Key Points
Osteoblastic niche supports quiescent multiple myeloma cells in vivo.
Multiple myeloma cells isolated from osteoblastic niche have enhanced tumorigenicity and stemlike properties.
Abstract
The heterogeneity of multiple myeloma (MM) contributes to variable responses to therapy. In this study, we aim to correlate the heterogeneity of MM to the presence of quiescent cells using the PKH26 dye. We tracked the rare quiescent cells in different niches of the bone marrow by allowing the cells to cycle in vivo. Surprisingly, quiescent PKH+ MM cells prefer to reside within the osteoblastic niches of the bone marrow (PKH+/OS) rather than the vascular (VS) niches or the spleen. These cells (PKH+/OS) displayed enhanced stemlike properties by forming colonies in semisolid medium. PKH+ cells were highly tumorigenic compared with PKH– cells and were resistant to a variety of drugs. However, the levels of drug resistance were somewhat similar regardless of where the PKH+ cells were isolated. Our data indicate that osteoblastic niches support the growth of quiescent PKH+ cells and allow them to have stemlike functions.
Introduction
In this report we used a lipophilic fluorescent marker, PKH, to understand the heterogeneity within multiple myeloma (MM) populations and to determine the effects of niches on the heterogeneity of MM cells.1 The intensity of PKH staining decreases with each cell division in a linear fashion, resulting in the labeling of quiescent cells within a proliferating population.2,3
We allowed the PKH-labeled MM cells to undergo the cell cycle within NOD/SCID mice,, and we tracked the PKH+ cells in different niches. In particular, we focused on analyzing the effects of different niches within the bone on MM cells because the bone marrow localization of MM cells is reminiscent of hematopoietic stem cells.4 Analysis of 70 NOD/SCID mice revealed that after in vivo cycling, quiescent PKH+ cells prefer to reside in the endosteal/osteoblastic regions (OS) of the bone marrow compared with the vascular (VS) regions or spleen. PKH+ cells from the osteoblastic niche (PKH+/OS) readily formed into colonies in PHA-LCM medium. The PKH+ MM cells were also highly proliferative in secondary xenograft assays and were resistant to select drugs compared with the PKH– MM cells. Our report is the first to show that quiescent MM cells have a preference for niches. Given that bone marrow provides a protective environment for MM cells to proliferate and survive during treatment, it is important to target these interactions to improve the efficacies of the current therapies and to eventually improve patient survival.
Methods
PKH staining
Cells (RPMI and NCI, 5 × 106) were stained with PKH67 (final concentration of 2 × 10−6 M) for 5 minutes. Stained cells were examined for PKH expression using fluorescence-activated cell sorting (FACS) analysis to ensure that >99% of cells were PKH+. Details on other methods can be found in the supplemental Methods, available on the Blood Web site. This study was conducted in accordance with the Declaration of Helsinki.
Results and discussion
Because the bone marrow localization of MM cells is reminiscent of the localization of hematopoietic stem cells, we compared the frequencies of PKH67+ cells in different niches that are important for MM proliferation, such as the OS regions of the bone and the VS regions of the bone. We also analyzed the spleen for PKH engraftment for comparison.
At 24, 48, and 72 hours post-transplant, the recipient mice were sacrificed to analyze the PKH+ cells. Similar to the hematopoietic stem cells reported previously,3 the highest amounts of PKH+ cells were recovered after 48 hours of in vivo cycling (supplemental Figure 1A). Therefore, we performed the following analyses at 48 hours post-transplantation.
Mice were sacrificed 48 hours post-transplantation with PKH67+ cells, and the number of PKH67+ cells in each niche was analyzed using FACS. After averaging a total of 70 mice, 11.56% of the PKH67+ RPMI MM cells were recovered from the OS niche, 7.65% from the VS niche, and 4.3% from the spleen. For the NCI MM cells, 18.3% of the cells were recovered from the OS niche, 8.9% were recovered from the VS niche, and 3.4% were recovered from the spleen (Figure 1A and supplemental Table 1). Quantitative real-time polymerase chain reaction analyses of the cells from the OS or the VS niches demonstrated that the mature bone marker osteocalcin and the bone morphogenetic proteins BMP2, BMP4, and BMP7 were more highly expressed in the cells from the OS niche than in the cells from the VS niche (supplemental Figure 1B), indicating a clear separation of the bone marrows from the bone lining tissues.
Quiescent PKH67+MM cells prefer to reside within the osteoblastic niche in the bones. (A) MM cells (106 cells/mouse) were stained with PKH67 and were injected into lightly irradiated (225 cGy) NOD/SCID mice via intravenous (IV) injection. Before injection, all cells were analyzed using FACS to ensure that >99% of the cells were PKH+. The mice were then sacrificed after 48 hours, and the spleens and bones were isolated. Cells were isolated from the osteoblastic (OS) and VS niches of the bones as indicated in the supplemental Methods. The number of PKH+ cells was calculated based on FACS analysis, which was gated on the PKH67+ cells (excitation wavelength 490 nm and emission wavelength 502 nm), and unstained samples were used as negative controls. (B) Immunohistochemistry analyses confirmed the FACS analyses. Each slide was examined for the presence of CD138, PKH, and Draq5. Image acquisition for the CD138, PKH, and Draq5 staining of each slide was performed using the same parameters of the confocal microscope in sequential mode. (C) PKH+CD138– MM cells exhibited slightly higher engraftment rates in bones compared with CD138+ cells. The CD138+ and CD138– cells were separated from MM cells (4 patients and 1 cell line) and were stained with PKH, followed by transplantation into irradiated NOD/SCID mice. (D) PKH+ MM cells isolated from the OS niches of the bones form more colonies in PHA-LCM medium than cells isolated from other niches. PKH+ MM cells were sorted from different organs of the mice 48 hours post-transplantation. PKH+ cells isolated from OS niches formed more colonies than PKH+ or PKH– cells from other niches. In addition, the colonies formed from the PKH+ cells from VS niches (PKH+/VS) were composed of fewer cells compared with PKH+/OS cells. In addition, the shape of the colonies was not as distinguishable from the colonies formed by the PKH+/OS cells. Although some PKH+ cells reside in the spleen (PKH+/SP) 48 hours post-transplantation, those cells failed to form colonies. All samples were plated in triplicate. *P < .01.
Quiescent PKH67+MM cells prefer to reside within the osteoblastic niche in the bones. (A) MM cells (106 cells/mouse) were stained with PKH67 and were injected into lightly irradiated (225 cGy) NOD/SCID mice via intravenous (IV) injection. Before injection, all cells were analyzed using FACS to ensure that >99% of the cells were PKH+. The mice were then sacrificed after 48 hours, and the spleens and bones were isolated. Cells were isolated from the osteoblastic (OS) and VS niches of the bones as indicated in the supplemental Methods. The number of PKH+ cells was calculated based on FACS analysis, which was gated on the PKH67+ cells (excitation wavelength 490 nm and emission wavelength 502 nm), and unstained samples were used as negative controls. (B) Immunohistochemistry analyses confirmed the FACS analyses. Each slide was examined for the presence of CD138, PKH, and Draq5. Image acquisition for the CD138, PKH, and Draq5 staining of each slide was performed using the same parameters of the confocal microscope in sequential mode. (C) PKH+CD138– MM cells exhibited slightly higher engraftment rates in bones compared with CD138+ cells. The CD138+ and CD138– cells were separated from MM cells (4 patients and 1 cell line) and were stained with PKH, followed by transplantation into irradiated NOD/SCID mice. (D) PKH+ MM cells isolated from the OS niches of the bones form more colonies in PHA-LCM medium than cells isolated from other niches. PKH+ MM cells were sorted from different organs of the mice 48 hours post-transplantation. PKH+ cells isolated from OS niches formed more colonies than PKH+ or PKH– cells from other niches. In addition, the colonies formed from the PKH+ cells from VS niches (PKH+/VS) were composed of fewer cells compared with PKH+/OS cells. In addition, the shape of the colonies was not as distinguishable from the colonies formed by the PKH+/OS cells. Although some PKH+ cells reside in the spleen (PKH+/SP) 48 hours post-transplantation, those cells failed to form colonies. All samples were plated in triplicate. *P < .01.
Immunohistochemistry analyses of xenograft organs confirmed the FACS data. Increased engraftment of PKH67+ (green) and CD138+ (red) cells were found in the OS niches compared with the VS and spleen niches (Figure 1B).
In addition, analyses of unmanipulated bones showed the location of the PKH+ cells near the OS regions of the bones. In contrast, the PKH– CD138+ cells were mainly located away from the bone-lining regions. It is also noted that fewer PKH– CD138+ cells were found in the same sections compared with PKH+ cells (supplemental Figure 2A-B).
Interestingly, the presence of PKH67+ cells that did not express the plasma cell surface marker CD138 were found after 48 hours of in vivo cycling (Figure 1B). These results indicate that most quiescent populations within MM can be either CD138+ or CD138–.
Therefore, we separated the MM cell lines or patient cells into CD138+ and CD138– cells and separately labeled those cells with PKH67 before transplantation into the mice. Although there was some variability, in general the CD138– cells derived from patients and cell lines retained the PKH staining better than CD138+ cells in vivo (Figure 1C), indicating that more CD138– MM cells remained quiescent in vivo compared with the CD138+ cells. The OS regions of the bones were still the preferable niche for both PKH+CD138+ and PKH+CD138– cells.
To increase OS niche specificity, we removed the monocyte lineages from the patient cells using CD14 antibodies. Slightly increased OS engraftment rates were observed upon transplantation of PKH+CD138– cells compared with the PKH+CD138+ cells. The OS niche was still a favorable niche for both cell populations (supplemental Table 2). We then compared the phenotypes of the CD138– MM cells with previously published MM stemlike cells using FACS analysis. The CD138– MM cells were enriched with CD20 and CD27 cell surface markers, as previously reported5 (supplemental Figure 2C-D). V(D)J recombination assays demonstrated the clonal relationship between the CD138+ and CD138– cells (supplemental Figure 2E).
We then measured the clonogenic properties of these cells using the PHA-LCM methylcellulose assay.5 Compared with the cells from other niches, the PKH+ cells isolated from the OS niche (PKH+/OS) formed the most colonies in PHA-LCM medium (Figure 1D and supplemental Table 3). Although some PKH67+ cells were found in the spleen (PKH+/SP), those cells failed to form colonies. The colonies derived from RPMI or NCI cells contained the same light-chain restriction patterns as the parental cell lines (supplemental Figure 3A). These data suggest that PKH+/OS cells are readily equipped to form colonies in vitro, which suggests that the niches that the cells reside in in vivo can influence the cells’ properties.
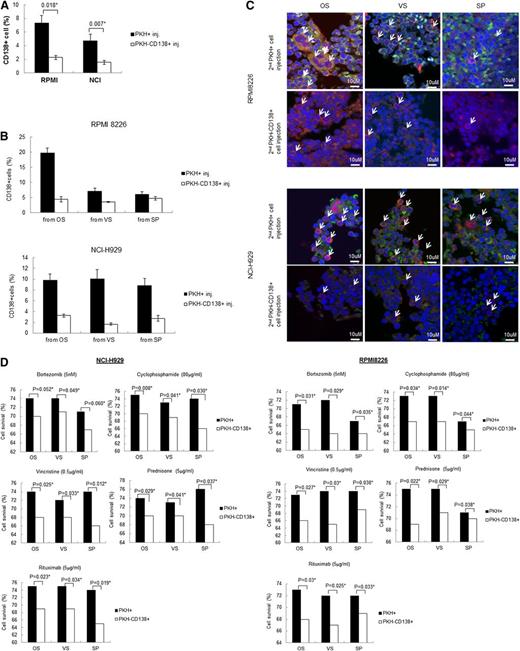
We then transplanted these cells in secondary recipient mice to observe the ability of the PKH+/OS cells to form tumors (supplemental Figure 3B). After 3 months, the organs were isolated from each mouse and were evaluated for tumor engraftment by FACS analyses using human CD138 as a marker. The PKH+CD138+ cells showed a significantly higher level of engraftment in the secondary mice than the PKH–CD138+ cells (Figure 2A). Interestingly, the PKH+ RPMI cells from the OS niches (20%) showed a higher CD138+ engraftment rate than the PKH+ cells from the VS niche (∼7%) or the spleen (∼5%) (Figure 2B). However, the PKH+/OS cells from the NCI cells engrafted to the OS, VS, and spleen at comparable levels, indicating that the homing ability of the NCI MM cells to locate to specific niches was somehow lost during serial transplantation. Immunohistochemistry results also supported the data from FACS analyses (Figure 2C). The increased clonogenic activity or tumorigenic properties of the PKH+ cells were not the result of differences in cell viability. Only live cells were sorted based on 7-AAD staining, before transplantation to the secondary xenografts (supplemental Figure 3C), and both the PKH+ and PKH– cells showed similar viability in vitro (supplemental Figure 3D).
PKH+cells from primary xenografts have a higher tumorigenic ability upon secondary transplantation. (A) PKH+ MM cells from primary mice xenografts showed higher engraftment rates in secondary recipient mice than cells isolated from other niches. PKH+ cells and PKH– (CD138+) cells were isolated from the spleen and the VS and OS niches of primary recipient mice 48 hours after transplantation. PKH– cells do not have markers to distinguish human cells from mouse cells; therefore, we isolated and sorted the PKH–CD138+ cells from the primary xenografts from the PKH– cells. These cells (5 × 104 cells/mouse) were then intravenously injected into irradiated secondary recipient mice and incubated for 3 months in vivo before sacrifice to evaluate engraftment. Tumor engraftment was analyzed using FACS against CD138 antibodies. (B) Detailed analysis of CD138+ engraftment levels analyzed in the OS niche, VS niche, and spleen. PKH+ or PKH–CD138+ cells from different niches of primary NOD/SCID mice were sorted and subsequently injected into secondary NOD/SCID mice. After 3 months, the secondary xenograft mice were sacrificed, and the spleens and bones were isolated. The cells from each niche were isolated and analyzed for CD138+ cell engraftment using FACS. Between 15 and 17 mice were analyzed for each niche, and the standard deviation was calculated accordingly. (C) Immunohistochemistry analyses confirmed the FACS data. Confocal microscopy was performed using different sections of paraffin-embedded organs. Each indicated organ was isolated from secondary xenograft NOD/SCID mice. PKH67+ cells are shown in green, CD138+ cells are shown in red, and the nucleus is shown in blue. This confocal staining is in accordance with the observations from the FACS analysis, mainly that the CD138+ engraftment was higher in secondary xenograft mice when cells from the osteoblastic or VS niches were injected. The spleens showed lower levels of CD138+ engraftment. (D) Cytotoxicity was assessed using the fluorometric cell viability assay CellTiter-Blue (Promega, Madison, WI). Sorted PKH+ and PKH–CD138+ cells (5 × 104) were incubated for the indicated times with the indicated drug doses for 24 hours. Cell viability was assessed based on the value of the fluorescent signal from the live cells with no drug treatments. The viabilities of the drug-treated cells were calculated based on a ratio of the fluorescent signal as shown in previous studies.7,8
PKH+cells from primary xenografts have a higher tumorigenic ability upon secondary transplantation. (A) PKH+ MM cells from primary mice xenografts showed higher engraftment rates in secondary recipient mice than cells isolated from other niches. PKH+ cells and PKH– (CD138+) cells were isolated from the spleen and the VS and OS niches of primary recipient mice 48 hours after transplantation. PKH– cells do not have markers to distinguish human cells from mouse cells; therefore, we isolated and sorted the PKH–CD138+ cells from the primary xenografts from the PKH– cells. These cells (5 × 104 cells/mouse) were then intravenously injected into irradiated secondary recipient mice and incubated for 3 months in vivo before sacrifice to evaluate engraftment. Tumor engraftment was analyzed using FACS against CD138 antibodies. (B) Detailed analysis of CD138+ engraftment levels analyzed in the OS niche, VS niche, and spleen. PKH+ or PKH–CD138+ cells from different niches of primary NOD/SCID mice were sorted and subsequently injected into secondary NOD/SCID mice. After 3 months, the secondary xenograft mice were sacrificed, and the spleens and bones were isolated. The cells from each niche were isolated and analyzed for CD138+ cell engraftment using FACS. Between 15 and 17 mice were analyzed for each niche, and the standard deviation was calculated accordingly. (C) Immunohistochemistry analyses confirmed the FACS data. Confocal microscopy was performed using different sections of paraffin-embedded organs. Each indicated organ was isolated from secondary xenograft NOD/SCID mice. PKH67+ cells are shown in green, CD138+ cells are shown in red, and the nucleus is shown in blue. This confocal staining is in accordance with the observations from the FACS analysis, mainly that the CD138+ engraftment was higher in secondary xenograft mice when cells from the osteoblastic or VS niches were injected. The spleens showed lower levels of CD138+ engraftment. (D) Cytotoxicity was assessed using the fluorometric cell viability assay CellTiter-Blue (Promega, Madison, WI). Sorted PKH+ and PKH–CD138+ cells (5 × 104) were incubated for the indicated times with the indicated drug doses for 24 hours. Cell viability was assessed based on the value of the fluorescent signal from the live cells with no drug treatments. The viabilities of the drug-treated cells were calculated based on a ratio of the fluorescent signal as shown in previous studies.7,8
Because cellular quiescence or stemlike properties are often linked to drug resistance in some tumors,6 we tested the drug susceptibility of the PKH+ or PKH–CD138+ cells in vitro using bortezomib, cyclophosphamide, vincristine, rituximab, and prednisone. Regardless of where the cells were isolated from, the PKH+ cells were more resistant to the drugs than the PKH– cell populations (Figure 2D). In summary, our report is the first show that quiescent MM cells preferably reside within OS niches. We discovered that both OS and VS niches in the marrow can support the proliferation of MM cells. However, the OS niches are the primary niches that support stemlike functions of MM cells. Our data also suggest that stemlike functions do not necessarily represent drug resistance, which is more likely governed by cell cycle status rather than the location of these cells, and these findings offer valuable preclinical models for drug testing and screenings for future applications.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The tissue samples were provided by the University of Texas MD Anderson Cancer Center Satellite Multiple Myeloma Tissue Bank. The authors thank Dr Naoki Nakayama (Center for Stem Cell and Regenerative Disease, IMM) for the useful discussion on bone-related markers.
This work was supported by The Anderson Cancer Center SPORE in multiple myeloma (P50CA142509).
Authorship
Contribution: Z.C. performed and analyzed the experiments; R.Z.O., M.W., and L.K. contributed the clinical samples; and N.M. supervised and planned overall experiments and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Nami McCarty, University of Texas-Health Science Center at Houston, 1835 Pressler St, IMM-630H, Houston, TX 77030; e-mail: nami.mccarty@uth.tmc.edu.