Abstract
Based on evidence from clinical trials there is a growing consensus that a three drug regimen involving at least one novel agent (proteasome inhibitor or immunomodulatory drug) should be used as initial induction in patients with newly diagnosed multiple myeloma (NDMM), usually for 3-4 cycles, prior to harvesting stem cells and proceeding to autologous stem cell transplantation (ASCT). Three drug regimens achieve deeper responses both before and after ASCT and this has been shown to translate into superior progression free survival (PFS). CR rates with the three drug regimens prior to ASCT are reported to be in the range of 20-30% with correspondingly high rates of very good partial response (VGPR) (50-60%). One such regimen is the combination of bortezomib with cyclophosphamide and dexamethasone (CyBorD). The published overall response rates (ORR) from phase II trials with CyBorD are approximately 90%, with at least 60% of patients achieving VGPR. At our center, CyBorD has been used as front line therapy since 2008. In this report we present our experience using this regimen as initial therapy in transplant eligible patients.
We retrospectively analysed clinical and laboratory records for 31 NDMM patients treated with CyBorD at our institution between 2008 and 2013, all of whom subsequently proceeded to ASCT. The standard protocol consisted of bortezomib 1.3 mg/m2 i.v. twice a week, cyclophosphamide orally at a dose of 300 mg/m2weekly, and dexamethasone orally of 40 mg daily given in 4 days long blocks weekly. Since November 2009 we have also used weekly CyBorD.
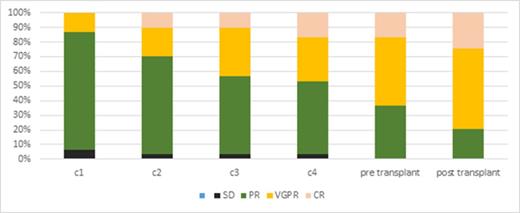
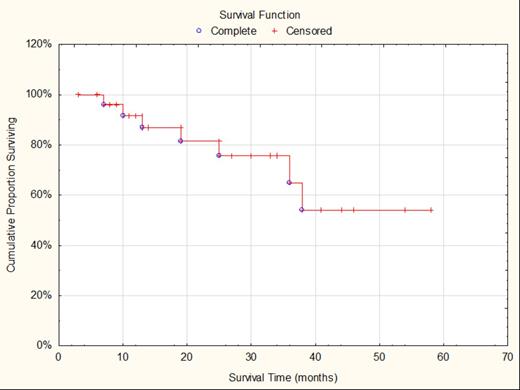
The median age was 57 years (range from 45 to 65), including 24 males and 7 females. According to ISS, 45% patients were classified as stage I, 5% stage II, and 50% as stage III. The ORR was 90% post cycle I and increased to 96% post cycle IV. At least VGPR was observed in 13% of patients after cycle 1 and 56% after cycle IV. Transplantation had improved the responses and 79% had at least VGPR post transplant versus 63% prior, and 24% patients achieved CR post ASCT in comparison to 16% prior ASCT (Fig. 1). The therapy was well tolerated. Haematological adverse events were acceptable and no patient required significant dose reduction or experienced treatment delay due to haematological toxicity. Importantly, no patients developed > grade 3 peripheral neuropathy and no patients required dose reduction or discontinuation of bortezomib due to neurological complications. Stem cell mobilisation was performed using a combination of cyclophosphamide 1.5g/m2 and G-CSF. All patients mobilized successfully without requirement for plerixafor. The medium CD34+ yield after 2 collection days was 8.2 x106/kg (range 1.8 -19.4). The PFS at 2 years was 75% and 64% at three years of follow up. At 2 years post transplant, the patients achieving at least a VGPR had a longer median PFS in comparison to patients with PR (91% vs 76%, p=NS) (Fig. 2). The cost analysis has shown that on average, the drug only cost of 4 cycles of CyBorD was 18 000€. This compares to 38 000€ for 4 cycles of bortezomib, lenalidomide, dexamethasone (VRD).
Our data confirm the safety and efficacy of the CyBorD protocol and its applicability to routine clinical practice outside of large academic myeloma centres. CyBorD is an active, well tolerated and cost effective option for patients with NDMM, which could be an ideal backbone for the incorporation of new modalities, such as monoclonal antibodies in induction therapy. A randomized comparison with other triple drug regimens are required to fully establish its place in the treatment of newly diagnosed multiple myeloma.
Response post each cycle of CyBorD, pre- and post ASCT.
Progression free survival for the entire cohort, 2 years PFS is 75% and 3 years PFS is 64%.
Progression free survival for the entire cohort, 2 years PFS is 75% and 3 years PFS is 64%.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal