Abstract
Abstract 4065
Opportunistic infection and disease relapse due to a delayed or impaired cellular immune reconstitution following allogeneic stem cell transplantation (SCT) is associated with significant morbidity and mortality. Various lymphoid subsets have been suggested to play an important role in immune function. However, it remains unknown which of these subsets directly impact survival after SCT. Therefore, we prospectively quantified multiple lymphoid subsets at 3 months following myeloablative allogeneic SCT and evaluated their impact on progression-free survival (PFS).
Quantitative recovery of 13 lymphoid subsets was prospectively characterized in a consecutive cohort of adult patients undergoing T-cell replete myeloablative SCT using peripheral blood stem cells (PBSCs) from a matched sibling donor (MSD) or a matched unrelated donor (MUD), or dual umbilical cord blood (DUCB) grafts. CD3+, CD4+, CD8+, regulatory (Treg) (CD4+, CD25+, CD62L+), cytotoxic (CTL) (CD8+, CD57+, CD28-), and activated T cells (CD8+, HLA-DR+), naïve CD4+ T cells with L-selectin expression (CD4+, CD45RA+/CD45RO-, CD62L+), NK (CD3-, CD16+/CD56+) and NKT cells (CD3+, CD16+/CD56+), B cells (CD19+, CD3-, CD16-, CD56-), plasmacytoid dendritic cells (DCs) (CD123+, CD11c-), and myeloid DCs (CD123-, CD11c+) were analyzed by flow cytometry on fresh peripheral blood. We included 69 patients (MSD, n = 23; MUD, n = 24; DUCB, n = 22) with standard-risk hematologic malignancies who survived at least 3 month (landmark day) following transplantation to evaluate the prognostic impact of lymphoid subset recovery at 3 months on PFS. Standard-risk diseases were defined as acute myelogenous leukemia (AML) in 1st or 2nd complete remission, acute lymphoblastic leukemia (ALL) in 1st or 2nd complete remission, myelodysplastic syndrome (MDS) with blasts <5%, malignant lymphoma (ML) in any complete remission, chronic myelogenous leukemia (CML) in 1st or 2nd chronic phase, and myelofibrosis (MF). PFS was defined as period from the 3 month after transplantation to disease progression or death, whichever occurred first and censored at time of last follow-up. The probability of PFS was estimated according to the Kaplan-Meier method, and groups were compared using the log-rank test. Cox proportional hazards multivariate regression modeling was used to predict PFS. Each lymphocyte subset was dichotomized at the median value and analyzed in a bivariate model adjusted for donor type (MSD/MUD or CBT) as well as in a univariate model in the MSD/MUD group. A parallel analysis was not performed in the CBT group due to few events.
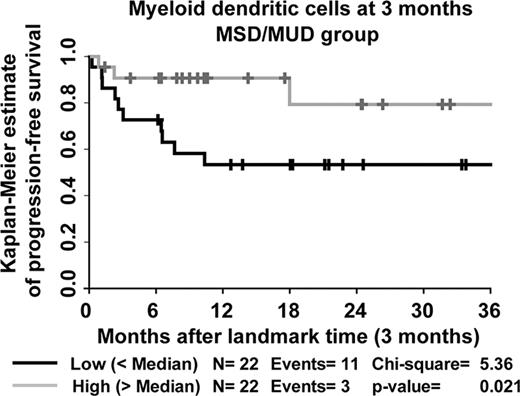
Median age (range) of recipients was 40 (19–65) years. Primary diseases were AML (n = 42), ALL (n = 12), MDS (n = 8), CML (n = 4), ML (n = 2), and MF (n = 1). Tacrolimus-based GVHD prophylaxis was used in 83% of recipients. Median follow-up of survivors after transplantation was 21.1 (range, 3.9–53.6) months. PFS rate at 1 year among DUCB, MSD, and MUD recipients was 0.85 (95% confidence interval, 0.61–0.95), 0.64 (0.40–0.80), and 0.73 (0.49–0.86), respectively, without significant difference between the 3 groups (log-rank test, P = 0.164). Patient characteristics were not associated with PFS in the univariate analysis. In the bivariate analysis controlling for donor type, higher numbers of T cells (P = 0.016), Treg (P = 0.015), CTL (P = 0.041), and myeloid DC (P = 0.028) were significantly associated with improved PFS. In the MSD/MUD group, myeloid DC was the only significant variable (hazard ratio 0.25, 95% confidence interval, 0.07–0.89, P = 0.032) (Figure 1).
Total T cell, regulatory T cell, cytotoxic T cell and myeloid DC recovery at 3 months post transplant is predictive of PFS. Given the unique properties of the DUCB graft, the predictive potential of lymphocyte subsets on PFS may differ from that of MSD/MUD transplant recipients and a larger cohort of DUCB recipients is needed to perform such an analysis. However, among recipients of MSD/MUD grafts, poor myeloid DC recovery at 3 months following transplantation predicted for worse PFS. These data allow for identification of a population at high risk for poor outcome who may be appropriate targets for intervention to augment post-transplant immune recovery using novel techniques.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal