Key Points
Independent prognostic impact of biological markers, notably TP53 and SF3B1 mutations, in CLL patients requiring therapy.
NOTCH1 mutation as a predictive factor for reduced benefit from the addition of rituximab to FC chemotherapy.
Abstract
Mutations in TP53, NOTCH1, and SF3B1 were analyzed in the CLL8 study evaluating first-line therapy with fludarabine and cyclophosphamide (FC) or FC with rituximab (FCR) among patients with untreated chronic lymphocytic leukemia (CLL). TP53, NOTCH1, and SF3B1 were mutated in 11.5%, 10.0%, and 18.4% of patients, respectively. NOTCH1mut and SF3B1mut virtually showed mutual exclusivity (0.6% concurrence), but TP53mut was frequently found in NOTCH1mut (16.1%) and in SF3B1mut (14.0%) patients. There were few significant associations with clinical and laboratory characteristics, but genetic markers had a strong influence on response and survival. In multivariable analyses, an independent prognostic impact was found for FCR, thymidine kinase (TK) ≥10 U/L, unmutated IGHV, 11q deletion, 17p deletion, TP53mut, and SF3B1mut on progression-free survival; and for FCR, age ≥65 years, Eastern Cooperative Oncology Group performance status ≥1, β2-microglobulin ≥3.5 mg/L, TK ≥10 U/L, unmutated IGHV, 17p deletion, and TP53mut on overall survival. Notably, predictive marker analysis identified an interaction of NOTCH1 mutational status and treatment in that rituximab failed to improve response and survival in patients with NOTCH1mut. In conclusion, TP53 and SF3B1 mutations appear among the strongest prognostic markers in CLL patients receiving current-standard first-line therapy. NOTCH1mut was identified as a predictive marker for decreased benefit from the addition of rituximab to FC. This study is registered at www.clinicaltrials.gov as #NCT00281918.
Introduction
Chronic lymphocytic leukemia (CLL) is characterized by a very heterogeneous clinical course. Nowadays, most patients are diagnosed with early-stage, asymptomatic disease and may enjoy a normal life expectancy. However, when patients require therapy for disease progression, their outcome is highly variable with significant disease-related mortality.1-4
Importantly, characteristics such as clinical staging do not fully explain the variability in treatment response and survival. Among the biological disease features underlying this heterogeneity, genetic lesions and the mutational status of the immunoglobulin heavy chain variable genes (IGHV) are of significance. The IGHV mutation status defines 2 CLL subsets with different biological and clinical features.5-7 Unmutated IGHV is associated with high-risk characteristics and shorter survival times. Genomic aberrations as assessed by fluorescence in situ hybridization (FISH) are present in more than 80% of cases and a hierarchical model of their prognostic impact has been established that defines 5 subgroups: 17p deletion (17p−), 11q deletion (11q−), trisomy 12 (+12), normal, and 13q deletion (13q−) as the sole abnormality.8 The poor outcome of CLL with 17p− is due to inactivation of the tumor suppressor TP539,10 ; also the sole mutation of TP53 (TP53mut) has been associated with inferior survival.11-15
Novel gene mutations have been identified in CLL by next-generation sequencing techniques. Mutations of NOTCH1 and SF3B1 are among the most frequent and are detected in 5% to 20% of patients.16-19 NOTCH1mut leads to oncogenic pathway activation; the mutation has been found to occur more frequently with +12 and unmutated IGHV. SF3B1mut affects the splicing machinery as a novel pathogenic mechanism; it has been correlated with 11q− as well as unmutated IGHV. In initial studies performed in heterogeneous patient cohorts outside clinical trials, both mutations have been associated with advanced disease and poor prognosis.16-21
Although there is a wealth of clinical and laboratory parameters identifying subgroups with different outcome in CLL, only few markers such as stage and 17p− directly influence therapy and have entered clinical practice.1-4 Moreover, there is a lack of “predictive” markers22 (ie, parameters with different influences on outcome depending on the type of treatment). Whereas prognostic markers estimate outcome irrespective of therapy type, predictive markers help to assess outcome of a particular treatment compared with another one.
Methods
Patients and treatment
CLL8 was a prospective, international, multicenter, randomized (1:1) first-line treatment trial comparing fludarabine and cyclophosphamide (FC) or FC with rituximab (FCR)23 (www.clinicaltrials.gov #NCT00281918).24 Between July 2003 and March 2006, 817 patients in good physical condition were enrolled. Diagnosis, staging, and response evaluation were based on standard criteria used in general practice.25 The protocol was approved by our facilities’ institutional review boards and all patients provided informed consent before inclusion in the trial. This study was conducted in accordance with the Declaration of Helsinki.
Laboratory analyses
Genomic aberrations and IGHV status were analyzed centrally by FISH and Sanger sequencing, respectively.7,8 Central testing of ZAP70 was introduced late during the trial and was available for 289 patients only. Lymphocyte doubling time was not available. Minimal residual disease (MRD) levels were studied centrally by 4-color flow cytometry with a sensitivity of at least 10−4.26 TP53 exons 2-11 were analyzed by a resequencing chip (Amplichip; Roche Molecular Systems, Pleasanton, CA) and confirmatory Sanger sequencing (Big Dye Terminator Kit and ABI 3100 sequencer; Applied Biosystems, Darmstadt, Germany). NOTCH1 was studied for mutations by Sanger sequencing of 2 overlapping DNA fragments from the PEST domain (exon 34, chr9: 139, 390, 619-139, 390, 840, and 139, 390, 710-139, 391, 290, genome build hg19) in which >90% of the reported CLL mutations cluster.16-19 For SF3B1, exons 13-16 were analyzed by denaturing high-performance liquid chromatography on a WAVE 3500HT System (Transgenomic Inc., Glasgow, United Kingdom) followed by confirmatory Sanger sequencing. Only sequence variants that led to a change in amino acid composition and not reported as normal variants were scored as mutations. Only when confirmed by Sanger sequencing were mutations included in the analyses. If necessary, fragment collection after denaturing high-performance liquid chromatography and cloning of polymerase chain reaction products were performed to improve sensitivity of detection by Sanger sequencing. Wherever possible, the somatic status of mutations was confirmed from normal DNA. All experiments were done blinded from clinical data.
Statistical analyses
Statistical analyses were performed on an intent-to-treat basis including all patients with samples available. The primary end point was progression-free survival (PFS); secondary end points were response (clinical and MRD) and overall survival (OS). Time to event was analyzed by Kaplan-Meier estimates and log-rank testing. Groupwise comparisons were performed with the Fisher exact test (categorical variables).
Independent prognostic factors were identified by multivariable analyses using Cox's proportional hazards regression with backward selection including the following variables: treatment (FC/FCR), age (≥65/<65 years), sex, disease stage (C/A+B), B symptoms, Eastern Cooperative Oncology Group (ECOG) performance status (≥1/0), Cumulative Illness Rating Scale score (CIRS) (>1/≤1), white blood cell (WBC) count (≥50/<50 Giga/L), serum β2-microglobulin (β2-MG) level (≥3.5/<3.5 mg/L), serum thymidine kinase (TK) level (≥10/<10 U/L), genomic aberrations (11q−, +12, 13q−, 17p−, normal), IGHV status (98% cutoff), and the gene mutations (TP53mut, NOTCH1mut, SF3B1mut). All variables were available for 507 and 497 patients in the OS and PFS analyses, respectively. To identify a predictive impact of gene mutations for a specific treatment effect by the addition of rituximab, we performed multivariable analyses including the interaction with treatment (FC vs FCR). Significance was set as P < .05. Analysis was performed using SPSS 20.0 (SPSS, Chicago, IL).
The trial was initiated in 2003 as an investigator-initiated German CLL Study Group trial. Starting in 2004, F. Hoffmann-La Roche took over sponsorship aiming at approval of rituximab for CLL. The sponsor was subsequently responsible for protocol amendments, data gathering, and shared responsibility for medical review with the German CLL Study Group. The corresponding author was responsible for data analysis, interpretation, and writing of the manuscript and had full access to all data and took the final decision to submit for publication on behalf of all coauthors.
Results
Frequency and distribution of genetic lesions
Of the 817 patients enrolled in the trial, baseline samples were available for analysis of the individual genetic markers in 616 (75.4%) to 628 (76.9%) cases because central genetic testing was not scheduled for all countries. The status of at least 1 gene mutation could be determined in 635 (77.7%) patients, and this cohort was representative regarding baseline characteristics and response (supplemental Table 1, available on the Blood Web site).
TP53, NOTCH1, and SF3B1 were mutated in 72 of 628 (11.5%), 62 of 622 (10.0%), and 114 of 621 (18.4%) of patients, respectively (for mutation details, see supplemental Table 2). In brief, TP53mut was mostly missense (55 of 72, 76.7%) and located in the DNA-binding domain. NOTCH1mut was virtually confined (61 of 62, 98.4%) to a 2-bp deletion (c.7541_7542delCT) in exon 34 and led to premature truncation within the PEST domain. SF3B1mut was all missense, occurring most frequently as p.K700E/c.A2098G (48 of 114, 42.1%), with the remaining mutations scattered over exons 14-16.
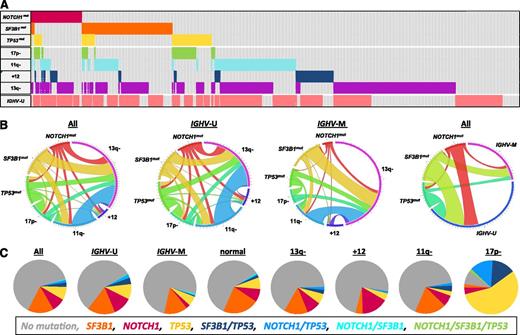
Frequencies and distributions of mutations, genomic aberrations, and IGHV status are illustrated in Figure 1. At least 1 mutation was identified in 218 of 621 (35.1%) patients; 190 (30.6%) patients had 1, 27 (4.3%) had 2, and 1 (0.2%) had 3 mutations. Of note, concurrent NOTCH1mut and SF3B1mut was very rare (0.6%), whereas TP53mut was frequently found in the NOTCH1mut (16.1%) and SF3B1mut (14.0%) subgroups.
Incidence and distribution of gene mutations, genomic aberrations, and IGHV status for the patients with all markers available (n = 573). Mutations in TP53, NOTCH1, and SF3B1 are denoted and color coded as NOTCH1mut, SF3B1mut, and TP53mut, respectively; genomic aberrations as 17p deletion (17p−), 11q deletion (11q−), trisomy 12 (+12), and 13q deletion (13q−); and IGHV unmutated as IGHV-U and IGHV mutated as IGHV-M. (A) Cluster diagram of patients (columns) and genetic parameters (rows). Distribution of marker positivity is ordered by rows. White boxes indicate patients without gene mutation, without aberrations (“normal FISH” group), or with mutated IGHV. (B) Circos diagrams of the pairwise cooccurrence of genomic aberrations with mutations for all patients (left), for IGHV subgroups (middle 2 panels), and of the pairwise cooccurrence of IGHV status with mutations (right). The length of the arc corresponds to the frequency of the marker alone plus its pairwise occurrence, whereas the width of the ribbon corresponds to the proportion of cooccurrence with the second marker. (C) Pie charts illustrating the occurrence and cooccurrence of mutations in all patients (left) and in subgroups defined by IGHV status and genomic aberrations (other panels). Mutations in TP53, NOTCH1, SF3B1, and combinations of mutations are indicated by the color code given at the bottom. The patterns of pairwise cooccurrence of gene mutations and genomic aberrations were similar in both IGHV subgroups, whereas the frequencies of mutations were different in subgroups defined by IGHV status and genomic aberrations (B-C).
Incidence and distribution of gene mutations, genomic aberrations, and IGHV status for the patients with all markers available (n = 573). Mutations in TP53, NOTCH1, and SF3B1 are denoted and color coded as NOTCH1mut, SF3B1mut, and TP53mut, respectively; genomic aberrations as 17p deletion (17p−), 11q deletion (11q−), trisomy 12 (+12), and 13q deletion (13q−); and IGHV unmutated as IGHV-U and IGHV mutated as IGHV-M. (A) Cluster diagram of patients (columns) and genetic parameters (rows). Distribution of marker positivity is ordered by rows. White boxes indicate patients without gene mutation, without aberrations (“normal FISH” group), or with mutated IGHV. (B) Circos diagrams of the pairwise cooccurrence of genomic aberrations with mutations for all patients (left), for IGHV subgroups (middle 2 panels), and of the pairwise cooccurrence of IGHV status with mutations (right). The length of the arc corresponds to the frequency of the marker alone plus its pairwise occurrence, whereas the width of the ribbon corresponds to the proportion of cooccurrence with the second marker. (C) Pie charts illustrating the occurrence and cooccurrence of mutations in all patients (left) and in subgroups defined by IGHV status and genomic aberrations (other panels). Mutations in TP53, NOTCH1, SF3B1, and combinations of mutations are indicated by the color code given at the bottom. The patterns of pairwise cooccurrence of gene mutations and genomic aberrations were similar in both IGHV subgroups, whereas the frequencies of mutations were different in subgroups defined by IGHV status and genomic aberrations (B-C).
IGHV unmutated CLL showed a higher frequency of the 3 mutations (42.9% vs 24.1%, P < .001), of TP53mut (15.0% vs 6.2%, P < .001), and NOTCH1mut (13.6% vs 4.5%, P < .001), whereas there was no significant increase for SF3B1mut (20.4% vs 15.8%, P = .194). The subgroups defined by genomic aberrations showed differences in mutation frequencies, but a few were significant: the 17p− subgroup frequently had TP53mut (84.3% vs 5.1%, P < .001) and NOTCH1mut (20.0% vs 9.1%, P = .024), whereas CLL with +12 rarely had SF3B1mut (4.2% vs 20.9%, P < .001) (supplemental Table 3).
Patient characteristics
Overall, the gene mutations showed few relations with the baseline disease characteristics (supplemental Table 3). TP53mut were associated with a CIRS >1. NOTCH1mut was correlated with Binet stages A/B and absence of B symptoms, and there was a trend (P = .066) toward lower WBC counts. There was no significant correlation between NOTCH1mut and CD20 expression (supplemental Figure 1), whereas there was higher expression of CD20 in cases with +12 (supplemental Figure 2A). SF3B1mut showed a significant correlation with TK ≥10 U/L, and in trend (P = .058) were more frequent in male patients.
Overall, the incidence of Richter syndrome during the course of the study was low, as expected in a first-line treatment cohort. Among the 622 patients with data on NOTCH1 available, there were 35 (5.6%) cases of Richter syndrome overall, 31 among 560 (5.5%) with NOTCH1WT, and 4 among 62 (6.5%) with NOTCH1mut (P = .770).
Clinical and MRD response to therapy
Clinical response rates were evaluated by mutation and by treatment (Table 1). The TP53mut subgroup showed significantly lower response rates with both treatments, the NOTCH1mut group showed a trend (not significant) toward lower response mostly with FCR, and SF3B1mut did not impact response to either treatment. Conversely, FCR compared with FC significantly improved response in all subgroups defined by absence of mutations and in tendency also in subgroups with mutations with the least relative improvement in the NOTCH1mut group (Table 1).
Outcome in patient subgroups defined by mutations (columns) and treatment (rows)
| . | TP53wt (n = 556) . | TP53mut (n = 72) . | P value* . | NOTCH1wt (n = 560) . | NOTCH1mut (n = 62) . | P value* . | SF3B1wt (n = 507) . | SF3B1mut (n = 114) . | P value* . |
|---|---|---|---|---|---|---|---|---|---|
| Clinical response (% CR + PR) | |||||||||
| FC | 92.2 | 51.6 | <.001 | 88.1 | 87.1 | .775 | 87.7 | 89.1 | 1.000 |
| FCR | 98.2 | 75.0 | <.001 | 96.6 | 90.0 | .109 | 96.3 | 96.4 | 1.000 |
| P value† | .002 | .105 | <.001 | 1.000 | <.001 | .287 | |||
| MRD negativity (% <10−4) | |||||||||
| FC | 37.3 | 7.7 | .034 | 32.5 | 50.0 | .338 | 37.5 | 23.5 | .151 |
| FCR | 68.0 | 18.2 | .002 | 66.1 | 46.2 | .222 | 64.1 | 66.7 | .832 |
| P value† | <.001 | .576 | <.001 | 1.000 | <.001 | <.001 | |||
| PFS (median in mo) | |||||||||
| FC | 35.9 | 12.1 | <.001 | 32.8 | 33.9 | .743 | 33.9 | 28.6 | .008 |
| FCR | 59.0 | 15.4 | <.001 | 57.3 | 34.2 | .013 | 59.1 | 42.9 | .033 |
| P value† | <.001 | .001 | <.001 | .996 | <.001 | .004 | |||
| OS (median in mo) | |||||||||
| FC | 89.6 | 30.4 | <.001 | 83.7 | 85.9 | .597 | 86.4 | 75.6 | .172 |
| FCR | NR | 42.2 | <.001 | NR | 79.2 | .112 | NR | NR | .301 |
| P value† | .014 | .166 | <.001 | .793 | .004 | .100 |
| . | TP53wt (n = 556) . | TP53mut (n = 72) . | P value* . | NOTCH1wt (n = 560) . | NOTCH1mut (n = 62) . | P value* . | SF3B1wt (n = 507) . | SF3B1mut (n = 114) . | P value* . |
|---|---|---|---|---|---|---|---|---|---|
| Clinical response (% CR + PR) | |||||||||
| FC | 92.2 | 51.6 | <.001 | 88.1 | 87.1 | .775 | 87.7 | 89.1 | 1.000 |
| FCR | 98.2 | 75.0 | <.001 | 96.6 | 90.0 | .109 | 96.3 | 96.4 | 1.000 |
| P value† | .002 | .105 | <.001 | 1.000 | <.001 | .287 | |||
| MRD negativity (% <10−4) | |||||||||
| FC | 37.3 | 7.7 | .034 | 32.5 | 50.0 | .338 | 37.5 | 23.5 | .151 |
| FCR | 68.0 | 18.2 | .002 | 66.1 | 46.2 | .222 | 64.1 | 66.7 | .832 |
| P value† | <.001 | .576 | <.001 | 1.000 | <.001 | <.001 | |||
| PFS (median in mo) | |||||||||
| FC | 35.9 | 12.1 | <.001 | 32.8 | 33.9 | .743 | 33.9 | 28.6 | .008 |
| FCR | 59.0 | 15.4 | <.001 | 57.3 | 34.2 | .013 | 59.1 | 42.9 | .033 |
| P value† | <.001 | .001 | <.001 | .996 | <.001 | .004 | |||
| OS (median in mo) | |||||||||
| FC | 89.6 | 30.4 | <.001 | 83.7 | 85.9 | .597 | 86.4 | 75.6 | .172 |
| FCR | NR | 42.2 | <.001 | NR | 79.2 | .112 | NR | NR | .301 |
| P value† | .014 | .166 | <.001 | .793 | .004 | .100 |
CR, complete response; mut, mutated; NR, not reached; PR, partial response; wt, wild-type.
P value columns compare outcome between subgroups defined by mutation status within 1 treatment arm.
P value rows compare outcome between treatment arms within subgroups defined by mutation status.
Disease burden as measured by MRD levels at final response assessment paralleled clinical response patterns (Table 1). MRD negativity (<10−4) was significantly less frequent in the TP53mut groups with both treatments, whereas it was estimated (not significant) to be less frequent in NOTCH1mut with FCR only, and was not significantly impacted by SF3B1mut with either treatment. Of note, FCR compared with FC approximately doubled the rate of MRD negativity in all subgroups except the NOTCH1mut group, in which no improvement was seen at all (FCR: 46.2% vs FC: 50.0%, P = 1.000) (Table 1). Although there was no statistically significant difference when comparing MRD levels between the groups defined by NOTCH1 status within 1 treatment arm, there was a highly significant difference when comparing the 2 treatments within the group with NOTCH1WT but not within the group with NOTCH1mut.
Survival analyses
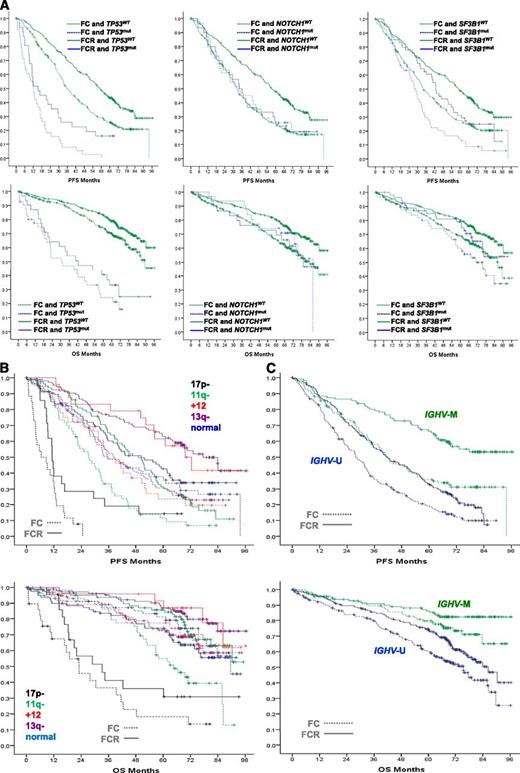
After a median follow-up time of 70 (range 0-97) months, there were 550 (67.3%) and 279 (34.1%) events in the full study population for PFS and OS, respectively. FCR significantly improved PFS (hazard ratio [HR] 0.586, P < .001) and OS (HR 0.678, P = .001). PFS and OS for the subgroups defined by gene mutations, IGHV status, and genomic aberrations according to treatment are illustrated in Figure 2.
Kaplan-Meier estimates. PFS (top) and OS (bottom) according to the status of gene mutations (A), genomic aberrations according to the hierarchical model (B), and IGHV status (C). Assignment to genetic subgroup and treatment is denoted by the color code and the structure of lines, respectively.
Kaplan-Meier estimates. PFS (top) and OS (bottom) according to the status of gene mutations (A), genomic aberrations according to the hierarchical model (B), and IGHV status (C). Assignment to genetic subgroup and treatment is denoted by the color code and the structure of lines, respectively.
TP53mut was associated in both treatment arms with significantly decreased PFS (FC: HR 4.295, P < .001; FCR: HR 3.173, P < .001) and OS (FC: HR 4.642, P < .001; FCR: HR 4.447, P < .001). In contrast, NOTCH1mut was only in the FCR arm associated with significantly decreased PFS (FC: HR 0.931, P = .741; FCR: HR 1.718, P = .013) and with a tendency toward inferior OS (FC: HR 0.854, P = .605; FCR: HR 1.610, P = .112). There were not significant differences regarding PFS and OS when comparing the groups defined by presence or absence of NOTCH1mut among patients with +12 or when comparing the groups defined by presence or absence of +12 among patients with NOTCH1mut (supplemental Figure 2B-C). SF3B1mut was associated in both treatment arms with significantly decreased PFS (FC: HR 1.520, P = .009; FCR: HR 1.463, P = .033) and with slightly (not significant) inferior OS (FC: HR 1.338, P = .178; FCR: HR 1.305, P = .301) (Table 1; Figure 2A).
17p− defined the worst prognostic subgroup in both treatment arms and there were only a few 17p− patients (7 of 46) with PFS of longer than 24 months (Figure 2B). When comparing baseline characteristics among these 46 patients, the only factor significantly associated with PFS >24 months was WBC (6 of 19 patients with WBC <50/nL vs 1 of 27 patients with ≥50/nl, P = .015). There was no significant association between PFS >24 months and IGHV status (1 of 8 patients with mutated IGHV vs 6 of 38 patients with unmutated IGHV, P = 1.000). However, 17p− CLL patients with PFS >24 months had better responses (CR 1 of 1, partial response 5 of 23, and stable disease/progressive disease 1 of 18, P = .030). A landmark analysis of patients with 17p− CLL without PFS event within 12 months of treatment start confirmed the prognostic impact of 17p− in this subgroup (supplemental Figure 3).
To study the independent prognostic impact of gene mutations, we performed multivariable analyses including the commonly used clinical and biological disease markers. The characteristics of the subgroup with all parameters available for multivariable PFS analysis (497/635, 78.3% of patients with gene mutation data) is given in supplemental Table 1. There were PFS events in 351 of 497 (70.6%) and OS events in 174 of 507 (34.3%) patients. The following independent prognostic factors were identified for PFS: FCR, TK ≥10 U/L, unmutated IGHV, 11q−, 17p−, TP53mut, and SF3B1mut. Regarding OS, the following parameters were found: FCR, age ≥65 years, ECOG ≥1, β2-MG ≥3.5 mg/L, TK ≥10 U/L, unmutated IGHV, 17p−, and TP53mut (Table 2).
Multivariable analyses of prognostic factors for survival
| Parameter . | HR . | 95% CI . | P value . |
|---|---|---|---|
| PFS | |||
| FCR | 0.506 | 0.408-0.628 | <.001 |
| TK ≥10 U/L | 1.362 | 1.049-1.769 | .020 |
| IGHV-U | 1.719 | 1.326-2.228 | <.001 |
| 11q− | 1.546 | 1.215-1.968 | <.001 |
| 17p− | 2.916 | 1.779-4.781 | <.001 |
| TP53mut | 2.123 | 1.400-3.218 | <.001 |
| SF3B1mut | 1.346 | 1.037-1.747 | .026 |
| OS | |||
| FCR | 0.650 | 0.480-0.880 | .005 |
| Age ≥65 y | 1.423 | 1.039-1.950 | .028 |
| ECOG ≥1 | 1.622 | 1.190-2.209 | .002 |
| β2-MG ≥3.5 mg/L | 1.473 | 1.069-2.030 | .018 |
| TK ≥10 U/L | 1.864 | 1.195-2.909 | .006 |
| IGHV-U | 2.059 | 1.389-3.053 | <.001 |
| 17p− | 2.715 | 1.602-4.602 | <.001 |
| TP53mut | 3.014 | 1.889-4.808 | <.001 |
| Parameter . | HR . | 95% CI . | P value . |
|---|---|---|---|
| PFS | |||
| FCR | 0.506 | 0.408-0.628 | <.001 |
| TK ≥10 U/L | 1.362 | 1.049-1.769 | .020 |
| IGHV-U | 1.719 | 1.326-2.228 | <.001 |
| 11q− | 1.546 | 1.215-1.968 | <.001 |
| 17p− | 2.916 | 1.779-4.781 | <.001 |
| TP53mut | 2.123 | 1.400-3.218 | <.001 |
| SF3B1mut | 1.346 | 1.037-1.747 | .026 |
| OS | |||
| FCR | 0.650 | 0.480-0.880 | .005 |
| Age ≥65 y | 1.423 | 1.039-1.950 | .028 |
| ECOG ≥1 | 1.622 | 1.190-2.209 | .002 |
| β2-MG ≥3.5 mg/L | 1.473 | 1.069-2.030 | .018 |
| TK ≥10 U/L | 1.864 | 1.195-2.909 | .006 |
| IGHV-U | 2.059 | 1.389-3.053 | <.001 |
| 17p− | 2.715 | 1.602-4.602 | <.001 |
| TP53mut | 3.014 | 1.889-4.808 | <.001 |
Variables included in the models: FC, FCR, age, sex, stage, ECOG performance status, CIRS score, B symptoms, white blood cell count, TK, β2-MG, 11q−, +12, 13q−, 17p−, IGHV mutational status, TP53mut, NOTCH1mut, SF3B1mut.
CI, confidence interval; U, unmutated.
Predictive marker analyses
To identify a predictive impact of gene mutations for a specific treatment effect by the addition of rituximab, we performed multivariable analyses including treatments (FC, FCR), gene mutations (TP53mut, NOTCH1mut, SF3B1mut), and their interactions as potential variables. Regarding PFS, we identified FCR, TP53mut, SF3B1mut, and notably NOTCH1mut interaction with FCR as independent factors (Table 3). When including all clinical and biological baseline characteristics in the multivariable model, no significant treatment interaction was found. The interaction between NOTCH1mut and treatment is illustrated uniformly in the analyses of clinical response, MRD, PFS, and OS, with improvement by the addition of rituximab to FC demonstrated mostly among patients without NOTCH1mut (Table 1; Figure 2A). There were no significant differences when comparing the distributions of baseline characteristics of patients with NOTCH1mut between the 2 treatment arms, arguing against an imbalance of risk factors as a cause of the differential treatment effects.
Multivariable analyses of mutations, treatments, and their interactions for survival after FC and FCR treatment
| Parameter . | HR . | 95% CI . | P value . |
|---|---|---|---|
| PFS | |||
| FCR | 0.544 | 0.445-0.665 | <.001 |
| TP53mut | 3.607 | 2.737-4.755 | <.001 |
| SF3B1mut | 1.355 | 1.070-1.717 | .012 |
| NOTCH1mut interaction | 1.652 | 1.076-2.535 | .022 |
| OS | |||
| FCR | 0.654 | 0.498-0.860 | .002 |
| TP53mut | 4.470 | 3.234-6.177 | <.001 |
| Parameter . | HR . | 95% CI . | P value . |
|---|---|---|---|
| PFS | |||
| FCR | 0.544 | 0.445-0.665 | <.001 |
| TP53mut | 3.607 | 2.737-4.755 | <.001 |
| SF3B1mut | 1.355 | 1.070-1.717 | .012 |
| NOTCH1mut interaction | 1.652 | 1.076-2.535 | .022 |
| OS | |||
| FCR | 0.654 | 0.498-0.860 | .002 |
| TP53mut | 4.470 | 3.234-6.177 | <.001 |
Variables included in the models: FC, FCR, TP53mut, NOTCH1mut, SF3B1mut, and the interactions of each gene mutation with treatments.
Because approximately 5% of all patients carried more than 1 gene mutation, and because of the independent impact of individual mutations with a strong impact of TP53mut, we analyzed PFS and OS for the following groups, in which each patient was assigned to 1 category only: (1) TP53mut (irrespective of other mutations), (2) SF3B1mut without TP53mut, (3) NOTCH1mut without TP53mut and SF3B1mut, and (4) no mutation (supplemental Figure 4). This analysis was in line with the differential prognostic and predictive roles of gene mutations as described previously (Figure 2A) with prognostic impact of TP53mut as well as SF3B1mut and predictive impact of NOTCH1mut.
Discussion
We evaluated the frequency, distribution, and clinical impact of TP53mut, NOTCH1mut, and SF3B1mut in a large cohort of CLL patients homogeneously defined by their need of first treatment based on international consensus criteria used in general practice. A major advantage of our study was that the analyses could be done on patients treated within a prospective, randomized trial of current standard therapy,23,24,27,28 and that a wide range of clinical and biological disease characteristics was available.
Overall, the frequency and distribution of mutations were similar as in previous analyses; however, a direct comparison is difficult because most reported cohorts were diverse with respect to disease state.16-21 For example, a population-based study of newly diagnosed patients showed low frequencies of NOTCH1mut and SF3B1mut (4.7% and 3.6%, respectively),29 whereas analysis in the UK Leukaemia Research Fund (LRF) CLL4 treatment trial showed frequencies of NOTCH1mut and SF3B1mut (10.0%, and 16.7%, respectively) in line with our data.30
The mutations were unevenly distributed in CLL subsets. Particularly striking was the mutual exclusivity of NOTCH1mut and SF3B1mut, indicating different pathogenic mechanisms and possibly distinct classes of driver mutations in CLL. Conversely, the incidence of TP53mut was even increased in the NOTCH1mut and SF3B1mut subgroups, suggesting cooperating effects. In relation to the IGHV status, we observed a higher mutational load in IGHV-unmutated CLL, most pronounced for TP53mut and NOTCH1mut, but much less so for SF3B1mut. Regarding genomic aberrations, we found the expected cooccurrences of 17p− with TP53mut10-15 and +12 with NOTCH1mut,16-21 although the latter was much less pronounced than in some but not all previous studies,29 whereas +12 was rare in SF3B1mut as also recently reported.30 Of note was the increased rate of 17p− in NOTCH1mut, again pointing to nonexclusivity of NOTCH1 and p53 abnormalities.
Despite comprehensive characterization, only a few associations were found with clinical and laboratory baseline disease features (supplemental Table 3). In contrast to previous studies,16,17,21 we found no association for NOTCH1mut with advanced disease, as we observed lower stages, fewer B symptoms, and lower WBC counts, and there was no significant association with the development of Richter syndrome.
The dissection of the differential impact of individual clinical and biological markers on outcome after state-of-the-art therapy could be performed in the current study because of its size, depth of annotation, and mature follow-up time. The strongest impact on all outcome end points was found for 17p− and TP53mut, confirming results from previous trials with chemotherapy alone.14,15,30 Of note, 17p− and TP53mut were confirmed as independent adverse markers despite their low incidence and high cooccurrence, underlining the role of p53 in determining treatment outcome. The prognostic impact of 17p− and TP53mut was observed for all efficacy end points (clinical response, MRD, PFS, OS) and was similarly evident in both treatment groups (FC and FCR). A landmark analysis at 12 months confirmed the prognostic impact of 17p−, and mutated IGHV status did not identify 17p− CLL patients with prolonged PFS. 17p− and TP53mut therefore define CLL patients who should be referred to specialized centers for enrollment in clinical trials developing novel treatment approaches in this genetically defined ultra-high-risk group.
In contrast, SF3B1mut was not associated with clinical or MRD response, but was a significant independent factor for more rapid disease progression, pointing to its role as an important driver mutation in CLL. NOTCH1mut was not selected as an independent unfavorable factor, underlining its reduced prognostic role, as also recently suggested by data from the UK LRF CLL4 trial using chemotherapy.30
Based on a recently proposed model,31 gene mutations and genomic aberrations were combined into the following groups: (1) 17p− and/or TP53mut (irrespective of other aberrations and mutations); (2) 11q−, SF3B1mut, and/or NOTCH1mut but no 17p− or TP53mut; (3) +12 or normal FISH but no 17p−, 11q−, TP53mut, SF3B1mut, or NOTCH1mut, and (4) 13q− as sole aberration and no gene mutation (supplemental Figure 5). As expected, this combined categorization of patients led to a wider separation of the survival estimates, although this type of grouping is not supported by the results of our multivariable analysis.
When evaluating the individual impact of clinical and laboratory parameters on PFS, it is noteworthy that only biological markers were of independent value. Conversely, FCR remained an independent favorable marker for PFS and OS, even after accounting for the relevant biological disease markers. Taken together, our multivariable analyses indicate that a combination of clinical (advanced age, reduced performance status) and biological features (17p−, 11q−, unmutated IGHV, TP53mut, SF3B1mut, high TK, high β2-MG) can be used to identify specific patient subgroups where further improvement beyond rituximab addition to chemotherapy is needed. Notably, these results apply to a specific treatment situation and may not be generalized. Correspondingly, in the UK LRF CLL4 trial comparing chlorambucil vs fludarabine vs FC, both NOTCH1mut and SF3B1mut had an impact on PFS and OS,30 underlining that the influence of gene mutations can vary according to the type and intensity of the regimen administered. Furthermore, prognostic marker analyses will need reassessment in the context of novel treatments because their impact may be changed by these options.
To identify a “predictive” impact of the gene mutations on therapy in a strict sense (ie, a differential influence on outcome depending on the type of treatment), we formally tested treatment interaction by multivariable analyses. Interestingly, a relation was found between the NOTCH1 mutational status and the addition of rituximab. Patients with NOTCH1mut in the current study did not appear to benefit from rituximab because there was neither an increase in clinical or MRD response nor an improvement in PFS or OS. That virtually a single mutation (c.7541_7542delCT) was relevant for this impact could make NOTCH1 analysis a straightforward and potentially highly worthwhile test that, if confirmed, could prevent side effects and the cost of rituximab. However, the lack of benefit from rituximab in NOTCH1mut CLL is a provocative finding that needs confirmation in independent trials before it may impact routine patient management.
The biological mechanisms underlying the differential activity of rituximab in relation to NOTCH1 mutational status remain unclear and need additional investigation because reduced rituximab target (CD20) expression did not appear to be a cause. Elucidation of the mechanistic basis would strengthen the rationale for guiding treatment based on NOTCH1mut status. Furthermore, it will be interesting to see if a similar observation can be made with other anti-CD20 or different antibodies.
Taken together, this study by integrated biological and clinical disease characterization provides a basis for evaluation of improved prognostic models (outcome estimation) and the identification of predictive markers (guidance of treatment choice). Testing for TP53mut should be evaluated in future clinical trials and performed before treatment initiation, particularly in patients without 17p−, to further evaluate its impact despite low frequency. Our data suggest NOTCH1mut as a predictive factor for reduced benefit from rituximab addition to chemotherapy, a provocative finding that needs confirmation by independent studies before entering routine diagnostics and possibly influencing patient management. SF3B1mut is a biological marker that provides independent prognostic information on progression but less so on survival and should be assessed prospectively in additional clinical trials. Finally, the impact of prognostic and predictive markers may change when better treatments become available. Therefore, it will be important to reassess these results derived from a trial with today’s most efficacious standard treatment approach in light of future concepts with novel agents targeting biological disease mechanisms.
The online version of this article contains a data supplement.
There is an Inside Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank all patients and their physicians for trial participation and donation of samples; Doris Winter, Christina Galler, and Elisa Woinikanis for their excellent technical assistance; and Myriam Mendila, Nancy Valente, Stephan Zurfluh, and Jamie Wingate for their support in conception and conduct of the trial.
This work was supported by grants from the CLL Global Research Foundation (Alliance), Else Kröner-Fresenius-Stiftung (2010_Kolleg24, Project 2012_A146), Virtual Helmholtz Institute (VH-VI-404, TP2), Deutsche Forschungsgemeinschaft (Sonderforschungsbereich 1074 project B2 and Heisenberg-Stipendium BU 1339/3-1) (L.B.), Deutsche José Carreras Leukämie Stiftung (Deutsche Jose Carreras Leukämie Stiftung R 06/03v) (S.B.), and F. Hoffmann-La Roche.
Authorship
Contribution: S.S. designed and performed research, provided patients and samples, gave administrative support, analyzed data, and wrote the paper; A.S., P.P., and T.Z. designed and performed research, analyzed data, and approved the paper; and all other authors performed research, analyzed data, and approved the paper.
Conflict-of-interest disclosure: S.S., M.K., U.J., C.M.W., and M.H. received research support and honoraria from Roche; N.P. and L.W. are employed by Roche Molecular Systems; and M.K.W. and G.F.-R. are employed by F. Hoffmann-La Roche. The remaining authors declare no competing financial interests.
Correspondence: Stephan Stilgenbauer, Department of Internal Medicine III, Ulm University, Albert-Einstein-Allee 23, 89081 Ulm, Germany; e-mail: stephan.stilgenbauer@uniklinik-ulm.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal