, P = .001). (D) Model for progression to first therapy. Risk factors were Rai stage 1 or higher, and unmutated IgVH gene. Patients with 0, 1, and 2 risk factors had 3-year progression rates of 0%, 54%, and 100%, respectively (P < .001). Thirteen patients were not assessable due to missing data on IgVH status.
Progression to therapy requirement for asymptomatic patients after diagnosis of 17p− CLL. (A) The 3 year progression rate to therapy requirement was 53% for the study cohort. (B) Progression to therapy requirement by institution. The 3-year progression rate to therapy requirement was 56% for patients from MDACC and 47% for patients from the Mayo Clinic (P = .17). (C) Progression to therapy requirement, effect of clone size. Patients with 75% or more nuclei with 17p− were at increased risk of progression (79% at 3 years vs 40% for the remaining patients, P = .001). (D) Model for progression to first therapy. Risk factors were Rai stage 1 or higher, and unmutated IgVH gene. Patients with 0, 1, and 2 risk factors had 3-year progression rates of 0%, 54%, and 100%, respectively (P < .001). Thirteen patients were not assessable due to missing data on IgVH status.
Factors significantly associated with short TTFT were Rai stage 1 or higher, white cell count at least 50 × 109/L, β2m at least twice the upper limit of normal, ZAP-70 positivity, and unmutated IgVH usage (Table 2). The impact of proportion of nuclei with 17p− on TTFT was assessed by dividing patients into quartiles of less than 25%, 25% to 49%, 50% to 74%, and 75% or more 17p− nuclei (Figure 1C). In this analysis, patients with less than 75% nuclei with a 17p− had similar progression rates, whereas those with at least 75% nuclei with a 17p− experienced more rapid disease progression (3-year TTFT, 40% and 79%, respectively, P = .001). Multivariate modeling identified 2 risk factors independently associated with reduced TTFT: Rai stage 1 or higher (hazard ratio [HR], 5.6; P = .003) and unmutated IgVH gene (HR, 5.2; P = .005) (Table 2). Patients with 0, 1, and 2 risk factors had 3-year TTFT rates of 0%, 54%, and 100%, respectively (Figure 1D; P < .001).
Univariate and multivariate analyses of factors determinant of time to first therapy
| Factors associated with TTFT . | n . | Univariate 3-y TTFT % and P . | Multivariate model . |
|---|---|---|---|
| Rai stage 0 | 30 | 24 | HR 5.6 |
| Rai stage ≥ 1 | 37 | 75 (P < .001) | (P = .003) |
| White cell count < 50 × 109/L | 49 | 43 | NS |
| White cell count ≥ 50 × 109/L | 18 | 78 (P < .001) | NS |
| β2m < 2 × upper limit normal | 40 | 37 | NS |
| β2m ≥ 2 × upper limit normal | 13 | 100 (P = .002) | NS |
| FISH deletion 17p < 75% | 46 | 40 | NS |
| FISH deletion 17p ≥ 75% | 21 | 79 (P = .001) | NS |
| ZAP-70 negative | 24 | 20 | NS |
| ZAP-70 positive | 17 | 80 (P = .002) | NS |
| Mutated IgVH | 24 | 28 | HR 5.2 |
| Unmutated IgVH | 30 | 80 (P = .002) | P = .005 |
| Factors associated with TTFT . | n . | Univariate 3-y TTFT % and P . | Multivariate model . |
|---|---|---|---|
| Rai stage 0 | 30 | 24 | HR 5.6 |
| Rai stage ≥ 1 | 37 | 75 (P < .001) | (P = .003) |
| White cell count < 50 × 109/L | 49 | 43 | NS |
| White cell count ≥ 50 × 109/L | 18 | 78 (P < .001) | NS |
| β2m < 2 × upper limit normal | 40 | 37 | NS |
| β2m ≥ 2 × upper limit normal | 13 | 100 (P = .002) | NS |
| FISH deletion 17p < 75% | 46 | 40 | NS |
| FISH deletion 17p ≥ 75% | 21 | 79 (P = .001) | NS |
| ZAP-70 negative | 24 | 20 | NS |
| ZAP-70 positive | 17 | 80 (P = .002) | NS |
| Mutated IgVH | 24 | 28 | HR 5.2 |
| Unmutated IgVH | 30 | 80 (P = .002) | P = .005 |
Variables that had no significant impact on time to first therapy: institution (M. D. Anderson vs Mayo Clinic), age, sex, time from initial diagnosis, performance status, and CD38 expression.
TTFT indicates time to first therapy; FISH, fluorescent in situ hybridization; IgVH, immunoglobulin variable region heavy chain; and NS, not significant.
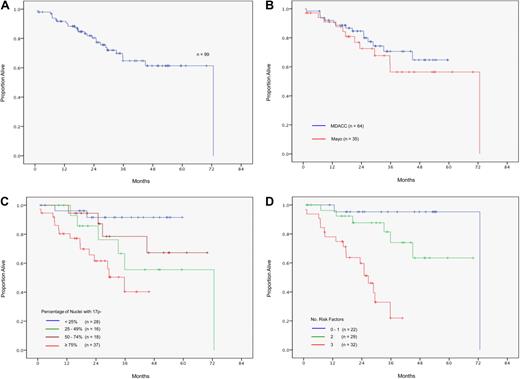
Overall survival
The rate of OS 3 years from the date of FISH documentation of 17p− was 65% (Figure 2A), and was similar for patients at MDACC and at the Mayo Clinic (Figure 2B). Factors significantly associated with reduced OS on univariate analysis were age at least 60 years, presence of B-symptoms, advanced Rai stage, white cell count at least 50 × 109/L, β2m at least twice the upper limit of normal, and unmutated IgVH gene (Table 3). The effect of increasing proportions of 17p-deleted nuclei is illustrated in Figure 2C: patients with less than 25% deleted nuclei had the most favorable outcome (3-year OS rate, 92%), patients with 25% to 74% deleted nuclei had intermediate outcomes (3-year OS rate, 67%), and patients with at least 75% deleted nuclei had the most adverse outcome (3-year OS rate, 40%, P = .001). Although several binary thresholds for the percentage of 17p-deleted nuclei were significant for inferior OS (including the 20% threshold reported by United Kingdom investigators6 ), an analysis of differing cut-points identified 25% as the most efficient cut-point in this cohort (3-year OS rate, 92% vs 54% for < 25% and ≥ 25% 17p-deleted nuclei, respectively, P = .007).
Survival after 17p− CLL diagnosis. (A) The rate of survival 3 years from the date of FISH diagnosis was 65%. (B) Survival after 17p− CLL diagnosis by institution. The rate of survival 3 years from the date of FISH diagnosis was 71% for patients from MDACC and 56% for patients from the Mayo Clinic (P = .43). (C) Survival after 17p− CLL diagnosis, effect of clone size. Survival was most favorable in patients with less than 25% deleted nuclei (3-year survival rate, 92%), intermediate in patients with 25% to 74% deleted nuclei (3-year survival rate, 67%), and least favorable in patients with 75% or more deleted nuclei (3-year survival rate, 40%; P = .001). (D) Model for survival after 17p− CLL diagnosis. Risk factors were Rai stage 1 or higher, unmutated IgVH gene, and 17p loss in ≥ 25% of nuclei. Patients with 1 or fewer, 2, and 3 risk factors had 3-year survival rates of 95%, 74%, and 22%, respectively (P < .001). Sixteen patients were not assessable due to missing data on IgVH status.
Survival after 17p− CLL diagnosis. (A) The rate of survival 3 years from the date of FISH diagnosis was 65%. (B) Survival after 17p− CLL diagnosis by institution. The rate of survival 3 years from the date of FISH diagnosis was 71% for patients from MDACC and 56% for patients from the Mayo Clinic (P = .43). (C) Survival after 17p− CLL diagnosis, effect of clone size. Survival was most favorable in patients with less than 25% deleted nuclei (3-year survival rate, 92%), intermediate in patients with 25% to 74% deleted nuclei (3-year survival rate, 67%), and least favorable in patients with 75% or more deleted nuclei (3-year survival rate, 40%; P = .001). (D) Model for survival after 17p− CLL diagnosis. Risk factors were Rai stage 1 or higher, unmutated IgVH gene, and 17p loss in ≥ 25% of nuclei. Patients with 1 or fewer, 2, and 3 risk factors had 3-year survival rates of 95%, 74%, and 22%, respectively (P < .001). Sixteen patients were not assessable due to missing data on IgVH status.
Factors associated with overall survival
| Factors associated with OS . | n . | Univariate 3-y OS % . | Multivariate model . |
|---|---|---|---|
| Age < 60 y | 40 | 77 | NS |
| Age ≥ 60 y | 59 | 58 (P = .04) | NS |
| B-symptoms absent | 83 | 68 | NS |
| B-symptoms present | 16 | 50 (P = .004) | NS |
| Rai stage 0 | 33 | 88 | |
| Rai stage 1-2 | 48 | 59 | |
| Rai stage 3-4 | 18 | 30 (P < .001) | HR 4.4 for Rai stage ≥ 1 (P = .02) |
| White cell count < 50 × 109/L | 59 | 73 | NS |
| White cell count ≥ 50 × 109/L | 40 | 53 (P = .02) | NS |
| β2m < 2 × upper limit normal | 49 | 77 | NS |
| β2m ≥ 2 × upper limit normal | 34 | 45 (P = .002) | NS |
| FISH 17p− Q1 (< 25%) | 28 | 92 | |
| FISH 17p− Q2 (25%-49%) | 16 | 56 | |
| FISH 17p− Q3 (50%-74%) | 18 | 79 | |
| FISH 17p− Q4 (≥ 75%) | 37 | 40 (P = .003) | HR 5.2 for FISH 17p− > 25% (P = .03) |
| Mutated IgVH | 29 | 89 | |
| Unmutated IgVH | 54 | 47 (P = .002) | HR 5.5 for unmutated IgVH (P = .01) |
| Factors associated with OS . | n . | Univariate 3-y OS % . | Multivariate model . |
|---|---|---|---|
| Age < 60 y | 40 | 77 | NS |
| Age ≥ 60 y | 59 | 58 (P = .04) | NS |
| B-symptoms absent | 83 | 68 | NS |
| B-symptoms present | 16 | 50 (P = .004) | NS |
| Rai stage 0 | 33 | 88 | |
| Rai stage 1-2 | 48 | 59 | |
| Rai stage 3-4 | 18 | 30 (P < .001) | HR 4.4 for Rai stage ≥ 1 (P = .02) |
| White cell count < 50 × 109/L | 59 | 73 | NS |
| White cell count ≥ 50 × 109/L | 40 | 53 (P = .02) | NS |
| β2m < 2 × upper limit normal | 49 | 77 | NS |
| β2m ≥ 2 × upper limit normal | 34 | 45 (P = .002) | NS |
| FISH 17p− Q1 (< 25%) | 28 | 92 | |
| FISH 17p− Q2 (25%-49%) | 16 | 56 | |
| FISH 17p− Q3 (50%-74%) | 18 | 79 | |
| FISH 17p− Q4 (≥ 75%) | 37 | 40 (P = .003) | HR 5.2 for FISH 17p− > 25% (P = .03) |
| Mutated IgVH | 29 | 89 | |
| Unmutated IgVH | 54 | 47 (P = .002) | HR 5.5 for unmutated IgVH (P = .01) |
Variables that had no significant impact on overall survival: institution (M. D. Anderson vs Mayo Clinic), sex, time from initial diagnosis, performance status, conventional cytogenetics, presence of other FISH abnormalities, CD38 expression, and ZAP-70 expression.
OS indicates overall survival; FISH, fluorescent in situ hybridization; HR, hazard ration; IgVH, immunoglobulin variable region heavy chain; and NS, not significant.
Multivariate analysis identified 3 risk factors independently associated with reduced OS: Rai stage 1 or higher (HR, 4.4; P = .02), 17p-deleted nuclei more than 25% (HR, 5.2; P = .03), and unmutated IgVH gene (HR, 5.5, P = .01; Table 3). These factors formed the basis for a survival model for patients with de novo 17p− CLL: patients with 0 or 1, 2, and 3 risk factors had 3-year OS rate of 95%, 74%, and 22%, respectively (P < .001; Figure 2D). Importantly, this survival model was equally applicable to patients from MDACC (P = .006) and to patients from the Mayo Clinic (P < .001).
Results of initial therapy
There were no protocols specific for the first-line treatment of symptomatic patients with 17p− CLL during the study period, and patients were treated at the discretion of the individual physician. Treatment outcome data are presented to provide some insight into how patients with 17p− CLL responded to various types of therapy, and not for the purpose of comparisons between individual regimens. Table 4 shows the response rates of 55 patients with documented treatment outcomes.
Response to initial therapy
| Treatment . | n . | CR, n (%) . | Nodular PR/unconfirmed CR, n (%) . | PR, n (%) . | Objective response, n (%) . |
|---|---|---|---|---|---|
| Purine analogue and rituximab (FCR-like) regimens* | 25 | 7 (28), 7 of 7 flow negative | 3 (12) | 8 (32) | 18 (72) |
| FCR + alemtuzumab (CFAR) | 16 | 7 (44), 5 of 6 flow negative | 1 (6) | 5 (31) | 13 (81) |
| Rituximab without chemotherapy† | 6 | 1 (17), 1 of 1 flow negative | 1 (17) | 1 (17) | 3 (50) |
| Alkylator-based regimens‡ | 4 | 0 | 0 | 1 (25) | 1 (25) |
| Lenalidomide | 4 | 0 | 0 | 1 (25) | 1 (25) |
| Treatment . | n . | CR, n (%) . | Nodular PR/unconfirmed CR, n (%) . | PR, n (%) . | Objective response, n (%) . |
|---|---|---|---|---|---|
| Purine analogue and rituximab (FCR-like) regimens* | 25 | 7 (28), 7 of 7 flow negative | 3 (12) | 8 (32) | 18 (72) |
| FCR + alemtuzumab (CFAR) | 16 | 7 (44), 5 of 6 flow negative | 1 (6) | 5 (31) | 13 (81) |
| Rituximab without chemotherapy† | 6 | 1 (17), 1 of 1 flow negative | 1 (17) | 1 (17) | 3 (50) |
| Alkylator-based regimens‡ | 4 | 0 | 0 | 1 (25) | 1 (25) |
| Lenalidomide | 4 | 0 | 0 | 1 (25) | 1 (25) |
CR indicates complete response; PR, partial response; FCR, fludarabine, cyclophosphamide, plus rituximab; flow negative, < 17 cos/19 cells in lymxxxx rate; GM-CSF, granulocyte macrophage colony-stimulating factor; R-CHOP, rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone; and R-CVP, rituximab plus cyclophosphamide, vincristine, and prednisone.
FCR (19); FCR & mitoxantrone (2); fludarabine & rituximab (1); pentostatin & rituximab (1); and pentostatin, cyclophosphamide & rituximab (2).
Rituximab (1); rituximab + GM-CSF (4); and rituximab + methylprednisolone (1).
R-CHOP (2); R-CVP (1); and chlorambucil (1).
Twenty-five patients received combination regimens containing a purine analog (either fludarabine or pentostatin) and rituximab (FCR-like regimens). The overall response (OR) rate to FCR-like regimens was 72%, with 28% complete response (CR) and 12% nodular partial response (PR) or unconfirmed CR. Sixteen patients received a combination of FCR and alemtuzumab (CFAR regimen). For these patients, the OR rate was 81%, with 44% CR and 6% nodular PR or unconfirmed CR. Six patients of an advanced age (median, 75 years) were treated with rituximab without chemotherapy. The OR rate was 50%, and this included 1 patient with CR lasting more than 36 months and 1 patient with unconfirmed CR lasting more than 55 months. Response rates to alkylating agents and lenalidomide were 25% and 25%, respectively, with no CR (Table 4). Marrow flow cytometry was performed in 14 patients who achieved a CR, and was negative in 13 (93%).
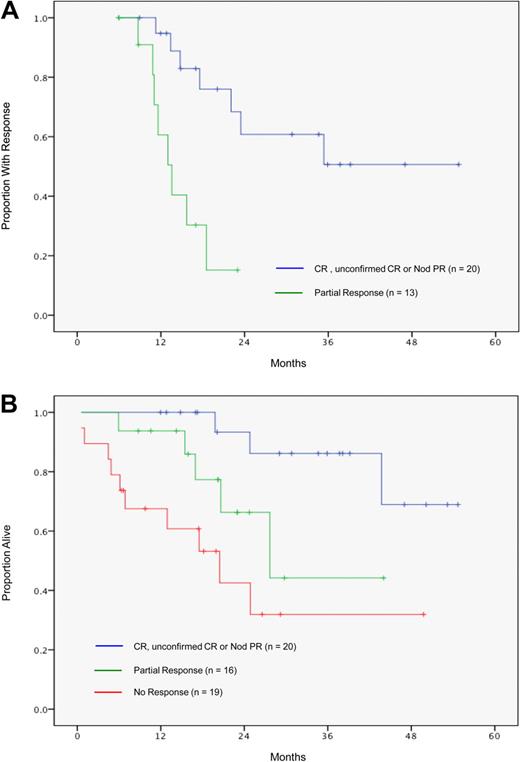
Patients with a PR had a short median TTP of 14 months (Figure 3A), whereas patients with either CR, unconfirmed CR, or nodular PR had significantly superior TTP (51% progression free at 3 years, P = .001 compared with partial responders), with no significant differences between individual major response categories (P > .30 for all comparisons). The superiority in disease control translated into an improved survival after initiation of therapy (Figure 3B): patients in CR, unconfirmed CR, or nodular PR had a favorable survival (median not reached, 3-year survival rate, 86%), whereas patients in PR had an inferior outcome (median survival, 28 months) which was not significantly better than that of nonresponders (median survival, 20 months, P = .13 vs partial responders).
Time to progression (TTP) after first therapy. (A) Patients with a complete response (CR), unconfirmed CR, or nodular partial response (Nod PR) experienced a significantly better TTP (51% at 3 years) than patients with a partial response (median TTP 14 months, P = .001 vs CR/Nod PR). Three patients with a partial response were not assessable due to inadequate follow-up of disease status. (B) Survival after first therapy. Patients with a complete response (CR), unconfirmed CR, or nodular partial response (Nod PR) experienced significantly better survival (86% at 3 years) than patients with a partial response (median survival 28 months, P = .05 vs CR/Nod PR) or patients with no response to treatment (median survival 20 months; P = .001 vs CR/Nod PR; P = .13 vs partial response).
Time to progression (TTP) after first therapy. (A) Patients with a complete response (CR), unconfirmed CR, or nodular partial response (Nod PR) experienced a significantly better TTP (51% at 3 years) than patients with a partial response (median TTP 14 months, P = .001 vs CR/Nod PR). Three patients with a partial response were not assessable due to inadequate follow-up of disease status. (B) Survival after first therapy. Patients with a complete response (CR), unconfirmed CR, or nodular partial response (Nod PR) experienced significantly better survival (86% at 3 years) than patients with a partial response (median survival 28 months, P = .05 vs CR/Nod PR) or patients with no response to treatment (median survival 20 months; P = .001 vs CR/Nod PR; P = .13 vs partial response).
Cytogenetic and FISH evolution after therapy
Repeat marrow FISH testing was performed in 13 complete responders and 2 nodular partial responders. All 15 patients were negative for 17p− at the time of response. Three patients had apparent loss of their 17p− clone at the time of disease relapse. Two patients with complex karyotypes and 9% 17p-deleted nuclei relapsed from CR with transformation to large cell lymphoma, and both patients lost their complex cytogenetic clones at the time of relapse, with one being confirmed by FISH as negative for previously observed 11q, 13q, and 17p deletions. Another patient with baseline deletions of 17p (20%), 11q (20%), and 13q (10%) relapsed from unconfirmed CR with a FISH-negative result, eventually reacquired 11q and 13q deletions on subsequent tests, but the 17p deletion was not observed in any relapse specimen.
Serial conventional cytogenetic and FISH studies were also performed in 6 patients who relapsed from a PR. In contrast to the patients who achieved major marrow responses, all partial responders had persistence of their 17p− clone at relapse.
Sole 17p deletion versus complex FISH karyotypes
Patients with sole deletion of 17p (n = 31) and patients with complex FISH karyotypes (17p deletion plus other FISH abnormalities; n = 68) were not significantly different in terms of progression rates (3-year TTFT 72% vs 49%, respectively; P = .57), initial treatment response (80% vs 57%; P = .14), or overall survival (3-year OS rate, 65% vs 64%; P = .94).
Discussion
An inherent difficulty in the study of de novo 17p− CLL is the rarity of the disease. At the 2 study institutions, where the proportion of 17p− patients may be higher than the population average due to referral bias, 17p− was found in only 5% to 7% of chemotherapy-naive patients. Despite some differences in patient characteristics (likely related to differences in referral pattern), the OS rates and the rates of progression to symptomatic disease were remarkably similar between the 2 institutions, providing evidence that the observed outcomes are likely to be representative of outcomes in patients with de novo 17p− CLL. This internal validation is important, as the results of the current study challenge several established doctrines about 17p− CLL.
The first doctrine is that 17p− CLL is a universally aggressive, poor-prognosis disease. The landmark study on FISH and CLL reported by Dohner et al2 showed that patients with 17p− CLL invariably progress to therapy requirement within 2 years, and that OS was dismal at a median of 32 months. Approximately 25% of patients in this study, however, had been pretreated and it was not known how these patients were distributed within the FISH categories. The presence of a substantial proportion of pretreated patients in the 17p− subgroup may have adversely influenced the outcome. In the current study, consisting exclusively of chemotherapy-naive patients, approximately 50% of patients developed progressive disease requiring therapy within 12 to 18 months, whereas the remaining half had relatively stable disease extending out to 70 months of follow-up. No patient with 17p− CLL and the favorable characteristics of Rai stage 0 and a mutated IgVH gene progressed or died at 3 years of follow-up. The findings of the present study are consistent with prior work from the Mayo Clinic demonstrating a median OS of 4.7 years among patients with a de novo 17p− identified within 1 year of diagnosis,16 and with anecdotal reports of early stage CLL patients with p53 abnormalities surviving for 10 years or more.29 A commonly held assumption is that the adverse prognosis of 17p− is related to its effects on the p53 pathway. It would therefore be of great interest to determine whether those patients with apparently benign disease were those with a nonmutated p53 allele, or preserved p53 function.29 However, in this retrospective study the absence of suitable patient material precluded these investigations. The clinical outcome of asymptomatic, early-stage patients with 17p− CLL is heterogeneous and such patients should not be managed differently from other patients with CLL solely because of their chromosomal abnormality, without accounting for other risk factors. In particular, we caution against the use of early allogeneic transplantation in de novo 17p− CLL in the absence of other clinical indications. Consistent with this recommendation, the current European Group for Bone Marrow Transplantation (EBMT) guidelines for allogeneic transplant suggest allogeneic transplantation for CLL patients with 17p− only if their disease has progressed to the point of requiring treatment.14
A second observation from the current study is that the response to purine nucleoside analog–based therapy was reasonable, and not as poor as suggested by recent German and United Kingdom trials.5,6 In the current study, OR rates greater than 70% were achieved with FCR-like therapies and CFAR, with CR in 28% and 44%, respectively. Achievement of a complete marrow response was associated with elimination of disease as detected by flow cytometry in some patients, and normalized cytogenetics and FISH. However, the flow cytometry method used in this study was of lower sensitivity than recent high-resolution techniques,30 and whether minimal residual disease was truly eradicated or not in our patients cannot be determined from the current data. Patients with complete (or near complete) responses experienced reasonably durable remissions, and had a favorable 3-year posttreatment OS rate of 86%. These outcomes, while inferior to those expected with FCR therapy in unselected patients,31 were nevertheless superior to the results reported for single agent alemtuzumab or high-dose methylprednisolone.9,10,32,–34 In addition, the observation of significant responses in some patients receiving single-agent rituximab suggests that rituximab may be a key component of therapy for patients with 17p− CLL. Further support for the use of rituximab emerged from the German CLL8 study comparing FC versus FCR,35 where CR rates were numerically higher in the small number of 17p− patients receiving FCR (19%) compared with patients receiving FC (4.5%), although the difference did not reach statistical significance (P = .185). The CLL8 study showed that patients with 17p− CLL treated with FCR had a poor progression-free survival of 12 months, underscoring the need for strategies to increase the proportion of patients reaching CR. The most effective approach to the first-line therapy of patients with 17p− CLL may therefore be induction with FCR or a related regimen, followed by postinduction maneuvers (such as alemtuzumab36 ) to consolidate responses. Whether allogeneic transplantation is required at the achievement of first CR, or whether it can be reserved until the time of early relapse, should be the subject of a systematic study.
Finally, our study provides evidence that 17p− may not be a primary pathogenic event, but may be a secondary genetic lesion that develops within a disease subclone. Whereas all patients who progressed from PR had persistence of 17p− by FISH, 3 patients who relapsed from CR had apparent disappearance of their original 17p− disease clone. In 2 cases, the relapse was aggressive transformation to large cell lymphoma, and in 1 case the relapse was with CLL that was initially negative for all FISH aberrations present at baseline, but then later reacquired 13q− and 11q− without 17p−. These cases suggested that the 17p− subclone may be suppressed (or even eradicated) by effective therapy. Deletion of 17p13.1 may simply be a marker for a cell with an unstable genome prone to new genetic lesions and clonal evolution.15 Studies of serial karyotypic and FISH studies are ongoing at our centers to provide insight into the evolution of the 17p13.1 deletion and other genomic aberrations in patients with CLL.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgment
The authors acknowledge the contribution of Gregory Jenkins in data collection and statistical assistance.
Authorship
Contribution: C.S.T. and T.D.S. designed the study, analyzed the data, and wrote the paper; M.J.K. and N.E.K. designed the study and provided supervision and advice in data analysis and manuscript preparation; L.V.A. and D.L.V.D. supervised the conventional cytogenetic and FISH testing and provided advice and oversight in manuscript preparation; S.O. contributed to the design of the study, verified the accuracy of patient data, and provided advice on statistical analysis; W.W. and A.F. contributed and verified the accuracy of patient data and provided advice and oversight in manuscript preparation; and S.L. and A.L. collected the patient data and coordinated the verification of data integrity.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Michael J. Keating, Department of Leukemia, Unit 428, The University of Texas M. D. Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX 77030; e-mail: mkeating@mdanderson.org.