Abstract
Hematopoietic cell transplant (HCT) is presumed to be more effective than chemotherapy alone for children with poor-risk AML in first complete remission (1st CR). The limited number of poor-risk children on individual studies has previously precluded a comparison of outcomes for those treated with chemotherapy compared to HCT.
We compared relapse, survival and treatment related mortality (TRM) among children with poor-risk AML treated with chemotherapy, matched related (MRD), or unrelated (URD) transplantation in 1st CR from 1989–2005. Bone marrow was the primary graft source but children also received peripheral blood stem cell and umbilical cord blood transplants. Poor-risk cytogenetics was defined by monosomy 7, deletions of 7q, monosomy 5, deletions of 5q, abnormalities of 3q, t(6;9)(p23;q34), or complex karyotype: defined as five or more cytogenetic abnormalities. Children treated with chemotherapy alone were drawn from Children's Oncology Group studies: CCG 2891, POG 9421, CCG 2941, CCG 2961, and AAML 03P1. Transplant recipients were drawn from these COG studies (MRD only) and the Center for International Bone Marrow Transplant Research registry (MRD and URD) during the same period.
The study included 234 children aged less than 21 years; 124 patients received chemotherapy alone, 55 patients MRD, and 55 patients URD transplant. Children in the chemotherapy group were more likely to be younger than 2 years of age, to be African-American, and to have a complex karyotype than children treated with HCT (p <0.001). More children treated with HCT had monosomy 7/7q- (p<0.001). African-American race was associated with higher mortality (HR = 2.12, p = 0.002) and higher relapse (RFS HR = 2.80, p<0.001) risks in univariate analysis. Older age (>11 years) was associated with higher mortality (p=0.05). Neither monosomy 7/7q- nor complex cytogenetics was significantly associated with survival on univariate analysis.
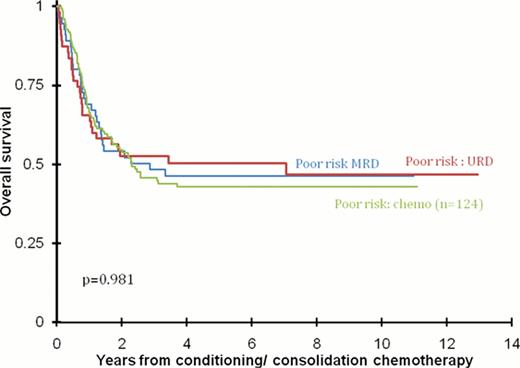
Overall survival at 5 years from the start of conditioning or consolidation chemotherapy was not significantly different for those treated with chemotherapy alone [43% + 9%], MRD HCT (46% +14%), or URD HCT (50% +14%), p = 0.98. However, the pattern of failure differed. Relapse rates were lower after URD transplants and transplant-related mortality rates higher after MRD and URD transplants. The 5-year cumulative incidence of relapse was 58% + 9%, 49% + 13% and 30% +12%, after chemotherapy, MRD, and URD transplant respectively (p=0.003). The corresponding 5-year treatment related mortality rates were 11% +6%, 15% + 10%, and 23% + 11% (p=0.04).
The multivariate analysis, after adjusting for race and age, confirmed the absence of differences in overall mortality; (reference group=chemotherapy alone;) MRD, hazard ratio [HR] 1.07, p=0.78) and URD, HR 1.02, p=0.95). The relapse risk was lower after URD transplants (HR 0.54, p=0.03) but not MRD transplants (HR 0.87, p=0.56). TRM was not significantly higher after MRD (HR 1.34, p=0.55) or URD (1.78, p=0.20).
The comparable survival observed after chemotherapy and transplantation for children with poor risk AML in CR1 does not support a role for allogeneic transplantation in these patients. Regardless of treatment received, African Americans had higher relapse and mortality risks and patients older than 11 years, higher mortality.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal