Abstract
Abstract 4136
Studies have shown that absolute lymphocyte count (ALC) early after allogeneic hematopoietic stem cell transplantation (HSCT) affects clinical outcomes. We hypothesize that the white blood cell (WBC) count at 1 month after HSCT may also predict transplant outcomes.
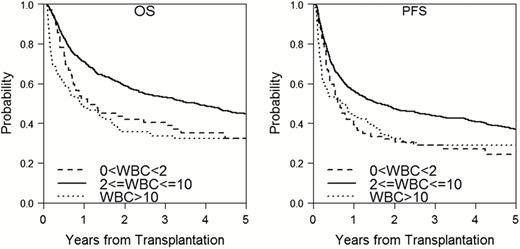
1115 adult patients undergoing allogeneic HSCT from 2003 through 2009 at Dana-Farber/Brigham and Women's Hospital were analyzed. The median age was 51 yrs (range 18–74); median follow up time among survivors was 4.3 years (range 1.1–9.2); 596 patients received reduced intensity conditioning (RIC) and 519 received myeloablative conditioning (MAC). Using the restricted cubic spline estimates on the log relative hazard over WBC at 1 month post HSCT, WBC was categorized as: low (0-<2), normal (2–10), and high (>10×109 cells/L).
The outcomes are summarized in the table and figure below. One-year OS was 52%, 71%, 48% for low, normal, high WBC at 1 month post HSCT, respectively, (p<0.0001) and 1-year PFS was 39%, 56%, and 44% for low, normal, high WBC, respectively (p<=0.0001). One year cumulative incidence of NRM was 15%, 5.2%, 9.1% for low, normal, high WBC (p=0.008 for low vs normal, p=0.33 for high vs normal) in RIC and 23%, 15%, 28% for low, normal, high WBC (p=0.28 for low vs normal, p=0.001 for high vs normal) in MAC. One year cumulative incidence of relapse was 51%, 44%, 58% for low, normal, high WBC (p=0.49 for low vs normal, p=0.04 for high vs normal) in RIC but 27%, 22%%, 23% for low, normal, high WBC (p=n.s.) in MAC. In multivariable multinomial logistic regression analysis, age (OR=0.94, p=0.004) and sirolimus containing GVHD prophylaxis (OR=3.3, p=0.044) in MAC, and mismatched donor type (OR=3.0, p=0.03) in RIC were the risk factors for low WBC; AML/CML (OR=8.2, p=0.009), CLL (OR=13.9, p=0.0036) in RIC and high disease-relapse index (ref. Armand et al, Blood, 2012) (OR=3.26, p=0.04) were risk factors for high WBC. In multivariable Cox model adjusting for other prognostic factors, both low and high WBC at 1 month were associated with poor OS (Low WBC: HR 1.59, p=0.01; High WBC: HR 1.85, p=0.007) and PFS (low WBC: HR 1.59, p=0.008; high WBC: HR 1.68, p=0.017) in RIC and high WBC at 1 month was associated with both poor OS (HR 1.93, p<0.0001) and PFS (HR 1.7, p=0.0006) in MAC. Furthermore, low or high WBC was associated with viral or fungal infection within 100 days of HSCT (viral: 27%, 9%, 9%,p=0.019 in MAC; 9%, 4%, 15%, p=0.01 in RIC; fungal: 27%, 6%, 9%,p=0.0006 in MAC; 2%, 2%, 9%, p=0.046 in RIC). In the MAC cohort, high WBC at 1 month was associated with development of subsequent grade II-IV acute GVHD: 41%, 39%, 51% for low, normal, (p<0.001). In the RIC cohort, only 48% in low (p<0.001) and 54% in high WBC (p=0.02) achieved ≥90% donor chimerism by day 30 post HSCT compared to 76% of patients in normal WBC, suggesting that the abnormal WBC reflects poor donor engraftment or persistence of underlying disease. There was a weak correlation between WBC and ALC at 1 month (correlation coefficient = 0.46). Low ALC is associated with poor outcome, but not high ALC.
Out data suggest that WBC at 1 month after allogeneic HSCT predicts transplant outcomes independent of ALC and chimerism.
| . | WBC . | N . | NRM (%) . | p-value . | Relapse (%) . | p-value . | PFS (%) . | p-value . | OS (%) . | p-value . |
|---|---|---|---|---|---|---|---|---|---|---|
| RIC | 0-<2 | 47 | 15 | 0.008 | 51 | 0.49 | 34 | 0.01 | 51 | 0.002 |
| 2-10 | 516 | 5.2 | ref | 44 | ref | 50 | ref | 72 | ref | |
| >10 | 33 | 9.1 | 0.33 | 58 | 0.04 | 33 | 0.002 | 48 | 0.0003 | |
| MAC | 0-<2 | 22 | 23 | 0.28 | 27 | 0.46 | 50 | 0.006 | 55 | 0.003 |
| 2-10 | 416 | 15 | ref | 22 | ref | 63 | ref | 70 | ref | |
| >10 | 81 | 28 | 0.001 | 23 | 0.65 | 48 | 0.0005 | 48 | <0.0001 | |
| Combined | 0-<2 | 69 | 17 | 0.03 | 43 | 0.12 | 39 | 0.0001 | 52 | <0.0001 |
| 2-10 | 932 | 9.4 | ref | 34 | ref | 56 | ref | 71 | ref | |
| >10 | 114 | 23 | <0.0001 | 33 | 0.94 | 44 | <0.0001 | 48 | <0.0001 |
| . | WBC . | N . | NRM (%) . | p-value . | Relapse (%) . | p-value . | PFS (%) . | p-value . | OS (%) . | p-value . |
|---|---|---|---|---|---|---|---|---|---|---|
| RIC | 0-<2 | 47 | 15 | 0.008 | 51 | 0.49 | 34 | 0.01 | 51 | 0.002 |
| 2-10 | 516 | 5.2 | ref | 44 | ref | 50 | ref | 72 | ref | |
| >10 | 33 | 9.1 | 0.33 | 58 | 0.04 | 33 | 0.002 | 48 | 0.0003 | |
| MAC | 0-<2 | 22 | 23 | 0.28 | 27 | 0.46 | 50 | 0.006 | 55 | 0.003 |
| 2-10 | 416 | 15 | ref | 22 | ref | 63 | ref | 70 | ref | |
| >10 | 81 | 28 | 0.001 | 23 | 0.65 | 48 | 0.0005 | 48 | <0.0001 | |
| Combined | 0-<2 | 69 | 17 | 0.03 | 43 | 0.12 | 39 | 0.0001 | 52 | <0.0001 |
| 2-10 | 932 | 9.4 | ref | 34 | ref | 56 | ref | 71 | ref | |
| >10 | 114 | 23 | <0.0001 | 33 | 0.94 | 44 | <0.0001 | 48 | <0.0001 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal