Abstract
Abstract 888
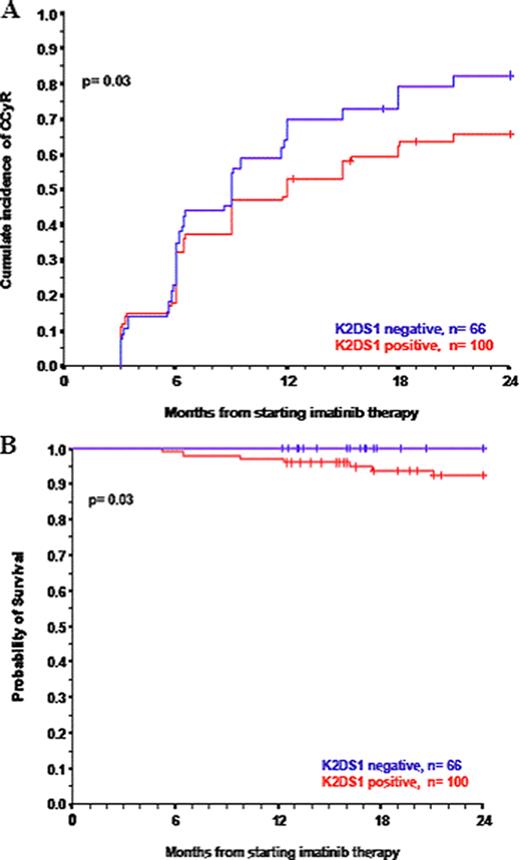
Natural killer (NK) cells are expanded in patients with chronic myeloid leukemia (CML) on tyrosine kinase inhibitors (TKI) and exert cytotoxicity against CML cells. NK cytotoxicity is determined by the balance between inhibitory and activating signals from cell surface killer immunoglobulin-like receptors (KIRs). The inherited repertoire of KIR genes may therefore influence susceptibility to treatment and prognosis in CML patients treated with TKI. To determine if innate immunity is associated with CML susceptibility and response to TKI, we investigated the impact of KIR genotype on the outcome of 166 consecutive patients with Philadelphia+ CML in chronic phase (CP) who received imatinib as first line treatment in our institution. The median follow up was 36 months and 75% of the patients were followed for a minimum of 24 months. One hundred and nineteen patients (71.7%) achieved CCyR, 10 (6.0%) progressed to advanced phase disease and 7 (4.2%) died. The 2-year cumulative incidence of CCyR was 72.2% and the 2 year probability of PFS and OS were 95.7% and 97.3% respectively. The presence of 2 KIR genes, namely K2DL5A and KIR2DS1, was associated with a significantly lower 2 year probability of CCyR (78.8% vs 63.2%, p=0.04 and 82.3% and 65.6%, p=0.03) respectively, PFS (98.9% vs 91.5%, p=0.02 and 98.4% vs 91.0%, p=0.01 respectively) and OS (100% vs 93.9%, p=0.02 and 100% vs 92.6% p=0.03 respectively). On multivariate analysis, the presence of KIR2DS1 (RR=0.66, p=0.03) and Sokal risk score (low risk RR=1, intermediate risk RR= 0.65, p= 0.04 and high risk RR= 0.59, p=0.034) were the only independent predictors for the achievement of CCyR. Furthermore, on multivariate analysis, the presence of KIR2DS1 was the only independent predictor for both PFS (P=0.02) and OS (P=0.03). In order to validate our results we explored the influence of the KIR genotype on achievement of CCyR and PFS and OS in a second independent patient group: KIR genotype was determined in 174 patients with CML-CP treated with first line imatinib within the multi-center STI571 Prospective International Randomised Trial (SPIRIT). The 65 patients who were KIR2DL5A positive had a significantly lower 2 year probability of achieving CCyR, PFS and OS than the 106 patients who were negative for this gene, namely 80.4% vs 86.8 (p=0.04), 85.7% vs 98.1% (p=0.01) and 94.3% vs 100% (p=0.02) respectively. Similarly, the 66 patients who were KIR2DS1 positive had a lower probability of achieving CCyR and lower PFS and OS than the 106 patients who did not have the gene (76.9% vs 87.9%, p=0.004, 85.3% vs 98.1% p=0.01 and 94.4% vs 100%, p=0.02 respectively). On multivariate analysis of this patient cohort KIR2DS1 remained the only independent predictor for the three outcomes. When patients were categorized based on their Sokal risk score and KIR2DS1 genotype, the most significant difference in CCyR, PFS and OS was observed in the 77 patients who had a high Sokal risk score and those with an intermediate Sokal risk score who were KIR2DS1 positive compared to the 89 patients who had a low Sokal risk score and those with an intermediate Sokal risk score who were KIR2DS1 negative; namely, 82.4% vs 59.3% (p=0.002), 92.1% vs 98.8% (p=0.03) and 94.2% vs 100% (p=0.03) and respectively (Figure 1). The mechanism by which KIR2DS1 predicts for a sub-optimal response to therapy is unknown. KIR2DS1+ve NK cells have been shown to secrete transforming growth factor-beta (TGF-beta) upon interaction with their ligand. TGF-b was recently shown to inhibit Akt signalling, a suppressor of the forkhead O transcription factor, FOXO3a, in the CML leukaemia-initiating cells (LICs) and may represent an important mechanism for the CML LIC to survive imatinib. Alternatively, KIR2DS1 may be simply a surrogate marker for another neighboring gene that is directly involved in pathogenesis of CML. In conclusion, our data demonstrate that KIR immunogenetics represent a novel prognostic tool for patients with CML-CP on TKI, and that KIR2DS1 positivity may predict response to imatinib and identify patients at greater risk of treatment failure. Functional and phenotypic studies to determine the expression of KIR2DS1 on the surface of NK cells and to assess the role of the cytokine milieu and the NK phenotype on outcome are currently underway.
CCyR and OS according to the expression of K2DS1 genotype and Sokal score
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal