Abstract
Allogeneic stem cell transplantation (alloSCT) remains the only curative therapy for patients with indolent B cell non-Hodgkin's Lymphoma (B-NHL) as well as patients with aggressive B-NHL that have failed prior autologous stem cell transplants (ASCT). Non-myeloablative (NMA) alloSCT has been universally implemented for B-NHL given the extensive prior therapy and advanced age of the typical patient undergoing alloSCT for these diseases and resultant 40–50% incidence of transplant-related mortality (TRM) with myeloablative conditioning per registry series'. NMA alloSCT relies on graft-versus-lymphoma (GVL) effect for disease control. While the literature has suggested improved event-free survival (EFS) for B-NHL patients with a negative fluorine-18-deoxyglucose positron emission tomography (FDG-PET) scan prior to ASCT in chemosensitive patients, this has not been elucidated in a conventional NMA alloSCT treatment platform. Our hypothesis is that FDG avidity pre-NMA alloSCT is not prognostic to progression-free survival (PFS) in chemosensitive patients with B-NHL.
This is a retrospective study of adult B-NHL patients with disease assessed by CT and FDG-PET prior to undergoing a T-cell replete NMA alloSCT from a 9/10 or 10/10 HLA matched related or unrelated donor conditioned with cyclophosphamide 50 mg/kg x1, fludarabine 25 mg/m2 daily over 5 days and 2 Gy total body irradiation, with or without peri-allo-SCT rituximab 375 mg/m2 administered approximately day (d) -8, d+21, d+28, d+25, d+42 as per an internal protocol. Patients receiving an unrelated donor graft received equine anti-thymocyte globulin 30 mg/kg administered daily d-3 and d-2. Graft-versus-host disease (GVHD) prophylaxis consisted of tacrolimus, sirolimus and methotrexate (n=51) or cyclosporin-A and mycophenolate mofetil (n=15). Event-free survival (EFS) was calculated using Kaplan-Meier method. An event is defined as progression of disease (PD) or death from any cause.
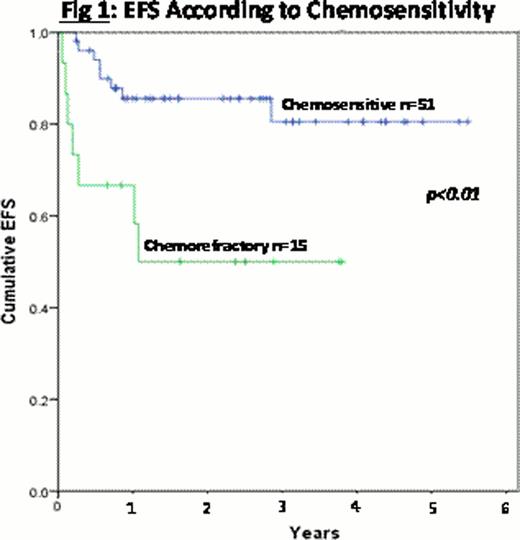
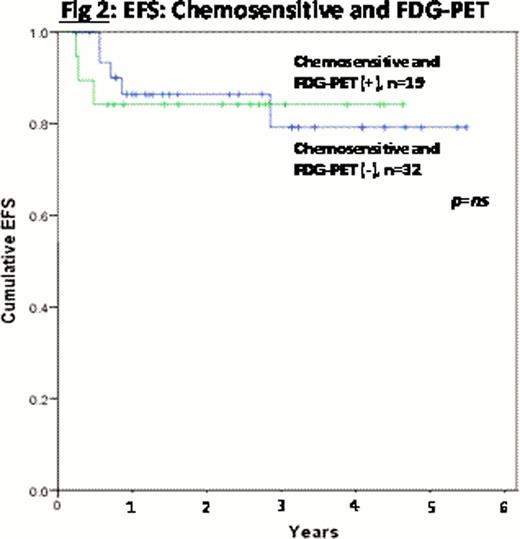
This analysis includes 66 patients with a median age of 54 (range 33–69) years at the time of allo-SCT. Diagnoses included: 16 CLL/SLL, 30 FL, 11 DLBCL/transformed B-NHL, 6 MCL and 3 other. Patients were previously treated with a median of 3 prior chemotherapy regimens (range 1–6) and 12 patients had undergone a previous ASCT. Fifty-one patients (77%) were chemosensitive at the time of alloSCT by CT criteria, as defined by either a complete or partial remission (Cheson et al, JCO 1999; Hallek et al, Blood 2005 for CLL/SLL). Of these 51 patients, 18 had FDG-avidity on FDG-PET at time of allo-SCT above liver background per Deauville criteria (Meignan et al, Leukemia and Lymphoma 2009). The median hematopoietic comorbidity index (HCT-CI) was 1 (range 0–8). Twenty-six patients received a graft from a 10/10 HLA matched related donor, 34 from a 10/10 HLA matched unrelated donor and 6 from a 9/10 HLA mismatched unrelated donor. Eighty-six percent of the patients received peri-alloSCT rituximab. The median follow-up for survivors is 29 (range 3–67) months. Of the 15 events, 10 were TRM (7 GVHD-related deaths) and 5 PD (3 chemosensitive patients and 2 chemorefractory patients pre-alloSCT). Only 1 event has occurred beyond 13 months. The estimated 2 year EFS is 77%. There was no difference in EFS according to: CR vs PR, graft source, number of previous lines of therapy, GVHD prophylaxis, peri-alloSCT rituximab, previous ASCT, or HCT-CI. The estimated EFS at 2 years for chemosensitive patients per CT criteria is 86% compared to 50% for patients without chemosensitivity pre-allo-HCT (figure 1, p<0.01). FDG-PET (+) was not prognostic in the chemosensitive patients prior to alloSCT (figure 2, p=ns). Only 2 of the 15 non-chemosensitive patients were FDG-PET (−) at time of alloSCT. Both of these patients had CLL/SLL and are event-free at 20 and 35 months post-alloSCT.
Chemosensitivity prior to T-cell replete NMA alloSCT for B-NHL predicts outcome post-transplant. FDG-PET scan did not add prognostic value to patients deemed chemosensitive by traditional CT criteria in our dataset. The majority of the events were TRM, which needs to be taken into consideration when interpreting these results. Transplant related mortality, especially GVHD related, continues to greatly impact survival of B-NHL patients undergoing NMA alloSCT.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal