In this issue of Blood, Hu et al show that depletion of mouse macrophages enables the development and persistence of human red blood cells (hRBCs) in immunodeficient mouse models.1
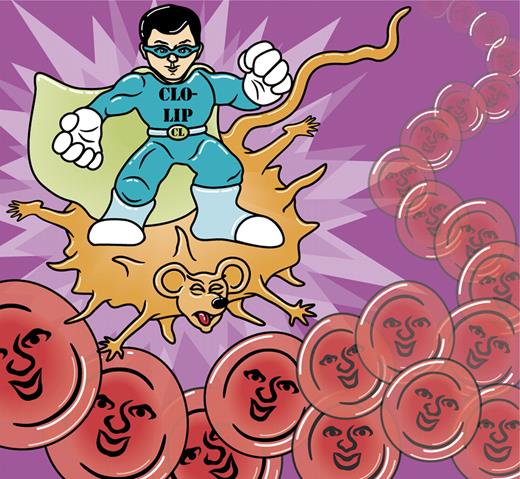
Suppression of mouse macrophages by clodronate liposomes (CLO-LIP) enables hRBC survival in mouse models. Professional illustration by A. Y. Chen.
Suppression of mouse macrophages by clodronate liposomes (CLO-LIP) enables hRBC survival in mouse models. Professional illustration by A. Y. Chen.
Xenotransplantation into immunodeficient mice represents an essential platform for the in vivo study of human hematopoietic cells and diseases that involve them. The NOD/SCID/IL2Rγ−/− (NSG) mouse has been hailed as one of the most accommodating of the immunodeficient strains because of its ability to support the differentiation and survival of various myeloid and lymphoid cell types.2 Yet surprisingly, NSG mice (and other immunodeficient mice strains as well) do not completely support human erythropoiesis or long-term survival of mature hRBCs. Here, a study by Hu and colleagues provides compelling evidence that macrophage-mediated phagocytosis is responsible for the clearance of hRBCs from xenotransplanted mice. The authors show that selective depletion of macrophages facilitates the survival of injected hRBCs as well as the differentiation of mature hRBCs from CD34+ precursors.1 These findings have far-reaching implications as they now permit in vivo models for hRBC development, hRBC diseases, drug development, and the potential development of RBC substitutes from human embryonic stem cells and/or induced pluripotent stem cells.
Without functional T, B, or natural killer cells present to mount an immune response, it has been rather perplexing as to why hRBCs do not survive in immunodeficient mice. Various strategies have been attempted to facilitate the survival of hRBCs including splenectomy, myelosuppressive agents, CD122-blocking antibodies, and injecting an overabundance of hRBCs.3-5 These methods, while varying in their degree of difficulty, achieved modest success with mostly short-lived effects. None of the studies using these approaches examined macrophage-mediated phagocytosis of hRBCs in any detail.
Macrophages are known to play an important role in the detection and elimination of old or defective endogenous RBCs and they use SIRPα/CD47 signaling to discriminate self from foreign. However, previous research has shown that mouse macrophage SIRPα is able to bind human CD47 and may not recognize human cells as “foreign” through this classic cell-surface receptor interaction.6 Hu and colleagues hypothesized that RBC-phagocytosing macrophages may still be responsible for the inability of hRBCs to survive in immunodeficient mice. To test this hypothesis, the authors treated animals with liposome-encapsulated clodronate, a well-documented macrophage depletion tool,7 and noted a significantly prolonged survival of hRBCs in the peripheral blood. They also examined the effects of macrophage depletion on the differentiation of mature hRBCs from CD34+ cells in both NOD/SCID and NSG mice. In the absence of macrophage depletion, only immature nucleated erythroid cells could be found in the bone marrow, seemingly blocked from further maturation and release into the circulation. However, clodronate liposome treatment allowed fully mature, enucleated RBCs to appear in the peripheral blood of both mouse strains (see figure). Using both in vivo and in vitro phagocytosis assays, the authors confirmed that the mouse macrophages readily take up hRBCs and are largely responsibly for their rejection in immunodeficient mice.1 While Hu and colleagues did not identify the exact molecular mechanism for the macrophage-mediated phagocytosis of hRBCs, their data suggest that lack of appropriate SIRPα/CD47 signaling is not the primary trigger.
Clodronate liposomes have been used to deplete or suppress macrophages has been used for roughly 2 decades,:7 the novelty and significance here is its use in the in vivo study of RBC diseases and erythropoiesis. Indeed, malaria researchers have begun taking advantage of clodronate liposomes in their quest to improve P falciparum parasite infection models in humanized mice. In a recent study, repeated clodronate-liposome injections were used to continuously suppress macrophages while repeated hRBC injections helped maintain a constant level of hRBCs, the combination of which allowed parasite infection of hRBCs to be studied over the course of several months.8 Macrophage depletion may also facilitate disease models, drug development, and/or new therapeutic approaches to combat various hemoglobinopathies and other RBC-related diseases.
In addition, clodronate liposomes may be used to study the process of human erythropoiesis in vivo. Renewable cell sources such as human embryonic stem cells and induced pluripotent stem cells may one day be used to manufacture cost-effective RBC substitutes, yet currently, enucleation and/or globin switching to the adult β form are inefficient in vitro systems.9,10 In vivo models using clodronate liposomes may help delineate these processes and will be integral to the continued development of stem cell–derived RBCs.
The newfound knowledge that mouse macrophages play an essential role in clearing hRBCs from immunodeficient mice should provide rationale for developing other directed approaches to increase the longevity and degree of chimerism of hRBCs in the mouse circulation. This is especially important considering that clodronate-liposome–associated toxicity may limit its use. One other interesting observation from the Hu et al study is that, after clodronate liposome delivery, injection of human erythropoietin and human IL3 enhanced the emergence of mature hRBCs. This lends additional support to the finding that human cytokine treatment may improve the engraftment and differentiation of human cells in mice.11 As more and more humanized mouse models are explored, these types of design considerations will be vitally important to their optimization and the information we can learn from our furry friends.
Conflict-of-interest disclosure: The authors are employees of Advanced Cell Technology, a biotechnology company in the field of regenerative medicine. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal