Abstract
Abstract 3098
Upfront treatment for advanced Hodgkin lymphoma (HL) is a matter of debate. The wide difference in progression-free survival (PFS) or freedom from treatment failure observed between the intensified regimen escalated (esc) BEACOPP and other standard intensity schedules - such us ABVD, ABVD hybrids and BEACOPP baseline - is in contrast with a small difference in overall survival (OS) [NEJM 2011;365 :203 and JCO 2009;27 :4548]. This fact suggests that high-dose therapy with autologous stem-cell transplantation (HDT/ASCT) can salvage more patients treated with standard intensity schedules than escBEACOPP treated patients.
In order to better understand this subject we analyzed all Swiss cases of refractory/relapsed HL that received HDT/ASCT after failure of at least 4 cycles of upfront escBEACOPP (4 to 8 cycles), given alone or combined with other regimens (cases, n=22) and compared outcomes with a control group of 33 patients transplanted after failure of upfront ABVD (N=18), ABDV-based combinations (hybrids, N=7), BEACOPP baseline (N=5) or up to 3 cycles of escBEACOPP plus radiotherapy (N=3). The high-dose schedule used before transplant was BEAM for 51/55 patients and CBV in 1 case and 3 controls.
Controls and cases were statistically similar in terms of timing of transplant (median year 2006 vs 2007), age at transplant (median 33 vs 28 years), sex (males 64% vs 68%), HL subtype, Ann Arbor stage, international prognostic score, ESR (38 vs 59 mm/1h) and bulky presentation (35% vs 60%), but there were significantly more B-symptoms among escBEACOPP patients (77% vs 23%, p=0.007). Furthermore, chemosensitivity (94% vs 82%), timing of relapse after upfront treatment (0–3 months: 30% vs 22%, 3–12 months: 18% vs 23% and >12 months: 52% vs 55%), median number of CD34+ cells reinfused (4.11 vs 2.99 ×10*6/kg), and need for a second salvage (12% vs 27%) were not significantly different in the two groups.
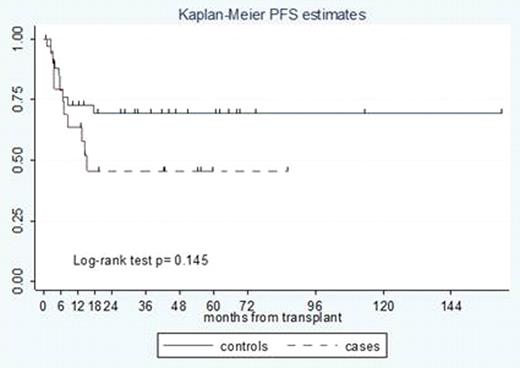
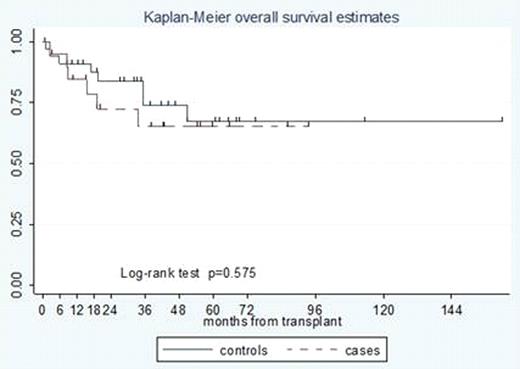
After a median post transplant follow up of 42.5 months, median PFS was 15.4 months for escBEACOPP, and was not reached for control cases (p=0.145). Two-years OS was 84% for controls (95% CI 65%-93%) and 72% for escBEACOPP (95% CI 45%-87%), while 5-years OS was 68% (95% CI 44%-84%) and 65% (95% CI 37%-83%) for controls and cases, respectively. Four of 33 controls (12%) and 3 of 22 (14%) upfront escBEACOPP cases received an allograft for relapsed HL after HDT/ASCT (p=NS). The incidence of severe (grade 3–4) anemia, thrombocytopenia, neutropenia, diarrhea, stomatitis and neutropenic fever was similar in the two groups. Regarding uncommon/unexpected toxicities of HDT/ASCT, one patient in the escBEACOPP group developed grade 4 encephalopathy, whilst in the control group we observed two cases of acute renal failure, one ARDS and one fatal stroke. One patient in the control group was diagnosed with a T-cell lymphoma after transplant (p=NS). Three t-MDS plus one t-AML were recorded among patients in the escBEACOPP group, with no cases of t-AML/t-MDS occurring among those treated with the less intensive approaches (p=0.023).
In our series, overall survival of chemosensitive HL patients autografted after failure of either upfront escBEACOPP or standard intensity regimens is encouraging. HDT/ASCT consolidation of chemosensitive patients failing upfront escBEACOPP seems justified.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal