Abstract
The antiphospholipid syndrome (APS) is defined by the persistent presence of antiphospholipid antibodies in patients with a history of thrombosis and/or pregnancy morbidity, including fetal loss. APS is an autoimmune disease with a confusing name because the pathologic auto-antibodies are shown to be directed against the plasma protein β2-glycoprotein I and not against phospholipids. In fact, auto-antibodies that recognize phospholipids themselves are not associated with thrombosis but with infectious diseases. One of the intriguing questions is why autoantibodies against β2-glycoprotein I are so commonly found in both patients and the healthy. Several potential mechanisms have been suggested to explain the increased thrombotic risk in patients with these autoantibodies. In this overview, we will summarize our knowledge on the etiology of the autoantibodies, and we will discuss the evidence that identify autoantibodies against β2-glycoprotein I as the culprit of APS.
Introduction
The existence of autoantibodies against β2-glycoprotein I (β2GPI) was described for the first time in 1990, when 3 different groups identified these antibodies as an important subpopulation of autoantibodies in patients with the antiphospholipid syndrome (APS).1-3 The plasma glycoprotein β2GPI consists of 326 amino acids, arranged in 5 highly homologous complement control protein domains, designated domain I to V from the N- to the C-terminus. The first 4 domains consist of approximately 60 amino acids each, whereas the fifth domain is larger because of a 6-residue insertion and a 19-residue C-terminal extension that constitute a phospholipid binding loop.4
APS is characterized by the presence of so-called “antiphospholipid” antibodies in plasma of patients experiencing thrombotic complications or pregnancy morbidity.5 At the time of the identification of β2GPI as an antigen in the syndrome, 2 other subpopulations of autoantibodies had already been identified as serologic markers: anticardiolipin antibodies, detected with an ELISA or a radioimmunoassay, and lupus anticoagulant (LA), detected as a prolongation of a phospholipid-dependent clotting test. The discovery that the anticardiolipin antibodies that are correlated with thrombotic complications are in reality autoantibodies that recognize β2GPI, which has a high affinity for cardiolipin, has been an important improvement in the development of diagnostics for the syndrome. This finding enabled the discrimination between β2GPI-dependent anticardiolipin antibodies that are correlated with thrombosis and fetal loss and β2GPI-independent anticardiolipin antibodies, whose presence seems to be innocent and that are often found in connection with infectious diseases.6
Soon after this discovery, it was established that autoantibodies against β2GPI can also have LA activity, highlighting the importance of antibodies directed against β2GPI for the syndrome.7,8 Although LA activity is caused by antiprothrombin antibodies in some patients,9 in additional studies investigators have shown that LA activity caused by anti-β2GPI antibodies correlates much stronger with a history of thrombotic complications.10,11 On the basis of these data, the presence of anti-β2GPI antibodies has been added to the official classification criteria for APS as the third serologic marker at a consensus meeting in Sydney in 2004.5
The classification criteria of APS are based on the combined results of many patient studies in which correlations were established between the presence of antiphospholipid antibodies in plasmas of patients and the occurrence of thromboembolic complications or pregnancy morbidity.5 Evidence for a causal connection between the presence of antiphospholipid autoantibodies and the observed clinical manifestations comes from experiments in animals in which the passive infusion of patient antibodies into pregnant mice resulted in reabsorbance of the fetuses and an increased thrombotic response after an experimental injury in otherwise-healthy mice.12 Additional experiments have shown that in particular autoantibodies against β2GPI are responsible for the enhanced thrombotic response.13 These studies have convinced most scientists that autoantibodies against β2GPI are the pathologic subpopulation of the antiphospholipid antibodies. Here, we review the evidence that anti-β2GPI antibodies are responsible for both the thrombotic and the pregnancy complications associated with APS, and we discuss why these autoantibodies are so commonly detected in both patients and the healthy.
The detection and specificity of autoantibodies against β2GPI
The anticardiolipin antibody ELISA, the anti-β2GPI antibody ELISA, and the LA assays detect overlapping, but different, populations of autoantibodies.14 The anticardiolipin antibody ELISA detects both antibodies directed against cardiolipin itself and antibodies against β2GPI, the anti-β2GPI antibody ELISA measures only antibodies against β2GPI, whereas LA assays can detect antibodies against both prothrombin and β2GPI, with the restriction that only a subpopulation of autoantibodies directed to β2GPI is able to induce a prolongation of a clotting assay. Because these 3 assays are used to measure different subpopulations of autoantibodies, they correlate differently with the clinical manifestations that determine APS. Many researchers have shown that LA assays are by far superior to the other 2 tests to detect the pathologic subpopulation of antiphospholipid antibodies.15-17 The correlation between thrombotic complications and anti-β2GPI or anticardiolipin antibodies is much weaker, and there are indications that patients with only a positive anti-β2GPI antibody ELISA do not have any clinical risk at all.17-19
This correlation is not easy to explain, considering the observation that passive transfer of anti-β2GPI autoantibodies into mice induces an increased thrombotic response.13 The most convincing explanation for this discrepancy is that there are different subpopulations of anti-β2GPI antibodies, each recognizing different epitopes on β2GPI and differing greatly in their pathologic effects. Indeed, it has been shown that antibodies that recognize domain I of β2GPI correlate much stronger with a history of thrombosis and pregnancy morbidity than antibodies that recognize other domains of β2GPI.20-22 Antibodies against domain V of β2GPI, often observed in leprosy, seem to be harmless.23 Autoantibodies against domain IV-V of β2GPI can be detected in young children without any sign of thrombotic events.24 Additional support for the importance of antidomain I antibodies comes from studies in mice in which injection of domain I attenuated the effects of antiphospholipid antibodies in a mouse model of APS.25 Moreover, antidomain I antibodies express LA activity.10 Apparently, antibodies that are directed against this domain score positive in all 3 assays. It is therefore not surprising that when all 3 assays for the detection of antiphospholipid antibodies are positive, the risk of recurrence of thrombotic complications is greatest.26 It should be noted that there might be different epitopes present on domain I.27 It is unknown whether autoantibodies specific for these individual epitopes harbor the same risk.
An important reason for the discrepancy between experimental data and epidemiologic studies is the poor standardization of the assays that are currently used to detect anti-β2GPI antibodies. Several surveys have shown that only the very high-titer anti-β2GPI antibodies are reliably detected, which depends in part on differences in protein preparations, surface immobilization, choice of microtiter plate, and blocking reagent.28 In particular, the presentation of β2GPI on the microtiter plate greatly influences the results.29 A popular way to obtain purified β2GPI is by perchloric acid precipitation, which might influence the integrity of the molecule.30 However, the use of perchloric acid–treated β2GPI resulted in steep calibration curves, indicating that the protein can be used as antigen in anti-β2GPI antibody ELISAs. It is important to use hydrophilic ELISA plates because the binding of β2GPI to these surfaces induces a conformational change that results in the presentation of the cryptic epitope to which the pathogenic antibodies are directed. The use of β2GPI from nonhuman sources is strongly discouraged because antibodies against bovine proteins are not uncommon in human blood.
The international classification criteria for APS include only the presence of IgG and IgM anti-β2GPI antibodies as part of the serologic criteria.5 This decision was determined by the results of epidemiologic and functional studies that were published at that time. Recent publications have questioned this decision.31-35 Additional studies have now been published in which the authors challenge the importance of IgM as a risk factor, and other studies have shown that IgA is associated with venous thrombosis and stroke. There are even studies in which investigators show that IgM protects against some of the clinical manifestations such as lupus nephritis.36 It is not easy to draw conclusions from all these conflicting observations. Aside from the fact that the assays to detect these autoantibodies are poorly standardized, there may be a difference in risk between patients with and without another underlying immune disease.35 Moreover, there may be an ethnic component to consider.37 Another factor that has to be taken into account is the affinity of the autoantibodies. Different studies have shown that particularly autoantibodies with greater affinity correlate with thrombosis.38,39 Some authors have suggested that the presence of anti-β2GPI antibodies should be measured in plasma diluted in 500mM NaCl to avoid the interference of the clinically irrelevant low-affinity antibodies.39,40 In summary, there is a general consensus that IgG is the important autoantibody that matters. In view of the conflicting publications, the importance of measuring IgM and IgA is unclear. As long as there are no conclusive studies, we suggest measuring them both but only consider medium- and high-titer antibodies as relevant.
Given all these uncertainties, one should be careful to interpret the results of an anti-β2GPI antibody ELISA. A combination of a positive anti-β2GPI antibody ELISA and a positive LA will identify patients at risk, whereas patients with a single positivity of anti-β2GPI antibodies should be considered at low risk for adverse clinical events. We strongly discourage the diagnosis of a patient only on the results of a single assay. The introduction of an ELISA specific for domain I of β2GPI could increase the specificity of the assay, probably at the expense of the sensitivity because we do not know whether this assay will identify all pathogenic autoantibodies.
The etiology of autoantibodies against β2GPI
Infection-related antiphospholipid antibodies are thought to interact directly with cardiolipin, independent of the presence of β2GPI, and they are considered not to be related to an increased risk of thrombosis.36 An increasing number of publications also describe autoantibodies against β2GPI in combination with infections.41-43 The eminence-based consensus is that these infection-related antibodies are distinct from the autoantibodies identified in APS patients,44 although there is not much scientific evidence that these infection-related autoantibodies are indeed different from APS-related autoantibodies. Infection-related anti-β2GPI antibodies circulate for a short period of time. The increased risk of thrombosis of patients with persistently present anti-β2GPI antibodies can be explained in part by the circulation time of the autoantibodies. Gharavi et al have shown that immunization with peptides derived from cytomegalovirus induced LA activity and resulted in thrombotic complications.41 Moreover, the presence of anti-β2GPI antibodies has been reported in patients with cytomegalovirus infections who developed thrombosis.45
Many publications link the etiology of autoantibodies to a molecular mimicry mechanism.46 Sequence similarities between foreign and self-peptides are considered to be sufficient to activate auto-reactive T and B cells with pathogen-derived peptides. Anti-β2GPI antibody formation is induced when mice are immunized with viral peptides, suggesting sequence or conformation similarities between the bacterial and viral peptides and amino acid sequences of β2GPI.47 However, mice and rabbits boosted with the anionic phospholipids cardiolipin and phosphatidylserine or with lipopolysaccharide also develop autoantibodies against β2GPI, demonstrating that molecular mimicry cannot be the only explanation for the etiology of these autoantibodies.48,49 Considering the ease with which these autoantibodies are formed after infections with a large number of dissimilar microorganisms (Table 1),50,51 there must be a more fundamental background for the frequent presence of these autoantibodies in the circulation.
Infectious diseases associated with the presence of autoantibodies against β2GPI
| Viruses | Parvovirus B19 |
| Cytomegalovirus | |
| Human immunodeficiency virus | |
| Varicella-zoster virus | |
| Epstein-Barr virus | |
| Hepatitis B/C | |
| Adenovirus | |
| Human T-lymphotropic virus type I | |
| Bacteria | Streptococcus pyogenes |
| Staphylococcus aureus | |
| Helicobacter pylori | |
| Salmonella typhi | |
| Mycobacterium leprae | |
| Escherichia coli | |
| Rickettsia typhi | |
| Mycobacterium leprae | |
| Mycobacterium tuberculosis | |
| Coxiella burnetii | |
| Chlamydophila psittaci | |
| Mycoplasma | Mycoplasma pneumoniae |
| Parasites | Plasmodium falciparum |
| Borrelia burgdorferi | |
| Leptospirosis | |
| Leishmania |
| Viruses | Parvovirus B19 |
| Cytomegalovirus | |
| Human immunodeficiency virus | |
| Varicella-zoster virus | |
| Epstein-Barr virus | |
| Hepatitis B/C | |
| Adenovirus | |
| Human T-lymphotropic virus type I | |
| Bacteria | Streptococcus pyogenes |
| Staphylococcus aureus | |
| Helicobacter pylori | |
| Salmonella typhi | |
| Mycobacterium leprae | |
| Escherichia coli | |
| Rickettsia typhi | |
| Mycobacterium leprae | |
| Mycobacterium tuberculosis | |
| Coxiella burnetii | |
| Chlamydophila psittaci | |
| Mycoplasma | Mycoplasma pneumoniae |
| Parasites | Plasmodium falciparum |
| Borrelia burgdorferi | |
| Leptospirosis | |
| Leishmania |
For additional information, see Sherer et al.47
There is a growing body of evidence that antiphospholipid antibodies, including anti-β2GPI antibodies, belong to the natural antibody repertoire.52-55 Natural antibodies are defined as antibodies that are present in the circulation before an antigen stimulus. Natural antibodies have been described as poly-reactive, that is, they can react with several unrelated antigens, including self-antigens. These natural antibodies seem to bind primarily to pathogenic structures that are well conserved and present in many species, such as clusters of charge, and they are usually of low affinity. Antiphospholipid antibodies have similar characteristics. As part of the innate immune system, the presence of natural antibodies must have a fundamental benefit, although they may cross-react with self-antigens.56 If anti-β2GPI antibodies belong to the natural antibody repertoire, this means that they are present for a purpose and that they could play a role in the innate immune response.54 Support for the identification of antiphospholipid antibodies as natural antibodies comes from the observation that healthy persons without APS can have memory B cells that produce antiphospholipid antibodies.57 In several elegant studies, Fleming et al have shown that natural anti-β2GPI antibodies are involved in complement-mediated mesenteric ischemia/reperfusion-induced injury.58,59 In addition, there are also indications that natural antiphospholipid antibodies are involved in acute graft rejection after renal transplantation.60 Natural antibodies are thought to play a role in the clearance of apoptotic bodies and there is convincing evidence that β2GPI and anti-β2GPI antibodies are essential for the clearance of these cell remnants.61,62 Recent epidemiologic studies in a large cohort of patients with systemic lupus erythematosus (SLE) have shown that the presence of anti-β2GPI IgM protects against lupus nephritis.35 Up to 5% of the healthy population has antiphospholipid antibodies, and these autoantibodies seem to be benign and of low affinity. All these observations suggest that many healthy patients have low-titer and low-affinity natural anti-β2GPI antibodies in their circulation and that the prevalence of these antibodies grows with age.63
The natural antibody repertoire may comprise 2 major subsets, an overt antibody population and a cryptic or latent population.64 The unmasking of these cryptic natural antibodies in vitro has been observed via the use of high-salt solution, low pH, or oxidative agents. Indeed, patients who are negative for antiphospholipid antibodies can become positive after oxidation-reduction reactions and vice-versa.65 In addition, the plasma of healthy persons becomes positive after it is heated to 56°C.66 Apparently, small changes or slight modulations within the antibody binding site can change epitope recognition.
The cause of the transition of these natural antibodies against β2GPI from benign to pathogenic antibodies remains elusive. Natural antibodies may, under certain circumstances, begin to modulate to pathologic autoantibodies via an antigen-driven selection of certain populations of B cells. In some studies authors have shown that infections contribute to the maturation of the immune system from low-titer and low-affinity antibodies to full blown autoantibodies.64 The further induction of autoantibodies against β2GPI may strengthen the efficacy of β2GPI as part of our defense mechanism. This latter suggestion is supported by the observation that the epitope recognized by the autoantibodies against β2GPI is completely conserved in mammalian evolution.67 Loss of tolerance can occur after sudden exposure to an antigen.
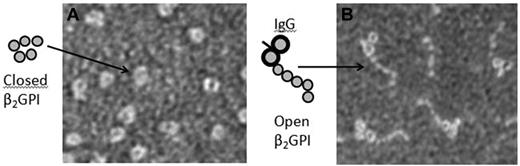
Interestingly, lymphocytes are not continuously exposed to antigenic stimulation in healthy patients because the epitope within β2GPI that is recognized by the pathogenic subpopulations of autoantibodies is cryptic. β2GPI is a protein that can adopt different conformations (Figure 1).68,69 In the presence of anionic phospholipids, lipopolysaccharide, or hydrophilic surfaces, the circular conformation of the protein unfolds, exposing antigenic determinants that are normally shielded from the circulation.70 One of these “cryptic” antigenic determinants is the epitope for the pathologic autoantibodies present in domain I of β2GPI.20-22 Infectious diseases can result in the binding of β2GPI to pathogens, resulting in exposure of an epitope in domain I and stimulation of T and B cells. This hypothesis is strengthened by the observation that binding of β2GPI to protein H, a membrane protein of Streptococcus pyogenes, results in the conformational change of β2GPI from the circular to the open conformation. Injection of mice with protein H results in induction of autoantibodies against murine β2GPI with LA activity.70 Further support comes from the observation that injection with murine domain I induces autoantibodies against β2GPI in these mice, whereas injection with domains II through V does not result in an immune response.71 All these experiments show that exposure of mice to this cryptic epitope within domain I of β2GPI results in an up-regulation of autoantibody production.
β2-glycoprotein I changes conformation on antibody binding. Scanning electron microscopy images showing plasma β2-GPI (A) and β2-GPI in complex with antibodies against domain I of β2-GGI (B). Samples were visualized using a Jeol JEM 1230 transmission electron microscope operated at 60 kV accelerating voltage and recorded with a Gatan Multiscan 791 CCD camera using the software provided by the manufacturer (magnification 200 000×).
β2-glycoprotein I changes conformation on antibody binding. Scanning electron microscopy images showing plasma β2-GPI (A) and β2-GPI in complex with antibodies against domain I of β2-GGI (B). Samples were visualized using a Jeol JEM 1230 transmission electron microscope operated at 60 kV accelerating voltage and recorded with a Gatan Multiscan 791 CCD camera using the software provided by the manufacturer (magnification 200 000×).
There are 4 β2GPI allelic variants known, of which the Val247Leu variant has attracted most attention. A meta-analysis has shown that patients with APS have a greater prevalence of the Val/Val genotype and that the presence of this variant is correlated with the presence of anti-β2GPI antibodies.72 It has been suggested that the tertiary structure of the Val247 variant of β2GPI differs from that of the Leu247 variant. Model systems suggest a loss of electrostatic interaction between Glu228 in domain IV and Lys308 in domain V in the Val247 variant, which may influence the stability of the circular plasma conformation.73 An increased tendency of β2GPI to open up and to expose the epitope for anti-β2GPI antibodies can explain the observed risk to develop autoantibodies against β2GPI in Val/Val carriers.
Recently, evidence has been brought forward that a part of β2GPI circulates in a reduced form with free surface-exposed thiol groups and that the percentage of reduced β2GPI is much greater in patients with APS.74 Binding studies have shown that the avidity of patient-derived autoantibodies is significantly greater for reduced β2GPI than for oxidized β2GPI.75 The authors hypothesize that oxidative stress lowers the threshold for the development anti-β2GPI antibodies. Alternatively, oxidation of β2GPI might favor a conformational change from the circular to the stretched conformation of β2GPI, resulting in exposure of cryptic epitopes and an enhanced antigen driven B-cell maturation.
The pathophysiology of the autoantibodies
Thrombotic events only take place every now and then in patients with antiphospholipid antibodies, despite the continuous presence of these antibodies in the circulation. This finding suggests that there are additional factors that determine whether thrombosis will occur. The current consensus is that a second hit is necessary to unveil the prothrombotic activity of antiphospholipid antibodies. The exact nature of this priming event, a perturbation of the endothelial lining of the vasculature, an increased inflammatory state, or something completely different, is unclear. Experimental data obtained in animal models of APS support the second hit hypothesis. Passive infusion of human IgG that was purified from patients with APS into mice only results in excessive thrombus formation on induction of a mechanical or chemical vascular injury.76,77 Likewise, rats only develop occlusive thrombi on infusion with human antiphospholipid antibodies when primed with endotoxin.78
Antiphospholipid antibody-associated thrombosis can occur throughout the body in every type of vessel—vein, artery, or microcirculation, although deep-vein thrombosis and ischemic stroke are most frequently observed.79 Thrombosis in APS has been attributed to antibody-mediated interference with several aspects of the coagulation system, such as the fibrinolytic pathway80 or the protein C axis.81 These suggestions offer unlikely explanations for the diffuse thrombotic diathesis observed in the APS because plasminogen deficiency is not associated with a thrombotic tendency, and deficiencies of regulators of coagulation are generally associated with vascular bed–specific thrombosis. However, we cannot exclude the possibility that the presence of the autoantibodies disturbs different metabolic pathways, which may operate under different conditions or in different patient groups. Nevertheless, a much more likely target-candidate for antiphospholipid antibodies would be a cellular component of the blood, including the endothelial lining of the vasculature. Indeed, activation of platelets, monocytes and endothelial cells by antiphospholipid antibodies in general and anti-β2GPI antibodies in particular, has been shown extensively (Figure 2). The prominent read-out for cell activation was the induction of the surface expression of procoagulant tissue factor.82 An interesting option is that budding of tissue factor containing microparticles from monocytes or endothelial cells could explain a more generalized increase in a risk for thrombotic complications.83
Sequence of events leading to cellular activation by β2GPI-antibody complexes. β2GPI is not recognized by pathologic anti-β2GPI antibodies in the circulation. When negatively charged, phospholipids become exposed, and β2GPI will bind to this surface and change conformation. This step exposes a cryptic epitope in domain I that is recognized by the pathologic antibodies. The antibody fixes β2GPI in this conformation, and the antibody–β2GPI complex can subsequently interact with several surface receptors, such as glycoprotein Ibα (GPIbα), LRP8, annexin A2, and several members of the TLR family (TLR2, -4, and -8). Because receptor and phospholipid binding are mutually exclusive, the β2GPI–antibody complex probably dissociates from the surface before it can interact with a surface receptor.
Sequence of events leading to cellular activation by β2GPI-antibody complexes. β2GPI is not recognized by pathologic anti-β2GPI antibodies in the circulation. When negatively charged, phospholipids become exposed, and β2GPI will bind to this surface and change conformation. This step exposes a cryptic epitope in domain I that is recognized by the pathologic antibodies. The antibody fixes β2GPI in this conformation, and the antibody–β2GPI complex can subsequently interact with several surface receptors, such as glycoprotein Ibα (GPIbα), LRP8, annexin A2, and several members of the TLR family (TLR2, -4, and -8). Because receptor and phospholipid binding are mutually exclusive, the β2GPI–antibody complex probably dissociates from the surface before it can interact with a surface receptor.
Transmission of activation signals across cell membranes usually involves ligand-receptor interactions and it is therefore not surprising that the identification of the receptor(s) that mediate the prothrombotic effects of antiphospholipid antibodies is subject of ongoing investigations. Several receptors have been reported thus far to interact with the β2GPI-antibody complex, among others TLR2,84 TLR4,85,86 TLR8,87 annexin A2,88 glycoprotein Ibα,89,90 and the low-density lipoprotein (LDL)–receptor family member LDL receptor–related protein (LRP)–8, also known as ApoER2.91 Activation of cell lines or cells isolated from blood with antiphospholipid antibodies indicates involvement of each of these receptors in the induction of a prothrombotic cellular phenotype in a β2GPI-dependent manner. Studies with murine thrombosis models confirm the roles of TLR4,92 annexin A2,93 or LRP8,76,77 as inhibition or absence of individual receptors results in an ameliorated thrombotic phenotype on challenge with antiphospholipid antibodies. Because none of these individual deficiencies reduces the thrombotic phenotype to baseline, we cannot exclude a cooperative effect between receptors in the pathophysiology of the syndrome.
Few data are available on the mechanism behind the adverse effects of antiphospholipid antibodies on pregnancy outcome. Antiphospholipid antibodies are reported to interfere with placentation,94,95 which might lead to placental insufficiency. Increased rates of placental thrombosis have been observed in women with antiphospholipid antibodies,96,97 which might be explained by either disruption of the annexin a5 shield that prevents the interaction between the coagulation system and the phosphatidylserine exposing syncytiotrophoblast surface98 or by a disproportionate inflammatory response that involves activation of the complement system and formation of the anaphylatoxin C5a.99
Data that support a role for the complement system in the pathophysiology of APS are more ambiguous. F(ab′)2 fragments of anti-β2GPI monoclonal antibodies retain the same prothrombotic potential as the full-length antibody in a hamster thrombosis model.100 This renders involvement of the Fc-mediated classic pathway of complement activation unlikely, although a contribution of this pathway to antiphospholipid antibody mediated effects cannot be fully excluded. Murine models of fetal loss, however, clearly indicate a role for the classic pathway in antiphospholipid antibody mediated pathology.99 This discrepancy can be explained to some extend by the high concentrations of total human IgG used in these studies, although similar amounts of IgG obtained from healthy controls had no effect on fetal loss. Moreover, complement deposition on circulating immune complexes is a prominent feature of SLE, a frequent comorbidity of APS. Further evidence for involvement of the complement system comes from studies that show that deficiency of either C3 or C5 protects from both antiphospholipid antibody-induced thrombosis101 and fetal loss.99,102 If there is a role for the complement system in APS, then the sustained effects of F(ab′)2 fragments of anti-β2GPI antibodies in combination with a role for C3 and C5 point in the direction of the alternative pathway of complement activation. This notion is strengthened by the protective effects of factor B deficiency on fetal loss.99
Attenuation of the activity of the autoantibodies
Currently prescribed thromboprophylaxis for patients with APS are antiplatelet agents, heparins, vitamin K antagonists, or combinations thereof. All of these drugs share the major disadvantage of a substantially increased risk of bleeding. This holds true for the use of vitamin K antagonists, considering patients with antiphospholipid antibodies are often treated for a longer period and with a target international normalized ratio of 3 or greater. It is therefore not surprising that a large amount of effort is being put in the development of better-tailored treatment strategies that do not have the adverse side-effects associated with anticoagulants. Solving the crystal structure of β2GPI has been the first step on the way to a deeper understanding of the biochemical mechanisms behind the interaction between β2GPI and antibodies, phospholipid surfaces, and receptors. This has allowed the design of tools that specifically antagonize the interaction between either β2GPI and antiphospholipid antibodies, or receptors and β2GPI-antibody complexes.
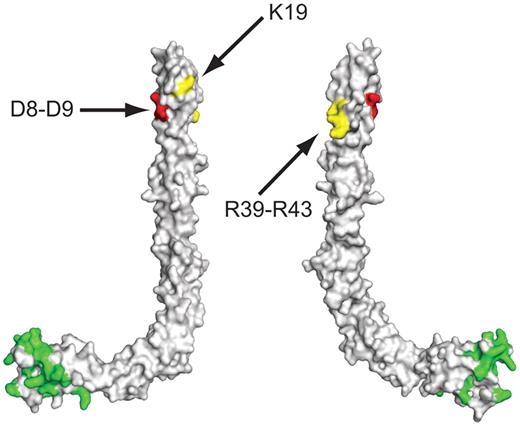
The primary antigenic epitope of anti-β2GPI antibodies resides in domain I and spans residues Arg39 to Arg43 (Figure 3).22,103 The identification is based on the strong attenuation of the binding of patient-derived antibodies to immobilized β2GPI in which these residues are mutated. Moreover, the presence of antibodies that interact with this region is strongly associated with thrombosis.10 Another putative antibody-binding site is located at the opposite side of the domain, in the region surrounding Lys19. Mutation of this residue has similar inhibitory effects on antibody binding—albeit less pronounced,103 but the relevance of antibodies that recognize this region remains to be determined. Interestingly, mutation of residues Asp8 and Asp9 in domain I increases antibody binding in the fluid phase.22 In fact, injection of domain I mutated at these residues neutralizes the prothrombotic effects of human antiphospholipid antibodies in a murine thrombosis model more effectively than infusion of wild-type domain I,25 which indicates its potential applicability as a therapeutic agent. Nevertheless, even though attenuation of the prothrombotic effects of antiphospholipid antibodies at the level of the interaction between antigen and antibody seems to be an attractive idea, it is important to realize that injection of domain I might not be without risk because it has been shown to lead to further immunologic priming toward β2GPI.71
Residues in the crystal structure of β2-GPI that are involved in the interaction with ligands. Domain I contains 2 primary antibody binding sites (highlighted in yellow): the region around Lys19 and the region spanning Arg39 to Arg43. Mutation of residues Asp8 and Asp9 (highlighted in red) enhances the binding of antiphospholipid antibodies to domain I. Domain V contains the phospholipid binding site, which overlaps with the site that interacts with LA1 of LRP8 (highlighted in green).110
Residues in the crystal structure of β2-GPI that are involved in the interaction with ligands. Domain I contains 2 primary antibody binding sites (highlighted in yellow): the region around Lys19 and the region spanning Arg39 to Arg43. Mutation of residues Asp8 and Asp9 (highlighted in red) enhances the binding of antiphospholipid antibodies to domain I. Domain V contains the phospholipid binding site, which overlaps with the site that interacts with LA1 of LRP8 (highlighted in green).110
The phospholipid binding site is located within the fifth domain of β2GPI. It has been mapped to the hydrophobic loop at the C-terminus of the domain and includes a large positively charged patch of Lysine residues. Mutations in this region,104,105 or cleavage of this hydrophobic loop by proteases such as plasmin,106 greatly reduce the capacity of β2GPI to interact with phospholipids. Interestingly, the lysine-rich region in β2GPI is highly homologous to a 20-amino acid peptide derived from an uncharacterized protein of cytomegalovirus (TIFILFCCSKEKRKKKQAAT). This peptide, referred to as TIFI, effectively competes with β2GPI-antibody complexes for binding sites on cellular surfaces.107 Coinjection of TIFI and antiphospholipid antibodies prevents excessive thrombus formation on a mechanical vascular injury,108 and TIFI-treatment of pregnant mice that were injected with human antiphospholipid antibodies significantly reduces fetal resorption rates.107 It should be noted, however, that immunization of mice with TIFI induces the generation of prothrombotic antiphospholipid antibodies,41 which precludes its applicability as a therapeutic agent in the syndrome.
β2GPI also interacts with cellular receptors via its fifth domain, but this interaction has only been studied in detail for LRP8. Biochemical analysis has shown that domain V interacts with the first LDL type A (LA) module of LRP8.109 Solution nuclear magnetic resonance spectroscopy has identified the residues in both LRP8 and domain V of β2GPI that are perturbed when both proteins interact.110 Interestingly, the epitope in domain V that interacts with LA1 of LRP8 involves several positively charged residues, including the positively charged patch of lysine residues that are essential for phospholipid binding. In fact, receptor binding and interaction with phospholipids are mutually exclusive. This has led to the development of an artificial dimer of LA1 of LRP8, which effectively inhibits the binding of β2GPI-antibody complexes to phospholipid surfaces.111 The efficacy of soluble LA1 of LRP8 as an inhibitor of the prothrombotic effects of antiphospholipid antibodies has been shown extensively both in vitro77,90,112 and in vivo.76 However, LDL-receptor family members are ubiquitous and are involved in several important processes, including protein clearance, lipoprotein metabolism and neuronal plasticity. Treatment with isolated LA modules might interfere with any of these processes, which makes unwanted off-target side-effects more than likely.
One of the most promising candidate drugs for treatment of APS is hydroxychloroquine, an antimalarial agent already used extensively for the treatment of SLE. Hydroxychloroquine effectively blocks the interaction between β2GPI and phospholipids113 and prevents the binding of antibody-β2GPI complexes to cells.114 Moreover, treatment with hydroxychloroquine ameliorates the prothrombotic effects of antiphospholipid antibodies in a murine thrombosis model,115 although these effects can also be mediated by the antiplatelet properties of the drug.116 Clinical trials should provide us with information on the efficacy of the drug as an antithrombotic agent in APS.
Because APS is an antibody-mediated disorder, anti–B-cell therapy might hold promise for the future. Data on the efficacy of anti–B-cell agents such as rituximab, however, are mostly limited to case reports. Further studies are needed before any conclusions can be drawn.
Concluding remarks
There is an increasing body of evidence that the presence of anti-β2GPI antibodies has a physiologic relevance and that they play different roles in innate immunity. These probably advantageous autoantibodies deteriorate into pathologic risk factors when their residence time in the circulation becomes indefinite and their avidity increases. The triggers that cause the transition from low-affinity temporary antibodies to greater-affinity persistent antibodies are unknown. Significant progress has been made since 1990, the year that the autoantibodies against β2GPI were first described, in our understanding of how the presence of these autoantibodies can cause the clinical manifestations that characterize APS. Experiments in animals have revealed that several cell types, such as endothelial cells, monocytes, and platelets, change their phenotype toward a more prothrombotic and proinflammatory state in the presence of these autoantibodies. Fundamental insight at the molecular level on how β2GPI interacts with its autoantibodies, the consequences of these interactions for the structure of β2GPI, and the newly acquired properties of structurally altered β2GPI to interact with phospholipids and cellular receptors is necessary to design new drugs for a better-tailored treatment of patients with APS.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors gratefully acknowledge Dr Matthias Mörgelin (Lund University, Lund, Sweden) for his help with the acquisition of electron micrographs.
R.T.U. is supported by a grant from the Dutch Heart Foundation (grant 2010T068).
Authorship
Contribution: P.G.d.G. and R.T.U. contributed equally to writing this review article.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Philip G. de Groot, University Medical Center Utrecht, Department of Haematology (G03.550), Heidelberglaan 100, 3584 CX Utrecht, The Netherlands; e-mail: ph.g.degroot@umcutrecht.nl.