With great interest we read the letter by Elmaagacli and coworkers who report the results of their retrospective study to investigate the impact of a donor LCT-13910 single nucleotide polymorphism (SNP) on the outcome of allogeneic hematopoietic stem cell transplantation (HSCT). They found no correlation between the presence of a LCT-13910 CC genotype and relapse rate or overall survival and only a nonsignificant reduction in the rate of transplantation-related mortality (TRM). We have recently reported the results of a retrospective study on the impact of the LCT-13910 SNP on the outcome of 111 consecutive patients who underwent allogeneic HSCT at our institution.1 We found that the presence of a CC genotype in donors was associated with a significantly better overall survival due to less TRM and a lower relapse rate in our patients.
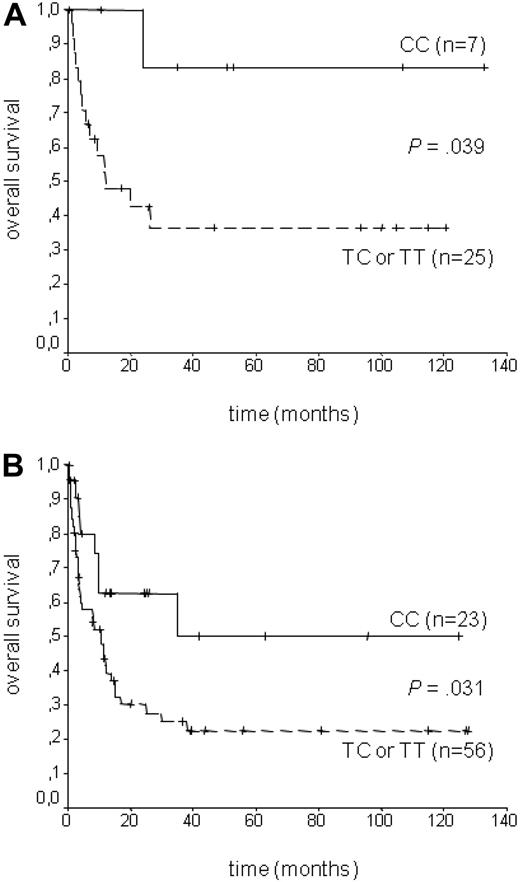
The authors discussed the possibility that our results might be caused by a more heterogeneous study population with regard to type of donor (HLA-identical sibling donors, mismatched donors, unrelated donors), type of disease, and the use of myeloablative as well as nonmyeloablative conditioning regimen. We have addressed this issue in the supplemental data of our paper,1 where we saw a survival advantage with CC donors in all subgroups analyzed. However, we looked at our data again and restricted analyses to the same patient population as used by Elmaagacli et al. Our published data contained 32 acute myeloid leukemia (AML) patients who received transplantations without T-cell depletion from HLA-identical sibling donors after myeloablative conditioning (subgroup 1). Even in this small subgroup we still found a significant survival advantage for patients receiving transplantations from a CC donor (log-rank P = .039; Breslow P = .035, Figure 1A), which was also true for all remaining patients (log-rank P = .031; Breslow P = .038; subgroup 2, Figure 1B). In subgroup 1, estimated cumulative survival was 83.3 months with a CC donor versus 36.5 months compared with patients whose donor carried a T-allele. Sixty-two and a half percent of patients received transplantation in first complete remission and 37.5% in more advanced disease. Graft-versus-host disease prophylaxis was cyclosporine and methotrexate in all patients.
Overall survival according to LCT genotype. The impact of the donor LCT-13910C > T polymorphism is not dependent on diagnosis, myeloablative conditioning, or type of donor. It is seen in AML patients who received a transplantation after myeloablative conditioning from HLA-identical sibling donors (A), as well as in all other patients (B).
Overall survival according to LCT genotype. The impact of the donor LCT-13910C > T polymorphism is not dependent on diagnosis, myeloablative conditioning, or type of donor. It is seen in AML patients who received a transplantation after myeloablative conditioning from HLA-identical sibling donors (A), as well as in all other patients (B).
However, the use and method of conditioning regimen was noticeably different (P < .001), as we used busulfan and cyclophosphamide (BU/CY) in 30 patients (93.8%) versus total body irradiation and cyclophosphamide (TBI/CY) in only 2 patients (6.2%). A recent meta-analysis clearly confirmed different effects of TBI versus busulfan-based regimen on overall survival, nonrelapse mortality, and side effects.2 With regard to role of SNPs on the outcome of allogeneic HSCT, even minor differences in clinical protocols can have a profound influence on results, as has been convincingly proposed for polymorphism of the NOD2/CARD2 gene by Elmaagacli3 and others4 before. Because allogeneic HSCT is a complex clinical procedure with little standardization between individual centers, it seems almost impossible to pinpoint a reason for the differing results of 2 retrospective single-center studies.
We appreciate this single-center analysis by Elmaagacli et al and are eagerly awaiting results from other centers.
Authorship
Contribution: H.H. wrote the manuscript, performed statistical analyses, and interpreted data; O.Z. performed polymerase chain reactions; O.K., H.K., J.K. and M.G. treated patients and collected clinical data; and D.L. supervised the project and reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Hanns Hauser, 1st Department of Internal Medicine, Elisabethinen Hospital, Fadingerstr 1, A-4020 Linz, Austria; e-mail: hanns.hauser@elisabethinen.or.at.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal