Key Points
CSF3R T618I is sufficient to drive a lethal myeloproliferative disease in a mouse bone marrow transplant model.
Treatment of CSF3R T618I mice with the JAK1/2 inhibitor ruxolitinib effectively reduces white blood cell count and spleen size.
Abstract
We have recently identified targetable mutations in CSF3R (GCSFR) in 60% of chronic neutrophilic leukemia (CNL) and atypical (BCR-ABL–negative) chronic myeloid leukemia (aCML) patients. Here we demonstrate that the most prevalent, activating mutation, CSF3R T618I, is sufficient to drive a lethal myeloproliferative disorder in a murine bone marrow transplantation model. Mice transplanted with CSF3R T618I–expressing hematopoietic cells developed a myeloproliferative disorder characterized by overproduction of granulocytes and granulocytic infiltration of the spleen and liver, which was uniformly fatal. Treatment with the JAK1/2 inhibitor ruxolitinib lowered the white blood count and reduced spleen weight. This demonstrates that activating mutations in CSF3R are sufficient to drive a myeloproliferative disorder resembling aCML and CNL that is sensitive to pharmacologic JAK inhibition. This murine model is an excellent tool for the further study of neutrophilic myeloproliferative neoplasms and implicates the clinical use of JAK inhibitors for this disease.
Introduction
We have recently identified activating mutations in the colony-stimulating factor 3 receptor (CSF3R; GCSFR) as targetable genetic drivers in ∼60% of chronic neutrophilic leukemia (CNL) and atypical (BCR-ABL–negative) chronic myeloid leukemia (aCML),1 2 related chronic leukemias characterized by increased numbers of mature neutrophils and the absence of BCR-ABL. Subsequently, the prevalence of CSF3R mutations in cases meeting strict diagnostic criteria for CNL was found to be as high as 83%, with a lower frequency observed in cases meeting strict aCML diagnostic criteria.2 CSF3R mutations are found in approximately 1% of de novo AML1,3 and can be acquired in patients with severe congenital neutropenia (SCN), which is correlated to an increased risk for development of AML.4
There are 2 classes of CSF3R mutations: truncations of the cytoplasmic domain and membrane proximal point mutations, including T618I.1,3 CSF3R truncation mutations are the mutation type nearly always observed in SCN and lead to enhanced cell surface expression and signaling of the receptor.5 In contrast, membrane proximal mutations (particularly T618I) are the predominant mutation type observed in CNL/aCML and confer ligand-independent growth.1,3 CSF3R mutations can activate downstream SRC- or JAK-family tyrosine kinase pathways, making these kinase pathways promising therapeutic targets for the treatment of leukemia patients with CSF3R mutations.1
Transgenic mice harboring CSF3R truncation mutations do not develop leukemia,6 but the truncation mutations can enhance leukemia progression in the context of another genetic driver.7 The T618I mutation has greater cell transformation capacity than the truncation mutations in vitro,1 but it is not known whether the T618I mutation alone is sufficient to drive CNL or aCML. In this study we created a CSF3RT618I bone marrow transplant mouse model that results in expansion of neutrophils in the peripheral blood and bone marrow, neutrophil infiltration in the spleen and liver, and eventual death, demonstrating that the T618I mutation alone is capable of driving neutrophil expansion. This neutrophilic expansion is dependent on JAK kinase signaling, because therapeutic JAK inhibition lowers white blood cell (WBC) count and reduces spleen size.
Methods
Expression vectors
Human CSF3R transcript variant 1 (NM_000760.2) pDONR vector was purchased from GeneCopoeia. CSF3RT618I mutation was made using the QuikChange II XL site-directed mutagenesis kit (Agilent Technologies). The Gateway Cloning System (Invitrogen) was used to clone CSF3RWT and CSF3RT618I into the MSCV-IRES-green fluorescent protein (GFP) plasmid.
Bone marrow transplantation
Wild-type BALB/C mice (000651) were purchased from Jackson Labs. Retroviral infection and transplantation was performed as previously described.8 All mouse work was performed with approval from the Oregon Health & Science University Institutional Animal Care and Use Committee.
Ruxolitinib treatment
Mice were administered 90 mg/kg ruxolitinib phosphate (ChemScene) dissolved in 5% dimethyl acetamide, 0.5% methylcellulose, or vehicle alone by oral gavage twice daily as previously described.9
Flow cytometry
After red blood cell lysis, cells were stained with the following antibodies for 20 minutes at 4°C: PE-CD3 clone 145-2C11 (eBioscience), PerCP Cy5.5-CD19 clone HIB1g (BD PharMingen), APC-CD11b clone M1/70 (eBioscience), and E450-Gr-1 clone RB6-8C5 (eBioscience). All flow cytometry was performed on an Aria III (BD Biosciences). Data were analyzed using FlowJo software (TreeStar).
Phospho-flow cytometry
Peripheral blood was collected from live animals immediately into fix/lyse buffer (BD Biosciences) for 15 minutes at 37°C. Cells were then permeabilized with methanol and stained with PE-pSTAT3 (pY705) (BD Biosciences) and analyzed by flow cytometry.
Pathology
Spleens, livers, and femurs were removed at necropsy and fixed in 10% zinc formalin. Fixed tissues were sectioned and stained using hematoxylin and eosin by the Histopathology Shared Resource at Oregon Health & Science University.
Results and discussion
CSF3RT618I causes a lethal myeloproliferative disorder resembling neutrophilic leukemia
To determine whether CSF3RT618I is sufficient to drive neoplastic expansion of neutrophils, we transplanted bone marrow expressing CSF3RT618I or CSF3RWT into irradiated mice. CSF3RWT was chosen for comparison to control for any effects of ectopic CSF3R expression. Blood counts were monitored 1 to 2 times per week (Figure 1A). The CSF3RT618I mice had an initial transient leukocytosis predominantly comprised of granulocytes (Figure 1A-C), trending back to normal by day 33 post transplant. The initial leukocytosis was specific to CSF3RT618I mice, indicating that it is a direct effect of the mutation rather than simply overexpression of CSF3R. At day 47, the CSF3RT618I mice had a dramatic rise in WBCs, again comprised of predominantly mature granulocytes (Figure 1A-C; supplemental Figure 1, available on the Blood Web site). By day 90, this leukocytosis was persistent and uniformly fatal in mice transplanted with hematopoietic cells expressing CSF3RT618I (Figure 1D). Expression of CSF3RWT did not lead to significant leukocytosis or morbidity in any mice. CSF3RT618I activated signaling downstream of the receptor, leading to an increase in phospho-STAT3 relative to mice expressing CSF3RWT (Figure 1E).
CSF3RT618Icauses a fatal disorder reminiscent of neutrophilic leukemia. Mice were transplanted with bone marrow expressing CSF3RWT (n = 5) or CSF3RT618I (n = 5). (A) CSF3RT618I causes leukocytosis. Total WBCs were measured over time in both the WT and T618I groups using an animal blood counter (scil Vet ABC). (B) Leukocytosis of CSF3RT618I is caused by granulocytic expansion. The percentage of granulocytes was measured using an animal blood counter and plotted over time. (C) CSF3RT618I results in an expansion of the granulocyte lineage at the expense of lymphocytes. Flow cytometry analysis was performed on peripheral blood from CSF3RWT and CSF3RT618I mice over time. The percentage of granulocytes relative to B-cell and T-cell lineages was increased in CSF3RT618I mice relative to CSF3RWT mice. Gating schemes used for analysis are shown in supplemental Figure 1. (D) CSF3RT618I mutation is uniformly lethal. For CSF3RT618I mice, events represent mouse death (n = 3) or euthanization as a result of moribund appearance (n = 2). The CSF3RWT mice were sacrificed at day 90 for histologic analysis; all mice appeared healthy. (E) CSF3RT618I mice have increased levels of phospho-STAT3. Blood from CSF3RWT or CSF3RT618I mice was pooled and pSTAT3 levels were measured by phospho-flow cytometry. Mean fluorescence intensity (MFI) of pSTAT3 was 604.5 for CSF3RWT and 1354.3 for CSF3RT618I.
CSF3RT618Icauses a fatal disorder reminiscent of neutrophilic leukemia. Mice were transplanted with bone marrow expressing CSF3RWT (n = 5) or CSF3RT618I (n = 5). (A) CSF3RT618I causes leukocytosis. Total WBCs were measured over time in both the WT and T618I groups using an animal blood counter (scil Vet ABC). (B) Leukocytosis of CSF3RT618I is caused by granulocytic expansion. The percentage of granulocytes was measured using an animal blood counter and plotted over time. (C) CSF3RT618I results in an expansion of the granulocyte lineage at the expense of lymphocytes. Flow cytometry analysis was performed on peripheral blood from CSF3RWT and CSF3RT618I mice over time. The percentage of granulocytes relative to B-cell and T-cell lineages was increased in CSF3RT618I mice relative to CSF3RWT mice. Gating schemes used for analysis are shown in supplemental Figure 1. (D) CSF3RT618I mutation is uniformly lethal. For CSF3RT618I mice, events represent mouse death (n = 3) or euthanization as a result of moribund appearance (n = 2). The CSF3RWT mice were sacrificed at day 90 for histologic analysis; all mice appeared healthy. (E) CSF3RT618I mice have increased levels of phospho-STAT3. Blood from CSF3RWT or CSF3RT618I mice was pooled and pSTAT3 levels were measured by phospho-flow cytometry. Mean fluorescence intensity (MFI) of pSTAT3 was 604.5 for CSF3RWT and 1354.3 for CSF3RT618I.
CSF3RT618I causes granulocytic expansion in the bone marrow and infiltration of granulocytes in the spleen and liver
Bone marrow of both CSF3RT618I and CSF3RWT mice exhibited abnormal hypercellularity; this was most pronounced in the CSF3RT618I mice (supplemental Figure 2). The marrow was composed mostly of mature granulocytes (supplemental Figure 2). CSF3RT618I and CSF3RWT mice also had infiltration of mature granulocytes into the spleen and liver (supplemental Figure 2), which was more pronounced in the CSF3RT618I than the CSF3RWT mice (supplemental Figure 2). The ability of CSF3RT618I as well as CSF3RWT to enhance production of mature myeloid cells is consistent with the normal physiological role of CSF3R in promoting neutrophil production and maturation.10,11 The T618I mutation in CSF3R further augments this signaling—possibly by conferring ligand independence to the receptor3 —resulting in a more exaggerated proliferation of granulocytes. The dramatic granulocytic expansion in mice transplanted with cells expressing CSF3RT618I led to death in all cases, whereas the granulocytic expansion in the CSF3RWT mice was not sufficient to cause death.
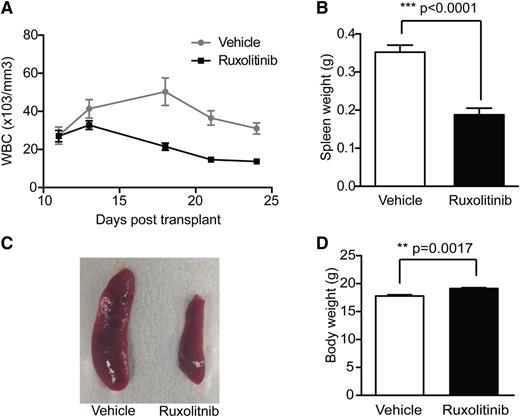
The JAK1/2 inhibitor ruxolitinib decreases WBC count and reduces splenomegaly in CSF3RT618I mice
We previously demonstrated that activating CSF3R mutations lead to preferential downstream signaling via JAK kinases, and a CNL patient carrying a JAK activating CSF3RT618I mutation showed marked clinical improvement after administration of the JAK1/2 inhibitor ruxolitinib.1 To determine whether the granulocytic expansion seen in CSF3RT618I mice is dependent upon the JAK kinase pathway, we tested the effect of ruxolitinib in a second cohort of CSF3RT618I mice. Oral administration of ruxolitinib (90 mg/kg 2×/d) or vehicle was started at day 12 post transplant, at which time mice already exhibited leukocytosis. Ruxolitinib treatment resulted in a prompt reduction in WBC count and a decrease in spleen weight (Figure 2A-C). Consistent with its ability to improve constitutional symptoms such as fatigue and early satiety in myelofibrosis,12,13 ruxolitinib-treated mice had increased body weight compared with vehicle-treated mice (Figure 2D). This demonstrates that the pathologic expansion of granulocytes in the CSF3RT618I mouse model is sensitive to JAK inhibition and warrants further investigation into the therapeutic use of JAK inhibitors in patients with CNL harboring the CSF3RT618I mutation.
The JAK1/2 inhibitor ruxolitinib decreases WBC count and reduces splenomegaly in CSF3RT618Imice. A second cohort of mice was transplanted with bone marrow expressing CSF3RT618I (n = 18); treatment with 90 mg/kg ruxolitinib twice per day (n = 9) or vehicle (n = 9) was initiated at day 12 post transplant. (A) Treatment with ruxolitinib results in prompt reduction in WBC count. Peripheral blood was collected on all mice 1 to 2 times per week. (B) Ruxolitinib decreases spleen weight. Mice were sacrificed on day 21 or 24 to evaluate spleen size. (C) Representative images of spleens from ruxolitinib- or vehicle-treated mice at time of necropsy. (D) Ruxolitinib-treated mice have significantly increased body weight compared with vehicle-control mice. Body weight was recorded on day 24 post transplant.
The JAK1/2 inhibitor ruxolitinib decreases WBC count and reduces splenomegaly in CSF3RT618Imice. A second cohort of mice was transplanted with bone marrow expressing CSF3RT618I (n = 18); treatment with 90 mg/kg ruxolitinib twice per day (n = 9) or vehicle (n = 9) was initiated at day 12 post transplant. (A) Treatment with ruxolitinib results in prompt reduction in WBC count. Peripheral blood was collected on all mice 1 to 2 times per week. (B) Ruxolitinib decreases spleen weight. Mice were sacrificed on day 21 or 24 to evaluate spleen size. (C) Representative images of spleens from ruxolitinib- or vehicle-treated mice at time of necropsy. (D) Ruxolitinib-treated mice have significantly increased body weight compared with vehicle-control mice. Body weight was recorded on day 24 post transplant.
Here we demonstrate that expression of CSF3RT618I in hematopoietic cells is sufficient to drive a lethal granulocytic expansion in mice. These data, in addition to the high prevalence of the CSF3RT618I mutation in patients with CNL,1,2 implicate CSF3RT618I as an important genetic driver of neutrophilic leukemias. Moreover, disease in the mouse model responds to therapeutic JAK inhibition, consistent with our previously observed disease response in a CNL patient treated with ruxolitinib.1 The CSF3RT618I bone marrow transplant provides a tractable mouse model of neutrophilic leukemia that will be useful for further studying the underlying biology of and therapeutic interventions in neutrophilic myeloproliferative neoplasms.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the histopathology shared resource at the Oregon Health & Science University for preparing the histology slides and performing hematoxylin and eosin staining.
This work was supported in part by The Leukemia & Lymphoma Society, the Training Program in Molecular Hematology (5T32HL007781), a Leukemia & Lymphoma Society Fellow Award, and a Medical Research Foundation Early Clinical Investigator Award (J.M.); and grants from the V Foundation for Cancer Research, the William Lawrence and Blanche Hughes Fund, the Gabrielle’s Angel Foundation for Cancer Research, and the National Cancer Institute, National Institutes of Health (5 R00CA151457-04) (J.W.T.).
Authorship
Contribution: A.G.F., S.B.L., L.R.R., A.A., M.M.L., M.L.A., J.D.M., and J.E.M. performed experiments and analyzed data; A.G.F., J.E.M., B.J.D., and J.W.T. designed experiments; and A.G.F., J.E.M., and J.W.T. wrote the manuscript.
Conflict-of-interest disclosure: J.W.T. and A.G.F. both receive funding for administration of clinical trials from Incyte, manufacturer of ruxolitinib. The other authors declare no competing financial interests
The current affiliation for A.G.F. is Division of Hematology/Oncology, University of California-Irvine, Irvine, CA.
Correspondence: Jeffrey W. Tyner, Oregon Health & Science University, BRB 511, Mailcode L592, 3181 SW Sam Jackson Park Rd, Portland, OR 97239; e-mail: tynerj@ohsu.edu.
References
Author notes
A.G.F. and J.E.M. contributed equally to this study.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal