Abstract
Abstract 2521
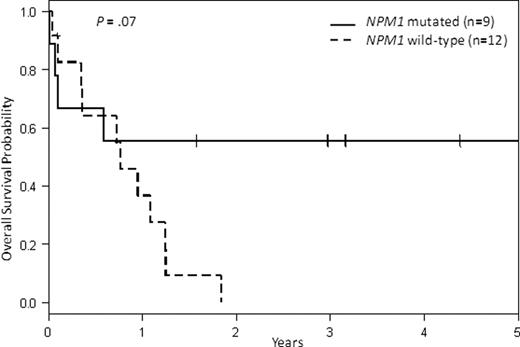
We asked whether a modified European LeukemiaNet (ELN) karyotype-based classification without molecular markers has prognostic significance in AML pts aged 80 to 89 years (y). We queried the German-Austrian AML Study Group (AMLSG; 7 pts), the Acute Leukemia French Association Group (ALFA; 17 pts), the German AML Cooperative Group (AMLCG; 35 pts) and the Cancer and Leukemia Group B (CALGB; 81 pts) for pts treated with intensive induction (7+3 or similar) on whom conventional karyotype analyses were completed and reviewed centrally. Of the 140 pts, including 82 (59%) men and 58 (41%) women, with a median age of 82 y (range, 80–89), 117 pts had de novo and 23 had secondary or therapy-related AML (s-AML/t-AML). There were 2 pts in the modified Favorable Group [t(8;21) and inv(16)], 67 pts in the modified Intermediate I Group [cytogenetically normal (CN-AML) pts], 44 pts in the ELN Intermediate II Group [t(9;11) and abnormalities (abn) classified as neither favorable nor adverse] and 27 pts in the ELN Adverse Group [inv(3) or t(3;3), t(6;9), t(v;11)(v;q23), -5 or del(5q), -7, abn(17p) and complex karyotype (≥3 abn)]. In order to assess the impact of karyotype on outcome, we eliminated early deaths. The complete remission (CR) rate for all 92 (66%) pts surviving beyond 30 days (d) was 46% and their median disease-free survival (DFS) was 6 months (mo); 35% were disease-free at 1 y and 12% at 3 y. Similarly, the median overall survival (OS) for pts surviving beyond 30 d was 6 mo, with 35% alive at 1 y and 11% at 3 y. There was no difference in DFS or OS based on AML type (de novo v s-AML/t-AML; Table 1). As shown in Table 2, pts in the modified Intermediate I Group had better OS than pts in the Adverse Group (P=0.03). Among CN-AML pts with molecular testing completed, 9/21 (43%) were NPM1-mutated (mut), 8/25 (32%) had FLT3-internal tandem duplication (ITD) and 1/12 (8%) was CEBPA-mut. Interestingly, FLT3-ITD did not have prognostic significance in the CN-AML cohort alive beyond 30 d (data not shown), but NPM1 mutation resulted in trends for higher CR rates (67% v 25%, P=.09) and longer OS (91 v 10 mo, P=0.07) in the CN-AML cohort alive beyond 30 d (Figure). Of note, there was no difference between the 2 larger cohorts (AMLCG and CALGB) in regards to pt characteristics or outcome in de novo pts; there were insufficient numbers of pts with s-AML/t-AML to compare the 2 cohorts. We conclude that there is a difference in accrual to clinical trials of octogenarian AML pts among the different cooperative groups. Further, CN-AML pts had better OS in octogenarian AML, and NPM1 mutation may be of prognostic significance among the CN-AML pts.
Table 1:
Treatment outcome by disease presentation for 92 pts alive beyond 30 d
| End Point . | de novo AML (n = 78) . | s-AML/t-AML (n = 14) . | All pts (n = 92) . | P de novo v s-AML/t-AML . |
|---|---|---|---|---|
| CR, no. (%) | 35 (45) | 7 (50) | 42 (46) | .78 |
| DFS | .76 | |||
| Median, y | 0.5 | 0.6 | 0.5 | .27 |
| % Disease-free at 1 y | 36 (26–51) | 29 (4–61) | 35 (21–49) | |
| % Disease-free at 3 y | 14 (5–29) | 0 | 12 (4–24) | |
| OS | ||||
| Median, y | 0.5 | 0.6 | 0.5 | |
| % Alive at 1 y | 35 (24–46) | 36 (13–59) | 35 (25–45) | |
| % Alive at 3 y | 14 (6–23) | 0 | 11 (5–19) |
| End Point . | de novo AML (n = 78) . | s-AML/t-AML (n = 14) . | All pts (n = 92) . | P de novo v s-AML/t-AML . |
|---|---|---|---|---|
| CR, no. (%) | 35 (45) | 7 (50) | 42 (46) | .78 |
| DFS | .76 | |||
| Median, y | 0.5 | 0.6 | 0.5 | .27 |
| % Disease-free at 1 y | 36 (26–51) | 29 (4–61) | 35 (21–49) | |
| % Disease-free at 3 y | 14 (5–29) | 0 | 12 (4–24) | |
| OS | ||||
| Median, y | 0.5 | 0.6 | 0.5 | |
| % Alive at 1 y | 35 (24–46) | 36 (13–59) | 35 (25–45) | |
| % Alive at 3 y | 14 (6–23) | 0 | 11 (5–19) |
Table 2:
Disease outcome by ELN karyotype-based classification without molecular markers for 92 pts alive beyond 30 d
| End Point . | Intermediate I (n = 43) . | Intermediate II (n = 29) . | Adverse (n = 20) . | P . |
|---|---|---|---|---|
| CR, no. (%) | 23 (53) | 13 (45) | 6 (30) | .23 |
| DFS | .17* | |||
| Median, y | 0.6 | 0.4 | 0.3 | |
| % Disease-free at 1 y | 36 (17–56) | 40 (16–63) | 17 (1–52) | |
| % Disease-free at 3 y | 23 (8–41) | 0 | 0 | |
| OS | .03† | |||
| Median, y | 0.9 | 0.4 | 0.3 | |
| % Alive at 1 y | 43 (28–57) | 33 (16–50) | 21 (7–41) | |
| % Alive at 3 y | 17 (8–31) | 5 (0–20) | 5 (0–22) |
| End Point . | Intermediate I (n = 43) . | Intermediate II (n = 29) . | Adverse (n = 20) . | P . |
|---|---|---|---|---|
| CR, no. (%) | 23 (53) | 13 (45) | 6 (30) | .23 |
| DFS | .17* | |||
| Median, y | 0.6 | 0.4 | 0.3 | |
| % Disease-free at 1 y | 36 (17–56) | 40 (16–63) | 17 (1–52) | |
| % Disease-free at 3 y | 23 (8–41) | 0 | 0 | |
| OS | .03† | |||
| Median, y | 0.9 | 0.4 | 0.3 | |
| % Alive at 1 y | 43 (28–57) | 33 (16–50) | 21 (7–41) | |
| % Alive at 3 y | 17 (8–31) | 5 (0–20) | 5 (0–22) |
*
Only Intermediate I compared to Intermediate II (too few pts in the Adverse Group)
†
This is overall P-value. Adjusted P-values were not significant for the differences between Intermediate-I and Intermediate-II Groups (P=.26) and between Intermediate-II and Adverse Groups (P=.87). There was a statistically significant difference between Intermediate-I and Adverse Groups (P=.03)
Disclosures:
Krug:MedA Pharma: Honoraria; Novartis: Honoraria; Alexion: Honoraria; Boehringer Ingelheim: Research Funding; Sunesis: Honoraria.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal