Abstract
Abstract 4132
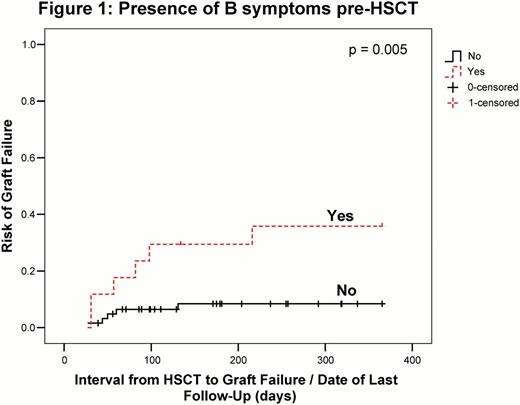
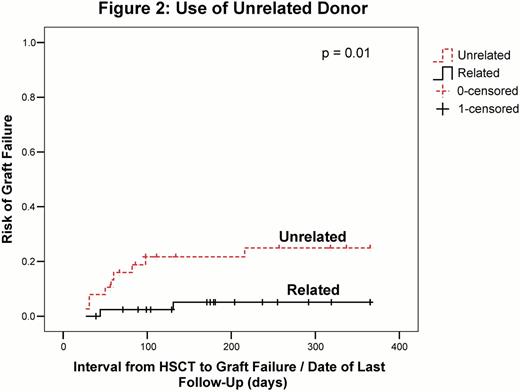
Allogeneic stem cell transplantation (allo HSCT) is the only modality that may produce long-term disease-free survival/cure for chronic lymphocytic leukemia (CLL). Successful transplant is hindered by relapse (REL), infections (INF), graft versus host disease (GVHD) and rejection of graft (GF). GF may manifest as either lack of initial donor (dn) cell engraftment (primary, P) or loss of donor cells after initial engraftment (secondary, S). To ascertain factors predictive for GF and outcomes thereafter including complete remission (CR), clearance of FISH abnormality (abn), non-relapse mortality (NRM), REL and survival, consecutive patients (pts) proceeding to allo HSCT at the Leukemia/BMT Program of BC with CLL (1991–2011) (n=81 total, 11 GF, 4P, 7S) were studied using prospective databases. HSCT Comorbidity index (Sorror) (CoI) was calculated for all pts, FISH performed pre and post SCT in 67 and 55 pts (10 GF), and chimerism for pts not receiving myeloablative (MA) conditioning (CON). P-values show relationship between non-GF and GF pts. Median (med) pt age (range) at diagnosis (dx) was 49 years (yrs) (26–65) whole cohort; younger at 47 (30–57) yrs in GF pts (p = 0.047). Gender was F in 24 (3 GF): M in 57 (8 GF) pts; 23 F (1 GF): 58 M (10 GF) dn (p = 0.3). Max stage was Rai advanced (III/IV) in 48 pts (59%) (8 GF) (p = 0.3); 17 (6 GF) had B-symptoms prior to HSCT (p = 0.005). Of 77 pts (95%) (11 GF) who received prior fludarabine (flu) (p = 0.4), 47 were refractory (REF) (7 GF) (p = 0.8); 35 (43%) (2 GF) were REF to last therapy (tx) pre-HSCT (p = 0.07). Med number of prior tx was 4 for both groups (range 1–14 whole cohort, 3–7 GF) (p = 0.5). CoI was 0 in 46 (57%) (6 GF), 1–2 in 26 (32%) (5 GF), and 3 or > in 9 pts (11%) (p = 0.3). Med pt age (range) at HSCT, whole cohort vs GF was similar at 57 (32–68) vs 58 (37–63) yrs (p = 0.4); and 45 (19–76) vs 42 (21–58) yrs for dn (p = 0.5). Dn was unrelated (UD) in 38 (47%) (9 GF) (p = 0.01), and HLA-mismatched (MM) in 17 (21%) (4 GF) (p = 0.2); 9 had HLA-C MM (2 GF) (p = 0.9). CON was MA (Cy/TBI) in 23 (28%) (2 GF) (p = 0.4), reduced intensity (RIC) in 41 (51%); flu/bu in 22 (27%), flu/bu + alemtuzumab (A) in 19 (23%) pts, (7 total RIC with GF, 6 post A CON) (p = 0.4), and non-myeloablative (NMA) (flu/cy) in 17 pts (21%) (2 GF) (p = 0.8). Peripheral blood (PB) was used for most pts (69, 85%) (10 GF) (p = 0.6). Cell dose, med (range) was 9.6 (0.4–25.8) TNC x108/kg pt wt (9.9, 2.7–18.4 for GF pts) (p = 0.4). CD34 count was 6.3 (2.4–578.9) x106/kg pt wt (5.9, 3.0–9.5 for GF pts) (p = 0.4). GVHD prophylaxis was CSP/MTX for the majority (79, 98%) (p = 0.1); 2 pts (1 GF) had T-Cell depletion. Pre-HSCT FISH abnormalities (abn) (61, 75% of pts) (10 GF) (p = 0.3) included: del 13q (37, 46%) (10 GF) (p = 0.09); +12 (11, 14%) (2 GF) (p = 0.9); del 11q (24, 30%) (6 GF) (p = 0.09) and del 17p (19, 23%) (3 GF) (p = 0.9). CR was achieved in 48 pts (2 GF) (p = 0.004), a med of 132.5d (28d to 3.5yrs) post HSCT (93d for GF pts, range -30–216 d) (p = 0.2). 42 pts with CR did not REL (2 GF), 6 did; 12 pts without CR have progressive CLL (4 GF), and 21 pts have no CR but no progression (5 GF) (p=0.02). 27 pts cleared FISH abn post HSCT a med of 98d (28d to 2.1yrs) (2 GF) (p = 0.09). AGVHD occurred in 45 pts (2 GF) (p = 0.09) and CGVHD in 55 pts (1 GF) (p = 0.001). KM estimate of OS (whole group vs GF) is similar at 66% vs 71% at 2yr, 57% vs 71% at 5yr and beyond (p = 0.8) At med post-HSCT follow-up (FU) of 3yrs (0.4–17yrs), 48 of 81 pts (60%) survive (7 GF, 64%). 33 are deceased at a med of 1.2yr (39d to 7.1yrs), 10 with NRM (1 GF) and 21 with REL (3 GF). Of the 11 GF pts, 7 required 2nd HSCT (64%, 3 with prior dn, all with different CON; 4 flu+treosulfan+ATG, 1 flu/cy, 1 Cy+ATG and 1 Cy+ATG+TBI); 2 pts (20%) 3rd HSCT. Current status is 7/11 GF pts alive (64%, 4 with CLL, 3 in CR) and 4 deceased (1 NRM, 2 INF, 1 CLL). Factors predictive for GF include (p-value, Odds-Ratio (if applicable)): younger age at dx (0.047), B-symptoms pre-HSCT (0.005, 6.3) (Fig 1), UD (0.01, 5) (Fig 2), alemtuzumab CON (0.008, 5.3) (Fig 3), clonal evolution (CE) by FISH (development of new FISH abn) (0.03, 5.8), and major ABO MM (0.04). GF pts had lower probability of CGVHD (0.001, 0.02), and post HSCT CR (0.004, 0.1), but similar OS to non-GF pts (p= 0.8 log rank). Strategies to decrease GF post allo HSCT for CLL include avoidance of major ABO MM and alemtuzumab in CON. Higher vigilance is required for GF in pts with pre-HSCT B symptoms, CE by FISH, and with use of UD. Of interest, survival for CLL pts with GF is not decreased due to effective rescue tx, but resource utilization is high with extra HSCT procedures required.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal