Abstract
Deficiency of the purine salvage enzyme adenosine deaminase leads to SCID (ADA-SCID). Hematopoietic cell transplantation (HCT) can lead to a permanent cure of SCID; however, little data are available on outcome of HCT for ADA-SCID in particular. In this multicenter retrospective study, we analyzed outcome of HCT in 106 patients with ADA-SCID who received a total of 119 transplants. HCT from matched sibling and family donors (MSDs, MFDs) had significantly better overall survival (86% and 81%) in comparison with HCT from matched unrelated (66%; P < .05) and haploidentical donors (43%; P < .001). Superior overall survival was also seen in patients who received unconditioned transplants in comparison with myeloablative procedures (81% vs 54%; P < .003), although in unconditioned haploidentical donor HCT, nonengraftment was a major problem. Long-term immune recovery showed that regardless of transplant type, overall T-cell numbers were similar, although a faster rate of T-cell recovery was observed after MSD/MFD HCT. Humoral immunity and donor B-cell engraftment was achieved in nearly all evaluable surviving patients and was seen even after unconditioned HCT. These data detail for the first time the outcomes of HCT for ADA-SCID and show that, if patients survive HCT, long-term cellular and humoral immune recovery is achieved.
Medscape EDUCATION Continuing Medical Education online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and the American Society of Hematology. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participationin the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 70% minimum passing score and complete the evaluation at http://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 3625.
Disclosures
H. Bobby Gaspar has been an occasional consultant for Enzon Pharmaceuticals Inc, a former manufacturer of polyethylene glycol (PEG-ADA). The remaining authors, the Associate Editor Crystal L. Mackall, and CME questions author Laurie Barclay, freelance writer and reviewer, Medscape, LLC, declare no competing financial interests.
Learning objectives
Upon completion of this activity, participants will be able to:
Compare overall survival (OS) of hematopoietic cell transplantation (HCT) in patients with adenosine deaminase–severe combined immunodeficiency (ADA-SCID) who received transplants from matched sibling donors (MSDs) and matched family donors (MFDs) versus matched unrelated and haploidentical donors, based on a multicenter retrospective study.
Compare outcomes of HCT in patients with ADA-SCID who received unconditioned transplants versus myeloablative procedures, based on a multicenter retrospective study.
Describe long-term immune recovery following HCT in patients with ADA-SCID, based on a multicenter retrospective study.
Release date: October 25, 2012; Expiration date: October 25, 2013
Introduction
Adenosine deaminase (ADA) deficiency is a rare inherited disorder of purine metabolism characterized by the accumulation of toxic metabolites that lead to abnormalities of T-, B-, and natural killer–cell development and function and nonimmunologic manifestations. Affected infants characteristically present with severe opportunistic infections, failure to thrive, and an immunologic profile consistent with SCID (ADA-SCID). Without treatment, the condition is fatal in the first year of life; therefore, it necessitates early intervention.
ADA-deficient SCID accounts for ∼ 10%-20% of all cases of SCID. ADA catalyses the deamination of deoxyadenosine (dAdo) and adenosine to deoxyinosine and inosine, respectively, and the lack of ADA results in the accumulation of dAdo in both intracellular and extracellular compartments.1 Within cells, conversion of dAdo by deoxycytidine kinase to deoxyadenosinetrisphosphate (dATP) leads to intracellular expansion of the dATP pool. The build-up of both dATP and dAdo has deleterious effects on lymphocyte development and function through a variety of different mechanisms, including dATP inhibition of ribonucleotide reductase, an enzyme necessary for DNA replication and repair, and induction of apoptosis in immature thymocytes.2 Although ADA is expressed in all body tissues, the profound lymphopenia seen in typical ADA-SCID may be best explained by the expression pattern of ADA, which is highest in T cells and in thymic progenitors3,4 and also by increased expression of deoxycytidine kinase in lymphocytes, which increases dATP accumulation from dAdo in immune cells more than in other tissues.5 The ubiquitous nature of ADA expression does, however, lead to significant nonimmunologic defects, including costochondral and skeletal dysplasias,6 neurologic deficits that involve motor function,7 bilateral sensorineuronal deafness,8 hepatic dysfunction,9 and defects in cognitive and behavioral function.10,11 The underlying pathogenesis and variety of clinical defects suggest that ADA deficiency is a metabolic disease with the most severe manifestations in the immune system.
Unlike other forms of SCID, several options are available for the treatment of ADA-SCID, namely hematopoietic stem cell transplantation (HCT), enzyme replacement therapy (ERT) with polyethylene glycol (PEG)–ADA,12,13 and more recently gene therapy (GT)14,15 (reviewed in Gaspar et al16 ). HCT has been the treatment of choice, but, with other management strategies available, it is essential to gather formal HCT outcome data so that informed choices can be made about optimal treatment. To date, there has been no formal data on the outcome related to transplantation for ADA-SCID alone. Although several studies have documented the survival outcome for all forms of SCID after HCT, large-scale detailed data on ADA-SCID transplantation outcome and immune recovery are not readily available. In a series of 475 patients with SCID from the European SCETIDE database, 51 patients with ADA-SCID were included, and the study documented a 3-year survival of 81% for HLA-matched transplantations and 29% for HLA-mismatched transplantations with no information on the degree of immune recovery.17 Only 4 unrelated donor transplantations were reported in this series, and no outcome data on these patients were presented. A more recent report on 699 patients with SCID included 75 patients with ADA-SCID, but the specific outcome for the patients with ADA-SCID alone was not documented.18 A series of 15 patients with ADA-SCID showed overall survival (OS) of 80%, but there were only 6 transplantations from mismatched family donors and 2 transplantations from unrelated donors in this series.19 The paucity of formal outcome data has limited the ability to make informed choices about transplantation. There has also been a perception among transplantation physicians that patients with ADA are more difficult to transplant, especially from unrelated and haploidentical donors. For these reasons, we initiated a multicenter survey designed to look at the survival outcome for patients with ADA-SCID after HCT, to examine the risk factors associated with survival, and to evaluate the extent of immune recovery after HCT.
Methods
A retrospective questionnaire-based analysis of 106 children with ADA-SCID was undertaken. The questionnaire was developed and approved by the Inborn Errors Working Party of the European Blood and Marrow Transplant Society and the BMT Working Party of the European Society of Immunodeficiencies. Questionnaires were distributed to all Inborn Errors Working Party members and to centers in North America and Saudi Arabia known to have performed transplantations for children with ADA-SCID. HCTs were performed between August 1981 and March 2009 in 16 international transplantation centers. A full list of transplantation centers and the number of transplantations performed are available in supplemental Table 1 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Data were gathered and stored anonymously.
Transplantation characteristics
ADA deficiency was diagnosed by genetic analysis or standard biochemical assays of ADA activity. A total of 106 patients (54 males and 52 females) underwent 119 transplantations. The median age at transplantation was 4 months (range, 2 weeks to 7 years). The median follow-up after transplantation was 6.5 years (range, 1.6-27.6 years). Details of transplantations undertaken are given in Table 1. There were 42 fully matched sibling donors (MSDs). Of the 12 matched family donors (MFDs), 11 were full matches and 1 was a single antigen mismatch. All 15 matched unrelated donors (MUDs) were matched to ≥ 10 of 10 loci (6 were matched at 12 of 12 loci) except for 1 donor who was matched at 8 of 8 loci. Haploidential (HAPLO) donors were antigen mismatched at > 2 loci.
Summary of patients and transplant characteristics
| . | Value . |
|---|---|
| Sex, n | |
| Male | 54 |
| Female | 52 |
| Ratio | 1.04 |
| PEG-ADA treatment, n | |
| Yes (> 3 mo) | 13 |
| No | 93 |
| Type of HCT, n | |
| MSD | 42 |
| MFD | 12 |
| MUD | 15 |
| MMUD | 7 |
| HAPLO | 30 |
| Intensity of conditioning, n | |
| None | 49 |
| RIC | 12 |
| MAC | 45 |
| Source of stem cell, n | |
| BM | 88 |
| PBSC | 9 |
| UCB | 9 |
| . | Value . |
|---|---|
| Sex, n | |
| Male | 54 |
| Female | 52 |
| Ratio | 1.04 |
| PEG-ADA treatment, n | |
| Yes (> 3 mo) | 13 |
| No | 93 |
| Type of HCT, n | |
| MSD | 42 |
| MFD | 12 |
| MUD | 15 |
| MMUD | 7 |
| HAPLO | 30 |
| Intensity of conditioning, n | |
| None | 49 |
| RIC | 12 |
| MAC | 45 |
| Source of stem cell, n | |
| BM | 88 |
| PBSC | 9 |
| UCB | 9 |
PEG-ADA indicates polyethylene glycol–adenosine deaminase; HCT, hematopoietic cell transplantation; MSD, matched sibling donor; MFD, matched family donor; MUD, matched unrelated donor; MMUD, mismatched unrelated donor; HAPLO, haploidential; RIC, reduced intensity conditioning; MAC, myeloablative intensity conditioning; BM, bone marrow; PBSC, peripheral blood stem cells; and UCB, umbilical cord blood.
Twenty-three patients received treatment with PEG-ADA before HCT, whereas 83 patients proceeded to HCT without prior ERT. Of the 23 patients, PEG-ADA was given for < 3 months in 10 patients and > 3 months in 13 patients. Data on the type and intensity of the conditioning regimen were available on all 106 patients of which myeloablative intensity conditioning (MAC) was used in 45 patients, reduced intensity conditioning (RIC) in 12, and no conditioning in 49 patients. MAC consisted of busulfan/cyclophosphamide in all 45 patients, although in 3 patients thiotepa was used in addition. RIC consisted of fludarabine/melphalan in 5 patients, fludarabine/treosulfan in 1 patient, treosulfan/cyclophosphamide in 1 patient, cyclophosphamide alone in 4 patients, and busulfan 8 mg/fludarabine in 1 patient. Of the no conditioning cohort, 2 were given alemtuzumab, and 1 patient was given rituximab and ATG. The stem cell source used was BM in 88 patients, peripheral blood stem cells (PBSCs) in 9, and umbilical cord blood (UCB) stem cells in 9 patients.
Immune reconstitution
Data were collected retrospectively on all patients at ∼ 6, 12, and 24 months and at the time of last follow-up visit. Data included absolute lymphocyte counts and T-cell (CD3, CD4, and CD8) and B-cell (CD19 and CD20) numbers. Data were also collected on the time taken from date of transplantation to normal PHA response. Humoral reconstitution was assessed by levels of serum Ig and by whether patients had discontinued Ig replacement therapy. In patients who stopped Ig replacement, their response to standard vaccinations was measured.
TRM and OS
The status of patients after HCT was noted in all patients, including date and cause of death. Transplantation-related mortality (TRM) was calculated from deaths in the first 100 days after HCT. Overall survival (OS) was calculated from the number of patients alive at the time of analysis.
Statistical analysis
Kaplan-Meier curves were used to analyze survival figures. The log-rank test (Mantel-Cox) and Gehan-Breslow-Wilcoxon tests were used to compare survival between different groups. Logistic regression was performed, using SPSS (SPSS Inc), to identify determinants of survival after HCT. Statistical analysis, including hazard ratio calculation, was performed with GraphPad Prism Version 5.00 for Windows (GraphPad Software; www.graphpad.com).
Results
The OS for the 106 patients studied was 67% (n = 71) with a TRM of 20%. In the overall cohort, the mean time to death after HCT was 142 days and the median time was 54 days (range, 1 day to 2 years). Several variables, including donor source, intensity of conditioning regime, use of PEG-ADA, age at transplantation, dATP levels at diagnosis, and the stem cell source, were subject to univariate and multivariate analyses to identify the main risk factors that influenced outcome after HCT (Tables 2, 3, and 4).
Influence of various risk factors that affect survival outcome after HCT (univariate analysis)
| Features . | Percentage . | n/N . | OS, % . | HR . | 95% CI . | P . |
|---|---|---|---|---|---|---|
| Donor source | ||||||
| MSD | 41 | 42/106 | 86 | |||
| MFD | 13 | 12/106 | 83 | 0.73 | 0.1287-4.158 | .72 |
| MUD | 14 | 15/106 | 67 | 0.263 | 0.063 65-1.92 | .05 |
| MMUD | 7 | 7/106 | 29 | 0.01459 | 0.001924-0.1107 | < .001 |
| HAPLO | 28 | 30/106 | 43 | 0.1629 | 0.068 24-0.3887 | < .001 |
| Conditioning | ||||||
| None | 46 | 49/106 | 78 | |||
| RIC | 11 | 12/106 | 67 | 0.51 | 0.1336-1.967 | .29 |
| MAC | 42 | 45/106 | 56 | 0.407 | 0.1996-0.8333 | .009 |
| PEG-ADA | ||||||
| No | 88 | 93/106 | 67 | |||
| Yes > 3 mo | 12 | 13/106 | 69 | 1.034 | 0.3690-2.898 | .97 |
| Age at transplantation | ||||||
| Birth to 6 mo | 63 | 67/106 | 72 | |||
| 6-12 mo | 25 | 26/106 | 58 | 0.556 | 0.2443-1.266 | .20 |
| 1-5 y | 11 | 12/106 | 58 | 0.6253 | 0.2026-1.930 | .59 |
| > 5 y | 1 | 1/106 | ||||
| dATP levels | ||||||
| 0-1000μM | 43 | 20/46 | 55 | |||
| > 1000μM | 56 | 26/46 | 73 | 1.829 | 0.6734-4.968 | .28 |
| Stem cell source | ||||||
| BM | 83 | 88/106 | 68 | |||
| PBSC | 8 | 9/106 | 67 | 0.8107 | 0.2228-2.950 | .58 |
| UCB | 8 | 9/106 | 56 | 0.4496 | 0.1171-1.726 | .16 |
| Features . | Percentage . | n/N . | OS, % . | HR . | 95% CI . | P . |
|---|---|---|---|---|---|---|
| Donor source | ||||||
| MSD | 41 | 42/106 | 86 | |||
| MFD | 13 | 12/106 | 83 | 0.73 | 0.1287-4.158 | .72 |
| MUD | 14 | 15/106 | 67 | 0.263 | 0.063 65-1.92 | .05 |
| MMUD | 7 | 7/106 | 29 | 0.01459 | 0.001924-0.1107 | < .001 |
| HAPLO | 28 | 30/106 | 43 | 0.1629 | 0.068 24-0.3887 | < .001 |
| Conditioning | ||||||
| None | 46 | 49/106 | 78 | |||
| RIC | 11 | 12/106 | 67 | 0.51 | 0.1336-1.967 | .29 |
| MAC | 42 | 45/106 | 56 | 0.407 | 0.1996-0.8333 | .009 |
| PEG-ADA | ||||||
| No | 88 | 93/106 | 67 | |||
| Yes > 3 mo | 12 | 13/106 | 69 | 1.034 | 0.3690-2.898 | .97 |
| Age at transplantation | ||||||
| Birth to 6 mo | 63 | 67/106 | 72 | |||
| 6-12 mo | 25 | 26/106 | 58 | 0.556 | 0.2443-1.266 | .20 |
| 1-5 y | 11 | 12/106 | 58 | 0.6253 | 0.2026-1.930 | .59 |
| > 5 y | 1 | 1/106 | ||||
| dATP levels | ||||||
| 0-1000μM | 43 | 20/46 | 55 | |||
| > 1000μM | 56 | 26/46 | 73 | 1.829 | 0.6734-4.968 | .28 |
| Stem cell source | ||||||
| BM | 83 | 88/106 | 68 | |||
| PBSC | 8 | 9/106 | 67 | 0.8107 | 0.2228-2.950 | .58 |
| UCB | 8 | 9/106 | 56 | 0.4496 | 0.1171-1.726 | .16 |
OS indicates overall survival; HR, hazard ratio; and CI, confidence interval. For additional abbreviation expansions please see Table 1.
Outcome after HCT in relation to different donor sources
| Donor source . | No. of patients . | Age at HCT, mo . | Intensity of conditioning regime for survivors, n (%) . | Engraftment . | No. of repeat transplantations . | TRM, n (%) . | OS, n (%) . | ||
|---|---|---|---|---|---|---|---|---|---|
| No conditioning, n (%) . | RIC, n (%) . | MAC, n (%) . | |||||||
| MSD | 42 | 30 (83) | 4 (100) | 8 (88) | 39 (91) | 4 | 3 (7) | 36 (86) | |
| Median | 3 | ||||||||
| Mean | 6.5 | (25/30) | (7/8) | ||||||
| Range | 0.5-84 | ||||||||
| MFD | 12 | 10 (80) | 1 (100) | 1 (100) | 10 (91) | 0 | 0 (0) | 10 (83) | |
| Median | 3 | ||||||||
| Mean | 6.09 | (8/10) | |||||||
| Range | 1-30 | ||||||||
| MUD | 15 | 3 (67) | 4 (50) | 8 (75) | 14 (93) | 1 | 4 (27) | 10 (67) | |
| Median | 7 | ||||||||
| Mean | 11.2 | (2/3) | (2/4) | (6/8) | |||||
| Range | 1-48 | ||||||||
| MMUD | 7 | 2 (50) | 5 (20) | 7 (100) | 0 | 4 (57) | 2 (29) | ||
| Median | 9 | ||||||||
| Mean | 8.7 | (1/2) | (1/5) | ||||||
| Range | 2-20 | ||||||||
| HAPLO | 30 | 6 (50) | 1 (0) | 23 (43) | 11 (37) | 8 | 10 (33) | 13 (43) | |
| Median | 5 | ||||||||
| Mean | 5.4 | (3/6) | (10/23) | ||||||
| Range | 2-16 | ||||||||
| Donor source . | No. of patients . | Age at HCT, mo . | Intensity of conditioning regime for survivors, n (%) . | Engraftment . | No. of repeat transplantations . | TRM, n (%) . | OS, n (%) . | ||
|---|---|---|---|---|---|---|---|---|---|
| No conditioning, n (%) . | RIC, n (%) . | MAC, n (%) . | |||||||
| MSD | 42 | 30 (83) | 4 (100) | 8 (88) | 39 (91) | 4 | 3 (7) | 36 (86) | |
| Median | 3 | ||||||||
| Mean | 6.5 | (25/30) | (7/8) | ||||||
| Range | 0.5-84 | ||||||||
| MFD | 12 | 10 (80) | 1 (100) | 1 (100) | 10 (91) | 0 | 0 (0) | 10 (83) | |
| Median | 3 | ||||||||
| Mean | 6.09 | (8/10) | |||||||
| Range | 1-30 | ||||||||
| MUD | 15 | 3 (67) | 4 (50) | 8 (75) | 14 (93) | 1 | 4 (27) | 10 (67) | |
| Median | 7 | ||||||||
| Mean | 11.2 | (2/3) | (2/4) | (6/8) | |||||
| Range | 1-48 | ||||||||
| MMUD | 7 | 2 (50) | 5 (20) | 7 (100) | 0 | 4 (57) | 2 (29) | ||
| Median | 9 | ||||||||
| Mean | 8.7 | (1/2) | (1/5) | ||||||
| Range | 2-20 | ||||||||
| HAPLO | 30 | 6 (50) | 1 (0) | 23 (43) | 11 (37) | 8 | 10 (33) | 13 (43) | |
| Median | 5 | ||||||||
| Mean | 5.4 | (3/6) | (10/23) | ||||||
| Range | 2-16 | ||||||||
Influence of various risk factors that affect survival outcome after HCT (multivariate analysis)
| Independent variable . | Regression coefficient . | Odds ratio (SE) . | P . |
|---|---|---|---|
| Constant | 1.8 | 6.3 | < .001* |
| Donor source | |||
| MSD | — | — | |
| MFD | −0.19 | 0.83 | .834 |
| MUD | −1.81 | 0.16 | .083 |
| MMUD | −3.87 | 0.02 | .007* |
| HAPLO | −2.86 | 0.06 | < .001* |
| Conditioning | |||
| None | — | — | — |
| RIC | 0.28 | 1.32 | .766 |
| MAC | 0.58 | 1.78 | .413 |
| PEG-ADA given | 1.45 | 4.26 | .110 |
| Age at transplantation | |||
| Birth to 6 mo | — | — | |
| 6-12 mo | −0.12 | 0.84 | .883 |
| 1-5 y | −1.30 | 0.27 | .124 |
| Stem cell source | |||
| BM | — | — | |
| PBSC | 0.90 | 2.45 | .29 |
| UCB | 0.42 | 1.52 | .688 |
| Independent variable . | Regression coefficient . | Odds ratio (SE) . | P . |
|---|---|---|---|
| Constant | 1.8 | 6.3 | < .001* |
| Donor source | |||
| MSD | — | — | |
| MFD | −0.19 | 0.83 | .834 |
| MUD | −1.81 | 0.16 | .083 |
| MMUD | −3.87 | 0.02 | .007* |
| HAPLO | −2.86 | 0.06 | < .001* |
| Conditioning | |||
| None | — | — | — |
| RIC | 0.28 | 1.32 | .766 |
| MAC | 0.58 | 1.78 | .413 |
| PEG-ADA given | 1.45 | 4.26 | .110 |
| Age at transplantation | |||
| Birth to 6 mo | — | — | |
| 6-12 mo | −0.12 | 0.84 | .883 |
| 1-5 y | −1.30 | 0.27 | .124 |
| Stem cell source | |||
| BM | — | — | |
| PBSC | 0.90 | 2.45 | .29 |
| UCB | 0.42 | 1.52 | .688 |
— indicates reference.
indicates significant.
Donor source and intensity of conditioning
Donor source had a major effect on the outcome of HCT. OS was higher in MSD and MFD HCTs (86% and 83%, respectively). Comparison of survival outcomes in MMUD and HAPLO transplantations (29% and 43%, respectively) with survival outcomes of MSD HCTs showed a highly significant difference (P < .001). Comparison of OS in MSD HCT with MUD HCT (67%) also showed a significant difference (P < .05; Table 2; Figure 1A). The majority of deaths (63%; 22 of 35) after all types of transplantations were in the first 100 days after HCT, with 13 deaths after 100 days (Figure 1A). The causes of death were mainly related to pneumonitis/respiratory failure and sepsis, which formed > 50% of all deaths. Other main causes included GVHD (15%) and fungal infection (11%; supplemental Figure 1). Of the 13 deaths after 100 days only 2 were related to transplant-related complications, namely chronic GVHD.
OS after HCT. Kaplan-Meier curve showing OS in relation to donor source (A) and intensity of conditioning (B).
OS after HCT. Kaplan-Meier curve showing OS in relation to donor source (A) and intensity of conditioning (B).
Most MSD/MFD transplantations were undertaken without any chemotherapy as were a smaller number of MUD and HAPLO transplantations, and this may have had a major effect on outcome. When conditioning itself was studied, a significantly improved OS was observed in unconditioned transplantations in comparison with transplantations after MAC (78% vs 56%; P = .009). Transplantations after RIC had an OS of 67%, and this was not significantly different from outcomes after unconditioned procedures (Table 2; Figure 1B).
Despite the lack of conditioning in most MSD/MFD transplantations, a high rate of engraftment was observed. Of the 40 unconditioned transplantations in the 2 groups there was an engraftment rate of 90% (35 of 39; 1 of the 40 patients died at day 14 and was hence excluded from the engraftment analysis). Four of 30 unconditioned MSD transplantations did not engraft (2 from matched cord blood and 2 from sibling donor marrow) and were retransplanted successfully. In contrast, of 6 patients who received a HAPLO infusion without conditioning, only 1 patient had successful engraftment, 1 patient died before day 100, and the remaining 4 survivors had failed to engraft. One of these latter 4 patients received 2 further unconditioned infusions without success and then went on to receive a MAC HAPLO transplant with 100% engraftment. A second patient received another unconditioned infusion with no success and died of sepsis. Unconditioned procedures were performed in 3 unrelated donor transplantations, 2 transplants did not engraft, which emphasizes the importance of donor compatibility in allowing success of unconditioned transplantations.
The degree of HLA disparity appears to play the major role in determining outcome, irrespective of conditioning regime. As shown in Table 3, the median and mean times at which transplantations were undertaken are similar for the different donor groups. When the type of conditioning within transplantations from different donor sources is studied, there is good survival in MSD/MFD transplantations even in RIC and MAC regimes (Table 3), whereas survival is decreased in MUD transplantations and is much worse in MMUD and HAPLO transplantations. Twenty-three patients underwent MAC transplantation from a HAPLO donor with an OS of 43% (10 of 23). Similarly only 1 of 5 MMUD transplantations survived a MAC procedure. By contrast 14 of 17 patients (82%) survived a MAC procedure from MSDs or MFDs or MUDs. Transplantations after RIC had an OS of 67%, although total numbers are relatively small (n = 12). Within the RIC group, survival was better after MSD/MFD transplantations (OS, 100%; 5 of 5) than after MUD/MMUD/HAPLO HCT (OS, 43%; 3 of 7).
The importance of donor source is supported by further statistical analysis. Logistic regression (Table 4) that explored the effect of various factors on OS again showed that donor type was a significant predictor of outcome. Specifically, it was found that transplantation from MMUDs or HAPLO donors significantly decreases the likelihood of OS in comparison with MSDs when controlling for all other variables. In this multivariate analysis the choice of conditioning regimen was not a statistically significant factor.
We also looked to determine whether there had been an improvement in transplantation outcome with time as a result of increased awareness of SCID, greater SCID HCT experience, and improved transplant-related processes/medications. The OS by decade for all HCTs improved from 51.7% (before 1991) to 73.1% (1991-2000) and 72.5% (2000-2009). We also looked at outcomes in HAPLO transplantations that have a poor outcome to determine whether there had been improvements in more recent years. The OS by decade was 40% (before 1991; n = 20; 12 deaths), 0% (1991-2000; n = 3; 3 deaths), and 71.4% (2000-2009; n = 7; 2 deaths). However, of the 5 survivors in the 2000-2009 time period, 2 did not engraft, of which 1 required a GT procedure for rescue and a second started PEG-ADA and then underwent 2 MSD transplantations from a newly born sibling and subsequently died of pneumonitis. Thus, 3 of 7 patients (42.3%) underwent a successful HAPLO transplantation between 2000 and 2009. MUD procedures were initiated in 1995 and hence were not analyzed by decade.
Analysis of other variables that contribute to outcome
Several other variables that might contribute to outcome were also studied (Table 2). The use of PEG-ADA may detoxify and allow stabilization of patients before transplantation. Patients were therefore divided into those who had received no or short-term (< 3 months) PEG-ADA (n = 93) and those who had received enzyme for > 3 months (n = 13), because this would be an appropriate time period for metabolic detoxification to occur. No difference in survival outcome was found between the 2 groups (supplemental Figure 2A).
The age of the child at transplantation did not have an influence on the outcome of transplantation. Patients were subdivided into 4 groups, birth to 6 months, 6 months to 1 year, 1-5 years, and > 5 years, although there was only 1 patient in the latter category and was therefore not subject to statistical analysis. A trend to better survival was observed in the younger age group, but this was not statistically significant (supplemental Figure 2B).
The levels of toxic metabolites are an indicator of residual ADA activity; furthermore, the severity of ADA gene mutations has previously been shown to correlate with the severity of immune and nonimmune features of the disease.10 To investigate whether these variables affected outcome, patients were categorized into 2 groups according to their dATP level at presentation; group 1 included patients with a dATP of 0-1000μM and group 2 included patients with levels > 1000μM. No significant difference in TRM or OS was observed between the 2 groups (P = .89 and P = .56, respectively; supplemental Figure 2C). The source of stem cell used (BM, PBSCs, or UCB stem cells) also had no significant effect on TRM or OS (P = .18 and P = .92, respectively; supplemental Figure 2D).
Immune recovery after transplantation
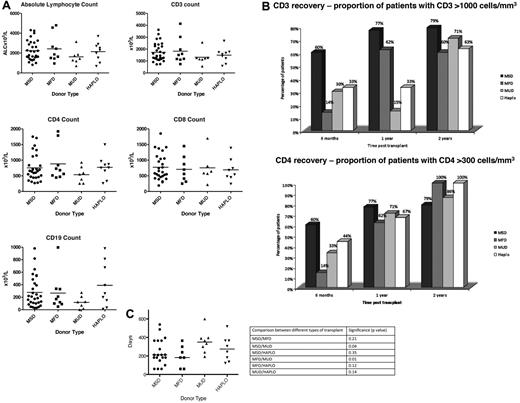
Seventy-one patients are alive, and data on immune reconstitution are available on 55 of those patients. The median time from transplantation to date of last follow-up was 6 years (range, 1-22 years) with a mean follow-up time of 6.6 years. Reconstitution was analyzed in relation to the type of transplantation. Only 2 patients who received a MMUD transplant survived, and so these patients are not shown in this analysis. At last follow-up, no significant difference was observed between the different transplantation groups in terms of the absolute lymphocyte count and total CD3, CD4, CD8, and CD19 lymphocyte subpopulations (Figure 2A).
Immune recovery at last follow-up in relation to donor source. (A) Levels of absolute lymphocytes and CD3, CD4, CD8, and CD19 cells at last follow-up. (B) Proportion of CD3 recovery > 1000 cells/mm3 and CD4 recovery > 300 cells/mm3 at 6 months, 1 year, and 2 years after HCT. (C) Time to achieve a normal PHA response after different donor type.
Immune recovery at last follow-up in relation to donor source. (A) Levels of absolute lymphocytes and CD3, CD4, CD8, and CD19 cells at last follow-up. (B) Proportion of CD3 recovery > 1000 cells/mm3 and CD4 recovery > 300 cells/mm3 at 6 months, 1 year, and 2 years after HCT. (C) Time to achieve a normal PHA response after different donor type.
The kinetics of T-cell recovery was also studied in relation to the type of transplantation (Figure 2B). The total CD3+ T-cell count was > 1000 cells/mm3 at 1 year in a significantly larger number of MSD transplantations (77%) and MFD HCTs (62%) compared with 33% of haploidentical HCTs and 15% of MUD/MMUD HCTs. At 2 years after transplantation, however, the proportion of patients who had attained a CD3+ count > 1000 cells/mm3 was similar in MSD/MUD/HAPLO transplantations. The difference in T-cell recovery is probably related to the number of CD8+ cells, because, if CD4+ reconstitution is analyzed separately, equivalent numbers of patients in the different donor subgroups have > 300 cells/mm3 at 6 months, 1 year, and 2 years after HCT. The time to a normal PHA response is also significantly quicker in MSD/MFD transplantations in comparison with MUD transplantations and most probably reflects the rate of T-cell recovery.
Although unconditioned transplantations result in improved survival and comparable immune reconstitution in comparison with transplantations after RIC and MAC, the question arises as to whether the lack of conditioning results in the engraftment of prethymic progenitors that will allow long-lived T-cell immunity. T-cell receptor excision circle (TREC; a surrogate marker of thymic activity) levels in CD4+ and CD8+ cells were available in several patients who had received unconditioned or RIC transplants (insufficient measurements were available in patients who had received MAC transplants). Both CD4+ and CD8+ TREC levels were at low levels in patients receiving unconditioned transplants. Although, the numbers of patients were small and numbers were variable, there was a trend to increased CD4+ and CD8+ TRECs in patients receiving RIC transplants (supplemental Figure 3).
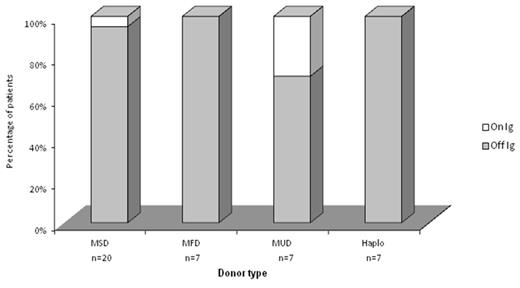
Humoral recovery was assessed by the number of patients who had discontinued Ig replacement therapy and who had made specific responses after vaccination. Data were available on 46 patients, and of those patients 41 (89%) have normal level of Ig for age and have stopped Ig replacement therapy. This was not related to donor source, and most patients in each group had been able to discontinue Ig replacement (Figure 3). Of 36 patients on whom vaccination-specific data were available, 34 were documented to have produced protective levels of tetanus-specific antibody, 1 patient had low levels, and 1 patient was in the process of being vaccinated.
Humoral recovery after HCT in relation to donor type. The proportion of patients who have stopped Ig replacement is indicated in gray, and the proportion continuing Ig replacement is indicated in white.
Humoral recovery after HCT in relation to donor type. The proportion of patients who have stopped Ig replacement is indicated in gray, and the proportion continuing Ig replacement is indicated in white.
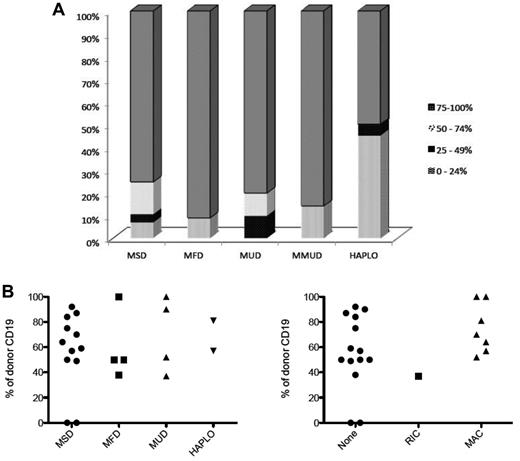
Degree of chimerism after HCT
Data on the degree of donor T-cell chimerism were available on 73 patients after transplantation. The median time at which data were available was 5 years after HCT (2 weeks to 26 years). The degree of donor chimerism in T cells is shown in Figure 4A. Chimerism was categorized into 4 different groups (0%-24%, 25%-49%, 50%-74%, and 75%-100%) and analyzed in relation to the donor source. In MSD/MFD/MUD/MMUD transplantations, most patients had donor chimerism in 75%-100% of T cells with most of these showing 100% donor chimerism. In MMUD transplantations, which had a poor survival outcome, the level of donor chimerism shown was at the last time point before death. After HAPLO transplantations (data on 20 patients), 9 had chimerism in the low 0%-24% range and 4 of 9 of these did not receive any conditioning and 5 of 9 had a MAC procedure. Ten HAPLO transplantations had T-cell chimerism in the high 75%-100% range and 9 of 10 had received a MAC transplant.
Donor chimerism after HCT. (A) The degree of donor T-cell chimerism in relation to donor type is shown. (B) The degree of donor B-cell chimerism in relation to donor type (left) and intensity of conditioning (right) is shown.
Donor chimerism after HCT. (A) The degree of donor T-cell chimerism in relation to donor type is shown. (B) The degree of donor B-cell chimerism in relation to donor type (left) and intensity of conditioning (right) is shown.
Data on B-cell chimerism were available on 22 patients after HCT (Figure 4B). Only 2 of 22 patients had no B-cell engraftment, and this was seen in 2 patients who received MSD transplants without conditioning. In all the other 20 patients regardless of donor type or conditioning regime, levels of donor B-cell engraftment at levels of ≥ 30% were seen. Notably, in 10 of 12 patients who received a MSD transplant without conditioning, B-cell engraftment of > 40% was seen. In the 2 patients with 0% B-cell chimerism, there was nevertheless, an increase in the number of recipient B cells and full restoration of humoral immunity with normal Ig production and specific responses to vaccinations. In 9 patients, where paired B and myeloid chimerism was available, 7 had marked differences (> 40%) in the level of chimerism between B and myeloid lineages, suggesting that there may be a selective advantage for donor B cells.
Metabolic correction after HCT
dATP levels as a measure of metabolic correction were available in 24 patients. The mean dATP value for all 24 patients was 71μM with a median value of 46μM (range, 0-227μM). Of these 24 patients 11 patients had an MSD transplantation with a median dATP value of 82μM (range, 0-163μM), 5 had MFD transplantation with a median dATP of 25μM (range, 10-174μM), 6 had MUD transplantation with a median dATP of 56.5μM (range, 0-227μM), and only 2 patients underwent a HAPLO HCT (dATP values, 5μM and 37μM, respectively). When analyzed by intensity of conditioning, 17 patients had no conditioning with a median dATP value of 82μM (range, 10-227μM), 3 received RIC with a median dATP value of 30μM (range, 0-37μM), and 4 received MAC with a median value of 21μM (range, 0-111μM). No statistical difference in metabolic correction after transplantation was observed between the different groups.
Discussion
The outcome of allogeneic HCT transplantations for children with SCID has improved dramatically over time.17,18 The overall message from these publications may however mask the fact that some SCID conditions may be more difficult to treat than others. Indeed, when subtype analysis of different SCID types has been undertaken,17 it has been shown that patients with T-B+ SCID fare significantly better than patients with T-B− SCID, but this analysis has not been extended to all SCID forms. The genetic basis of > 18 different forms of SCID has now been characterized, and the molecular pathogenesis in these different forms is now well understood and ranges from defects of molecules with expression restricted to the immune system to those in which proteins are more ubiquitously expressed. It is therefore important that we are able to understand the prognosis for each different form of SCID rather than for SCID as a collection of diverse disorders. This will allow better counseling for families but also will enable physicians to understand where and how transplantations can be improved and also when other treatment options should be pursued.
The metabolic nature of ADA-SCID has always distinguished this disease from other forms of SCID. The impression has also been held by treating physicians that the condition is more difficult to treat, but there have been no objective data to support this notion. In this retrospective study of 106 patients treated in Europe, North America, and the Middle East, we detail the outcome of HCT for ADA-SCID and highlight risk factors associated with survival.
It is clear from the data presented here that donor type is the most important factor to influence outcome. OS was significantly better after MSD and MFD HCTs than after transplantations from other donor sources (Tables 2 and 3). The ability to perform MSD/MFD HCTs without conditioning and soon after the diagnosis (because of the ready availability of the donor) may be major contributions to this improved outcome. However, the improved outcome can also be seen (albeit at smaller numbers) in conditioned transplants from these donor sources. The superior results after MSD/MFD transplantations may reflect a shorter donor search to transplantation time in comparison with unrelated donor transplantations where the delay may affect negatively on the clinical status of the patient. MSD/MFD transplantations are generally undertaken without serotherapy, unlike MUD/MMUD/HAPLO transplantations, and this is reflected in the faster and better recovery of CD3+ cells in the first year after transplantation in recipients of MSD/MFD HCTs (Figure 2A). This in turn may allow more rapid T cell–mediated resolution of viral infections than transplantations from other donor sources.
In contrast poor outcome was observed after HCT from HAPLO donors (Tables 2 and 3). In this series, unconditioned HAPLO T cell–depleted transplantations had a high rate of graft failure or rejection, which contrasts markedly from the data for similar transplantations performed in SCID-X1.20 In general, patients with ADA-SCID are severely lymphopenic, lacking both T and natural killer cells, so that the basis of nonengraftment is unlikely to relate to immunologic rejection. Alternative explanations may include the inability of the ADA-deficient marrow stromal microenvironment to support engraftment of wild-type HSCs, and this is supported by in vitro murine data which show that mesenchymal stromal cells from ADA−/− mice have a decreased ability to support colony formation compared with mesenchymal stromal cells from wild-type mice.21 This hypothesis most probably relates to the support of progenitor cells, because, although unconditioned MSD/MFD transplantations with infusions of whole marrow are able to engraft, under these conditions the engraftment is mainly of more mature cells. Further experimental evidence is required to study this question in more detail. In the HAPLO and MMUD setting conditioned transplantations also have poor outcome, and this may relate to the inability to withstand toxicity associated with the conditioning regime or the delayed T-cell reconstitution, which may prevent clearance of viral infection.
Data from MUD transplantations are significantly worse than data from MSD/MFD transplantations but are much better than data from MMUD/HAPLO procedures. The numbers of MUD transplantations remain considerably lower than MSD/MFD transplantations, and so, as better conditioning regimes become available,22 it may be expected that there will be an improvement in the survival figures with time.
One surprising issue was the lack of any beneficial effect of using PEG-ADA in patients for ≥ 3 months before transplantation. Patients with ADA-SCID present with significant infections coupled with a metabolic toxicity that demands immediate treatment. The use of PEG-ADA to achieve rapid systemic detoxification is well documented and is associated at least anecdotally with improved clinical well-being, and so it may have been expected that this would result in improved transplantation survival. However, patients maintained on PEG-ADA for > 3 months (n = 13) are often those for whom no immediate MSDs/MFDs are available, and of this cohort 12 of 13 patients went on to have a MUD/MMUD/HAPLO transplantation, again emphasizing the role of donor source in determining transplantation outcome. In previous studies on all forms of SCID, patients who received a transplant at a younger age (< 6 months) were found to have an improved outcome.17 In this study, as can be seen from Table 2 and supplemental Figure 2B, patients who received a transplant < 6 months of age had an OS of 72% compared with 58% in the other 2 groups (6-12 months and 1-5 years), but this improved outcome was not statistically significant. This is most probably related to the total numbers of patients in the older groups (6-12 months, n = 26; 1-5 years, n = 12), which were much lower than that seen in the < 6-month group (n = 67).
The study also allowed us to look at cellular and humoral immune reconstitution and the donor cell engraftment after HCT. The data are not complete and highlight the limitations of a multicenter retrospective study such as this, which are acknowledged. Nevertheless, the data available do allow certain conclusions to be drawn. Overall long-term immune reconstitution in all patients after HCT appears to be comparable between the different donor groups. Although there is an improvement in initial T-cell recovery in MSD/MFD HCTs (which is most probably related to the lack of serotherapy used), the absolute numbers of T-cell numbers long term is similar for all transplantation types. Similarly, most evaluable patients have achieved full humoral reconstitution and have been able to discontinue Ig replacement and respond to vaccinations. These data suggest that once patients survive the procedure and engraft donor cells, relatively complete immune reconstitution is established. This observation is in striking contrast to the results of immune reconstitution after ERT. Reports suggest that, despite being well detoxified, patients on long-term PEG-ADA have T-cell numbers that are well below normal levels.23 The specific reasons for this are unclear, but data suggest that intracellular ADA expression either through transplantation of wild-type cells or GT of autologous cells corrects T-cell function more effectively than exogenous enzyme replacement.24 B-cell function and in particular antigen diversity is affected by the build up of dATP as a consequence of ADA deficiency.25 These defects are not fully repaired by ERT whereby only 50% of patients are able to discontinue Ig replacement therapy.16,26 After HCT, however, most patients are able to discontinue Ig replacement and make vaccine-specific responses, suggesting relatively complete humoral recovery.
The quality of long-term T-cell recovery is difficult to assess, given the limited data available. One intriguing question is whether unconditioned transplantations in MSD/MFD HCTs, which are highly successful in terms of survival outcome, will give rise to long-term thymopoiesis or whether the T-cell reconstitution seen is because of engraftment of mature T cells in the donor graft that will ultimately be exhausted leading to long-term T-cell compromise. The data available suggest the latter and show that TREC levels in most unconditioned procedures are at low levels, indicating that there has been only limited prethymic progenitor cell engraftment. T-cell immunity in the long term in these transplantations therefore depends on the pool of mature T cells with little or no thymic renewal. As yet there are no data to show that there are adverse clinical consequences of these findings in ADA-SCID, but these data emphasize that patients need to be followed carefully even 10-15 years after HCT.
Donor engraftment in the T-cell lineage was almost 100% in all patients regardless of the conditioning regime used. These results imply that there is a significant survival/proliferative advantage to wild-type T cells, which allows them to survive and expand to repopulate the T lymphoid compartment. It is known that detoxification through exogenous enzyme replacement will allow ADA-deficient T-cell development. In the transplantation scenario when detoxification has been achieved through engraftment of donor cells, there is little outgrowth of host ADA-deficient T cells, presumably because they are out-competed by donor T cells that express ADA, again suggesting that intracellular ADA expression is important for T-cell function and survival. An interesting finding in this study is that most of the 22 patients evaluated had significant levels of donor B-cell chimerism. Even in unconditioned procedures, 10 of 12 patients showed donor B-cell chimerism > 40%, suggesting that there may also be a survival advantage to ADA-expressing B lymphocytes. This is further supported by the increased level of B-cell to myeloid chimerism in several patients. Importantly, even those patients who lack B-cell chimerism were able to develop increased numbers of recipient B cells (presumably as a result of ADA produced in trans by engrafted donor T cells) and able to recover humoral immunity, suggesting donor B-cell chimerism is not an absolute prerequisite for functional humoral reconstitution.
The correction of nonimmunologic defects such as cognitive, behavioral, and audiologic abnormalities were not documented in sufficient detail in this retrospective data analysis to enable further comment. In the small studies that have been performed, donor source or conditioning did not affect cognitive, behavioral, or neurologic outcome,10,11,19 but larger prospective well-controlled studies need to be performed to look at influence of transplantation on these defects.
The results from this report have for the first time documented the different outcomes of transplantation for ADA-SCID from different donor sources and after different conditioning regimes, confirming the specific features of this disease with respect to other SCID variants. They show clearly the importance of donor matching in improving outcome and the poor outcome in mismatched transplantations. Clearly, given the good survival figures shown after GT procedures for ADA-SCID,14,16 mismatched transplantations should be undertaken only when other treatment options are not available. The outcomes for MSD and MFD transplantations even without conditioning are good and remain the treatment of choice. The choice of GT or matched unrelated transplantation remains open to discussion, given that at present GT offers 100% survival and ∼ 70% efficacy (defined by the need to restart enzyme replacement), whereas MUD transplantations offer ∼ 70% survival and 100% efficacy. As more patients are treated and data are collected for both procedures, this choice may become clearer.
The other striking feature highlighted by this report is the excellent immune reconstitution observed long term, both cellular and humoral, after HCT regardless of donor or transplantation type. These data also show that high levels of T- and B-cell donor chimerism are achieved even after unconditioned matched donor procedures and suggest that there is a survival advantage to ADA-expressing lymphoid cells. Thus, the important factor is that patients survive the transplantation procedure, for if that is achieved, near normal long-term cellular and humoral immune recovery can be expected.
One final issue to address is indeed whether it is more difficult to undertake transplantation for ADA-SCID than for other forms of SCID. In the MSD, MFD, and MUD settings the results both in terms of OS and immune recovery are comparable with what has been reported for all forms of SCID in several studies.17,18,27 In the HAPLO donor setting, the OS again mirrors the outcomes historically for other SCID forms (∼ 50% OS historically) with improvement in OS in the past decade.17,18 A main difference, however, that distinguishes ADA-SCID from T-B+ SCID is that in HAPLO transplantations, engraftment is unlikely to occur without cytoreductive conditioning and a high rate of rejection is seen. Conversely, one advantage that ADA-SCID may show over T-B+ SCID (namely SCID-X1 and JAK-3 SCID) and T-B− SCID forms is that humoral immune recovery is often achieved, even in the absence of donor B-cell engraftment.
There is an Inside Blood commentary on this article in this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The European Society for Immunodeficiencies registry helped to identify patients in the European database.
This work was supported by the Great Ormond Street Hospital Children's Charity (H.B.G.) and the Great Ormond Street National Institute for Health Research Biomedical Research Center.
The study was initiated by the Inborn Errors Working Party of European Group for Blood and Marrow Transplantation (IEWP EBMT).
Authorship
Contribution: H.B.G. and L.N. conceived the study and designed the questionnaire; A.H., C.B., A.B., and M.R. input data; Z. Allwood provided statistical help and analysis; P.V., K.R., M.H., W.F., A.G., M.S., R.B., A. Finocchi, C.C., A.A., F.P., A.L., C. Steward, A. Filipovich, R.M., V.B., S.A.-M., H.A.-M., Z. Alsum, H.A.-D., A.A.G., C. Speckmann, A. Fischer, N.M., K.E.M., E.G., D.A.Z., C.M.R., J.B., E.G.D., and M.C.-C. provided clinical care of patients, gathered patient data, and provided input into the writing of the paper; and A.H. and H.B.G. analyzed the data, produced the figures, and wrote the paper.
Conflict-of-interest disclosure: H.B.G. has been an occasional consultant for Enzon Pharmaceuticals Inc, a former manufacturer of PEG-ADA. The remaining authors declare no competing financial interests.
Correspondence: H. Bobby Gaspar, Molecular Immunology Unit, UCL Institute of Child Health, 30 Guilford Street, London WC1N 1EH, United Kingdom; e-mail: h.gaspar@ich.ucl.ac.uk.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal