Abstract
Abstract 364
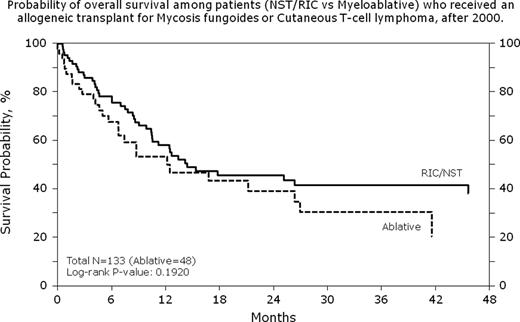
Patients (pts) with advanced stage CTCL have a poor prognosis with standard therapy whereas AHCT possibly is curative. Published experience with AHCT for CTCL is modest. We report the outcomes of a large cohort of CTCL pts receiving AHCT (N=133) reported to the CIBMTR from 2000–2009. The majority of pts 129 (97%) were diagnosed with Mycosis Fungoides or Sezary Syndrome. Only 8 (6%) received AHCT in a complete remission (CR) while 46 pts (35%) never achieved CR pre-AHCT. Most pts (83%) were transplanted beyond 12 months from diagnosis. Median (range) time from diagnosis to transplant is 29 (4-206) months. Peripheral blood was the main graft source (83% vs. 14% marrow and 3% cord blood). Donor types included: 66 HLA-identical siblings (50%), 56 unrelated donors (42%), 11 from other related donors (8%). Reduced intensity conditioning (RIC) was used in 64%. Recipients of RIC were on average older (median age 51 vs. 44 yr for myeloablative) and transplanted in later study years. Among the myeloablative regimens, cyclophosphamide with total body irradiation was the most common (38%) whereas among RIC, fludarabine in combination with busulfan, cyclophosphamide or melphalan was used in 50%. GVHD prophylaxis regimens varied. Overall mortality at 30 and 100 days was 7% and 16%, respectively. Overall survival at 6 mo and 2 yr was 75% (95% CI 67–82%) and 44% (95% CI 34–53%), respectively. Conditioning intensity was not different statistically for the overall survival of these pts (figure 1). Treatment related mortality (TRM) at 6 mo and 2 yr was 10% (95% CI 5–17%). Progression/relapse of CTCL was 44% (95% CI 34–54%) at 6 mo and 58% (95% CI 47–68%) at 2 yr. Progression free survival at 6 mo was 46% (95% CI 36–57%) and at 2 yr 32% (95% CI 23–42%). The incidence of grade II-IV acute GVHD was 36% (95% CI 22–50%) and of chronic GVHD 31% (95% CI 19–45%) in a subset of reported pts. Infection as a cause of death does not seem to be increased in CTCL transplanted pts. Conditioning intensity did not impact TRM or the risk of progression. This very large series of allogeneic HCT demonstrates feasibility in pts with advanced CTCL with a low TRM and long term progression free survival in approximately one third of pts. Progressive disease was the primary cause of treatment failure in this cohort of pts with advanced disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal