Abstract
Although bone marrow (BM) and peripheral blood mobilized hematopoietic stem cells (PBSC) are widely used as graft sources in patients undergoing hematopoietic stem cell transplantation (HSCT), the graft of choice for each subset of patients remains to be determined. Several studies have, prospectively and retrospectively, addressed this question with inconsistent results. While the increased incidence of chronic graft versus host disease (cGVHD) in PBSC recipients has been unanimously found, data regarding disease free survival (DFS), overall survival (OS) and acute graft versus host disease (aGVHD) incidence have been controversial, mainly for patients with high risk disease. We retrospectively compared the clinical outcomes of 334 patients with acute leukemia and chronic myeloid malignancies receiving related BMT or PBSCT after myeloablative conditioning regimen, treated at seven transplantation centers in Brazil from 2008 to 2009.
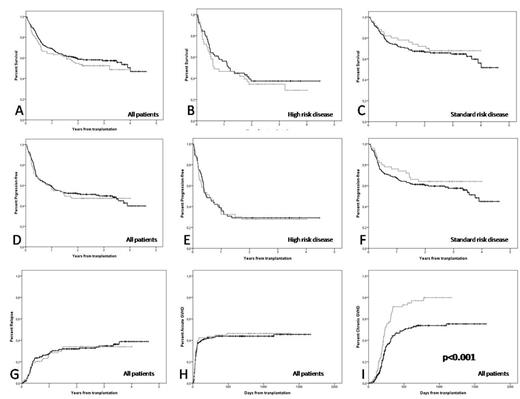
Median OS was 2.85 and 2.39 years (HR 1.19; 95% CI, 0.84 to 1.68, p=0.34), and DFS was 2.48 and 2.18 years for BM and PBSC recipients respectively (HR 1.07; 95% CI, 0.77 to 1.48, p=0.70). For patients with high risk disease, median OS was 2.1 and 1.72 years (HR 1.18; 95% CI, 0.73 to 1.91, p=0.50) and DFS was 0.46 and 0.58 years (HR 1.04; 95% CI, 0.66 to 1.64, p=0.86) for BMT and PBSCT respectively. Additionally, in agreement with previous reports, the cumulative incidence of chronic GVHD at three years was 53.7% and 79.8% (HR 1.93; 95% CI 1.38 to 2.69, p< 0.001) for BM and PBSC respectively (Figure 1). On the other hand, aGVHD incidence / severity, cumulative incidence of relapse and non relapse mortality (NRM) were not different between BM or PBSC recipients. The same being true when only patients with high risk disease were evaluated.
Major outcomes after transplant according to bone marrow (dark line) and peripheral blood (gray line) as the graft sources. Overall survival for the whole cohort (panel A), high risk (panel B), cumulative incidences of: and standard risk (panel C) patients; disease free survival for the whole cohort (panel D), high risk (panel E) and standard risk (panel F) patients, and relapse (panel G), grades III-IV aGVHD (panel H) and cGVHD (panel I) for the whole cohort. The only outcome that was statistically different was the cumulative incidence of cGVHD – (item I)
Major outcomes after transplant according to bone marrow (dark line) and peripheral blood (gray line) as the graft sources. Overall survival for the whole cohort (panel A), high risk (panel B), cumulative incidences of: and standard risk (panel C) patients; disease free survival for the whole cohort (panel D), high risk (panel E) and standard risk (panel F) patients, and relapse (panel G), grades III-IV aGVHD (panel H) and cGVHD (panel I) for the whole cohort. The only outcome that was statistically different was the cumulative incidence of cGVHD – (item I)
In conclusion, in our cohort, there was no OS or DFS benefit for patients receiving PBSC when compared to BM recipients, even when only high risk patients were analyzed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal