Abstract
Abstract 4016
Multiple Myeloma (MM) is an incurable plasma cell malignancy accounting for 11,000 deaths annually in the US and 20% of deaths from all hematological malignancies. MM is one of myriad malignancies exhibiting enhanced glucose consumption associated with an aerobic glycolytic phenotype (i.e. the Warburg effect). We have recently published a study defining key glucose transporters responsible for facilitating glucose entry in myeloma and observed that MM cells exhibit reliance on constitutively cell surface-localized GLUT4 for basal glucose consumption. MM cells cultured in the absence of glucose or upon GLUT4 suppression exhibit either overt apoptosis (sensitive phenotype) or growth arrest (resistant phenotype). To further demonstrate the clinical utility of targeting GLUT4 for MM therapy we tested a HIV protease inhibitor ritonavir that has an off-target inhibitory effect on GLUT4. Treatment of MM cells with physiologically achievable concentrations of ritonavir blocks glucose entry resulting in MM cell death or growth suppression.
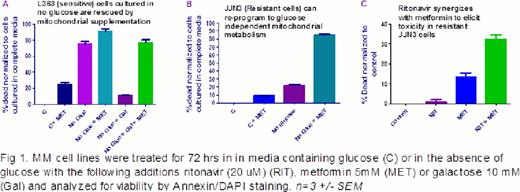
The objective of this study was to define those metabolic pathways in resistant MM cell lines which compensate for the decrease in cellular glucose and protect the cells from toxicity caused by glucose-deprivation or GLUT4 suppression. We hypothesized that resistant cells (i.e. JJN3) cultured in the absence of glucose revert to mitochondrial metabolism or autophagy to prevent cell death. The autophagy inhibitor chloroquine did not sensitize resistant cells cultured in the absence of glucose, ruling out autophagy as a source of compensatory metabolites. We next established that the mitochondrial substrates 2-methyl pyruvate or galactose rescue sensitive cells from toxicity caused by culture in the lack of glucose (Fig. 1A). These results suggest the potential for mitochondrial metabolism to rescue cell death ensuing upon inhibition of glycolysis. We therefore treated the resistant JJN3 cells with mitochondrial inhibitors metformin or rotenone to determine if we could elicit toxicity upon glucose-withdrawal. Indeed, resistant cells were sensitized to glucose-withdrawal upon treatment with complex 1 inhibitors metformin (Figure 1B) or rotenone. Metformin treatment alone had a minimal impact on the viability of resistant cells cultured in the presence of glucose (Fig. 1B). To simulate glucose-withdrawal we tested the ability of ritonavir (HIV protease inhibitor that has an off target inhibitory effect on GLUT4) to elicit toxicity in combination with metformin in the resistant cells. Our studies revealed that addition of ritonavir with metformin synergizes to elicit toxicity in resistant cells (Fig. 1C). This synergy was also observed in additional MM cell lines (KMS11 and U266). The biguanide metformin is the most commonly prescribed anti-hyperglycemic drug for the treatment of Type II diabetes. Epidemiologic studies have correlated metformin with a reduced risk of cancer in diabetics earning the drug recognition as a possible anti-neoplastic agent for various types of malignancies. This combinatorial regimen of ritonavir and metformin was not toxic in normal PBMC. The selective tumor specific synthetic lethality induced in ritonavir treated resistant cells upon metformin treatment is detected at doses that are clinically achievable with both compounds. We have initiated studies to evaluate this combination in mouse models of myeloma and patient samples. HIV patients chronically treated with ritonavir who exhibit diabetic symptoms have been treated with metformin indicating this combination treatment is well tolerated in humans. Our studies reveal a potent combinatorial regimen involving repurposed, FDA approved, ritonavir and metformin for the treatment of MM and potentially other glucose-driven malignancies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal