In this issue of Blood, Balusu and collegues provide preclinical evidences that targeting nucleophosmin (NPM1) induces differentiation and death of acute myeloid leukemia (AML) cells harboring NPM1 mutations.1 These findings establish the rationale for novel treatment strategies in this large subgroup of AML.
NPM1 is one of the most abundant proteins in the nucleolus. Despite its nucleolar localization, NPM1 physiologically shuttles constantly across various cell compartments (nucleolus, nucleoplasm, cytoplasm) and this traffic is critical for most of its functions, including regulation of ribosome biogenesis and control of centrosome duplication.2 NPM1 also interacts with the tumor suppressor p14ARF and p53, and influences the cellular apoptotic response, although its exact role in this pathway still remains poorly understood.2
Mutations involving the NPM1 gene are the most frequent molecular alteration in AML with normal karyotype, accounting for ∼ 60% of cases (ie, one-third of adult AML).3 As a consequence of these mutations, the NPM1 mutant intracellular traffic is altered leading to its aberrant accumulation in the cytoplasm of leukemic cells.4 Through formation of heterodimers with the wild-type NPM1 protein, the leukemic mutants also dislocate the normal nucleophosmin in the cytoplasm (see figure).4
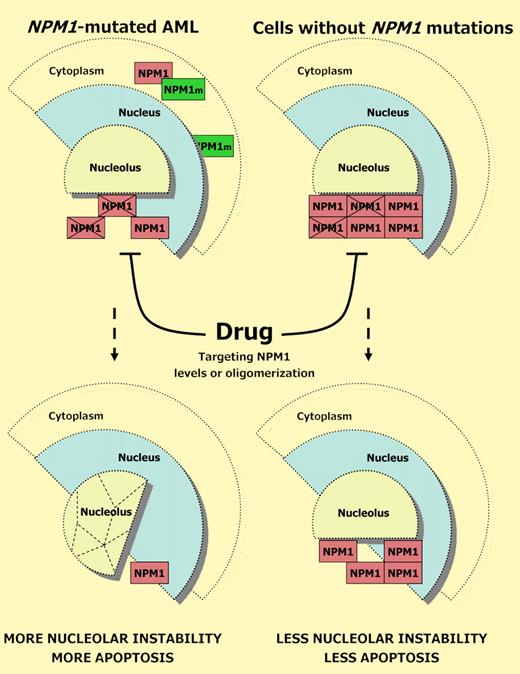
Potential strategy for targeting leukemic cells harboring NPM1 mutations. NPM1 is one of the most abundant nucleolar protein. NPM1-mutated AML cells are depleted of normal NPM1 (red blocks) in the nucleolus because of both haploinsufficiency and cytoplasmic dislocation (through formation of heterodimers with NPM1 mutant; NPM1m, green blocks). This may explain why they are more sensitive than cells with germ line NPM1 (containing full dose of wild-type NPM1) to drugs that, affecting NPM1 levels or oligomerization lead to disruption of the nucleolar structure and apoptosis.
Potential strategy for targeting leukemic cells harboring NPM1 mutations. NPM1 is one of the most abundant nucleolar protein. NPM1-mutated AML cells are depleted of normal NPM1 (red blocks) in the nucleolus because of both haploinsufficiency and cytoplasmic dislocation (through formation of heterodimers with NPM1 mutant; NPM1m, green blocks). This may explain why they are more sensitive than cells with germ line NPM1 (containing full dose of wild-type NPM1) to drugs that, affecting NPM1 levels or oligomerization lead to disruption of the nucleolar structure and apoptosis.
Because of its distinctive molecular, pathologic, and clinical characteristics,5 NPM1-mutated AML has been included as a provisional entity in the 2008 World Health Organization classification of lympho-hemopoietic neoplasms. AML with mutated NPM1 is generally characterized by good response to induction chemotherapy3 and favorable prognosis (in the absence of a concomitant FLT3-ITD mutation).5 However, a significant number of cases with NPM1-mutated AML still show poor outcome, especially those associated with FLT3-ITD mutation and elderly patients. Therefore, there is the need for exploring new treatment strategies.
Intervening on the abnormal traffic of the NPM1 mutant appears a difficult task.4 A more concrete possibility in NPM1-mutated AML is to interfere with the function of residual wild-type NPM1 encoded by the normal allele. NPM1 mutations in AML are always heterozygous,5 thus NPM1-mutated AML retains in the nucleolus a certain amount of wild-type NPM1 protein.4 This finding and the observation that complete deletion of NPM1 gene in knockout mice leads to death during embryogenesis2 strongly suggests that maintaining wild-type NPM1 in the nucleolus may be required for leukemic cell survival.4,6 Therefore, there is a rationale for interfering with wild-type NPM1 to enhance the propensity of NPM1-mutated AML cells to die or to be killed by chemotherapeutic drugs.6 Balusu et al explore this interesting issue.
Using the human Ontario Cancer Institute (OCI)/AML3 cell line (known to harbor NPM1 gene mutation), the authors show that knocking down NPM1 induced differentiation, growth inhibition, and increased apoptosis more specifically in NPM1-mutated AML cells than in other cell lines not carrying the NPM1 mutation. These events were associated with activation of the p53 tumor suppressor pathway and down-regulation of HOXA9 and Meis1 genes, which are known to be up-regulated in NPM1-mutated AML5 and likely contribute to leukemogenesis. Knockdown of NPM1 also abolished lethal AML phenotype induced by OCI-AML3 cells in the immunocompromised NOD/SCID mice.1
Balusu et al also provide evidence that down-regulation of NPM1 acts in synergy with other drugs, such as all-trans-retinoic acid (ATRA) and cytarabine, in inducing cell apoptosis.1 Interestingly, ATRA itself was previously reported to induce in vitro apoptosis in NPM1-mutated AML cells in association with down-regulation of NPM1 mutant protein.7 However, it remains uncertain whether the addition of ATRA to induction chemotherapy improves survival in NPM1-mutated AML patients.
Balusu and colleagues also explored the effects of a small molecule (NSC348884) that is able to interfere with NPM1 oligomerization. They showed that inhibition of the NPM1-NPM1 interaction induced apoptosis and sensitized OCI-AML3 and primary NPM1-mutated AML cells to ATRA without affecting NPM1 protein levels. By contrast, AML or normal CD34+ progenitor cells not carrying NPM1 mutation were relatively unaffected.
The underlying mechanisms of these pharmacologic effects are still unknown. Interfering with the levels or the oligomerization status of NPM1 may influence its capability to properly build up the nucleolus in NPM1-mutated AML cells (see figure). This feature is related to the fact that wild-type NPM1 (and other proteins, such as nucleolin) act as “hub” proteins (ie, capable to interact with many other proteins) that serve as building blocks for nucleolar assembly.8 Interestingly, ablation of either NPM1 or nucleolin by RNA interference is sufficient to disrupt the nucleolar structure.9 Similarly, the anticancer peptide CIGB-300 leads to nucleolar disassembly and apoptosis, most likely through its capability to bind NPM1.10
Because AML cells carrying the NPM1 mutation are depleted of wild-type NPM1 protein in their nucleolar pool (because of haploinsufficiency and cytoplasmic dislocation through formation of heterodimers with the mutant), they are more sensitive than cells with germ line NPM1 gene (containing a full dose of wild-type NPM1) to drugs that affect the levels and oligomerization status of NPM1 and lead to disruption of the nucleolar structure (see figure).6 Thus, tuning the dose of these drugs could become a strategy for targeting leukemic cells harboring NPM1 mutations more selectively than other leukemic or normal cells.
Conflict-of-interest disclosure: B.F. applied for a patent on the clinical use of NPM1 mutants. M.P.M. declares no competing financial interests. ■