Key Points
Loss of SPARC protects HSCs from the toxic effects of serial 5-FU treatment.
HSCs in a SPARC-deficient niche return faster to quiescence after activation following 5-FU treatment.
Abstract
Around birth, hematopoietic stem cells (HSCs) expanding in the fetal liver migrate to the developing bone marrow (BM) to mature and expand. To identify the molecular processes associated with HSCs located in the 2 different microenvironments, we compared the expression profiles of HSCs present in the liver and BM of perinatal mice. This revealed the higher expression of a cluster of extracellular matrix-related genes in BM HSCs, with secreted protein acidic and rich in cysteine (SPARC) being one of the most significant ones. This extracellular matrix protein has been described to be involved in tissue development, repair, and remodeling, as well as metastasis formation. Here we demonstrate that SPARC-deficient mice display higher resistance to serial treatment with the chemotherapeutic agent 5-fluorouracil (5-FU). Using straight and reverse chimeras, we further show that this protective effect is not due to a role of SPARC in HSCs, but rather is due to its function in the BM niche. Although the kinetics of recovery of the hematopoietic system is normal, HSCs in a SPARC-deficient niche show an accelerated return to quiescence, protecting them from the lethal effects of serial 5-FU treatment. This may become clinically relevant, as SPARC inhibition and its protective effect on HSCs could be used to optimize chemotherapy schemes.
Introduction
Hematopoietic stem cells (HSCs) are required to maintain the hematopoietic system, as many of its mature cell types must continuously be replaced. These long-lived stem cells are able to self-renew lifelong while preserving their multilineage differentiation potential. During homeostasis, the self-renewal rate of HSCs is low, with their vast majority being quiescent and residing in the G0 phase of the cell cycle.1 Using label-retaining assays, our group and others have described a population within the HSC compartment, which is long-term quiescent and referred to as dormant.2,3 On injury to the hematopoietic system, as, for example, induced by the chemotherapeutic agent 5-fluorouracil (5-FU), quiescent and dormant HSCs become reversibly activated and undergo proliferation to eventually replenish the hematopoietic system.2,4-7 Several stimuli have recently been identified that induce activation of dormant HSCs including cytokines such as interferon-α and -γ and granulocyte colony-stimulating factor.2,5,8 Despite this recent progress in understanding the molecular basis of HSC activation, very little is known about how their return to quiescence is regulated.
The extracellular matrix protein secreted protein acidic and rich in cysteine (SPARC; osteonectin; BM-40) is known to be involved in tissue development, repair, and remodeling.9,10 SPARC regulates cell-matrix interactions and modulates signaling pathways. In the adult organism at homeostasis, SPARC expression is restricted to remodeling tissues such as the bone and gut. Moreover, SPARC expression is frequent in tumors and fibrotic disorders.10 SPARC has attracted attention in the hematopoietic research field, as it is part of the commonly deleted region of the 5q myelodysplastic syndrome and is deregulated in other hematologic malignancies.11-15 However, previous studies have only demonstrated a role for SPARC in erythroid development. For instance, a reduction of burst-forming units of the erythroid lineage (BFU-E) was detected in SPARC-deficient bone marrow (BM), although erythrocyte and erythroid progenitor numbers were normal in vivo.11-15 There is experimental evidence that SPARC promotes the development of erythroid progenitors in a non-cell autonomous fashion, as the BFU-E defect could be rescued by exogenous SPARC.12
The role of SPARC in HSC biology remains poorly understood, although a recent study suggests that SPARC is dispensable for murine HSC function.13 SPARC is part of the BM niche and a critical regulator of bone remodeling.16 As SPARC is expressed in remodeling tissues and during tissue repair, some phenotypes of mutant mice may only become obvious in situations of injury.17 Strikingly, here we show that SPARC deficiency affects HSC function under certain stress conditions, which provides SPARC-deficient mice with a survival benefit when treated repeatedly with the chemotherapeutic agent 5-FU. In addition, we demonstrate that this is mediated by its function in the niche rather than by a cell autonomous role in HSCs.
Material and methods
Animal experiments and mouse models
Animal experiments were conducted in accordance with the German law (license G-191/11 from Regierungspräsidium Karlsruhe). All adult mice used in experiments were 7 to 10 weeks of age at the start of the experiment unless otherwise stated. Conditional Sparctm1a(EUCOMM)Wtsi mice were purchased (The Knockout Mouse Project, Davis, CA) and crossed with FLP-deleter to excise the Neo-cassette18 and MxCre19 or Tie2Cre20 to obtain conditional MxCre;Sparcflox2 or Tie2Cre;Sparcflox2 mice or with Sox2Cre21 to obtain homozygous germ-line–deleted mice of te C57BL/6 background referred to as Sparc−/−. Deletion of SPARC was confirmed by polymerase chain reaction (PCR) and quantitative reverse transcriptase-PCR (qRT-PCR). Primers used for genotyping are listed in supplemental Table 1, available on the Blood Web site. Wild-type (WT) control mice were C57BL/6JOlaHsd mice (Harlan, Boxmeer, Netherlands), unless otherwise stated. Control mice were always age and gender matched. For the MxCre-mediated gene deletion, 3-week-old mice were injected with 10 μg/g polyI:C (Invivogen, San Diego, CA) in phosphate-buffered saline 5 times every other day. For polyI:C treatment, mice were injected with 100 μg/mouse polyI:C (Invivogen) at indicated times prior to analysis. In serial 5-FU experiments, mice were injected intraperitoneally every 7, 10, or 11 days with 150 μg/g 5-FU (Invivogen). Previously irradiated and transplanted mice received 120 μg/g. To analyze cell proliferation by 5-bromo-2-deoxyuridine (BrdU) incorporation, 200 μL BrdU (1.8 mg/mL in phosphate-buffered saline; Becton Dickinson, San Jose, CA) were injected intraperitoneally 15 hours before analysis. The transforming growth factor (TGF)-β blocking antibody 2G7 (kindly provided by Genentech, San Francisco, CA) or isotype control immunoglobin (Ig)G1 was injected intravenously at a dose of 10 μg/g. All experiments were performed 2 (N = 6-8) or 3 times (N = 9-16).
BM transplantations
Recipient mice were lethally irradiated with 2 × 5 Gy 1 day prior to BM transplantation. In straight chimera experiments, recipients were CD45.1 (B6.SJL-PtprcaPepcb/BoyCrl), whereas in reverse chimera experiments, recipient mice were either Sparc−/− or C57BL/6JOlaHsd (both CD45.2). A total of 1 to 3 × 106 BM cells in phosphate-buffered saline was injected intravenously. Donor mice were either CD45.2 (experimental and littermate control mice) or CD45.1/2 (competitor and reverse chimeras; intercross between B6.SJL-PtprcaPepcb/BoyCrl and C57BL/6JOlaHsd). BM of 3 donor mice per genotype was pooled.
BM preparation and flow cytometry
Bones were crushed in RPMI + 2% fetal calf serum and filtered through a 40-μm mesh, and numbers of viable cells were determined by Vi-CELL (Beckman Coulter, Brea, CA). Lin− BM was prepared by negative isolation with monoclonal antibodies against CD4, CD8a, B220, Gr1, Ter119, and CD11b and removal with sheep anti-rat IgG-coated Dynabeads (Life Technologies, Carlsbad, CA). BM niche cells were isolated by collagenase digestion of cleaned bone chips as previously described.22 Populations and corresponding antigens are listed in supplemental Table 2 and antibody clones in supplemental Table 3. For cell cycle analysis, cells were fixed with Cytofix/Cytoperm and stained with anti-Ki-67 antibody (B56; Becton Dickinson) and Hoechst33342 (Life Technologies). Samples were analyzed on the flow cytometer LSRII/Fortessa (Becton Dickinson). Cell sorting was performed on fluorescence-activated cell sorter (FACS) AriaII/AriaIII (Becton Dickinson). Data were analyzed with FlowJo software (Tree Star, Ashland, OR).
RNA isolation and qRT-PCR
A total of 2000 to 50 000 cells were sorted in extraction buffer, and RNA was isolated with the PicoPure RNA isolation kit (Arcturus, Mountain View, CA), including RNase-free DNase digestion (Qiagen, Hilden, Germany). RNA samples were transcribed using the SuperScript VILO cDNA synthesis kit according to the manufacturer’s instructions using additional oligo-dT primers (Invitrogen). qRT-PCR was performed using the ABI Power SYBR Green Master Mix (Life Technologies) on a Viia7 (Life Technologies) with the primers listed in supplemental Table 4.
Blood counts
Blood counts were determined using a Hemavet 950FS (Drew Scientific, Dallas, TX).
Histology
Freshly isolated bones and guts were fixed overnight in 10% buffered formaldehyde at 4°C, dehydrated, embedded in paraffin, cut with a microtome, rehydrated, and stained with hematoxilin and eosin.
Statistical analyses
Statistical methods are mentioned in figure legends.
Results
SPARC is highly upregulated by HSCs that have recently colonized the BM
Definitive HSCs develop in the embryo in the aorta-gonad-mesonephros region by embryonic day (E)8.5.23,24 These HSCs then migrate to the fetal liver and placenta at approximately E11.5, where they undergo expansion and maturation.25 Close to the time of birth, HSCs leave the liver and colonize the BM, where they engraft in the proximity of the endosteal interface of trabecular bone and are maintained throughout life.26 Here, using gene expression profiling, we identified the extracellular matrix protein SPARC to be highly upregulated in HSCs that have recently colonized the BM, along with a cluster of extracellular matrix-related genes (supplemental Figure 1).
SPARC expression by HSCs is dispensable for HSC homing and engraftment
This observation prompted us to analyze HSC numbers in several SPARC-deficient mouse models at different ontogenetic stages. Moreover, we performed competitive transplantation experiments to compare the frequency of functional HSCs in the different knockout strains and their controls. Together, our results suggest that cell autonomous SPARC is dispensable for HSC function (supplemental Figures 2 and 3).
SPARC-deficient mice show reduced sensitivity to serial 5-FU treatment
Several cell types have been suggested to support HSC function in the BM niche, including osteoblasts, osteoprogenitors, mesenchymal stem cells, endothelial cells, and perivascular cells.27,28 Considering the extracellular nature of SPARC, SPARC secreted by niche cells rather than HSCs themselves might affect HSC function. Interestingly, niche cells of adult mice including osteo-lineage cells, mesenchymal progenitors, and endothelial cells express >1000-fold higher SPARC mRNA levels than adult HSCs (Figure 1A). These results and the reported role of SPARC in tissue remodeling and repair9,10 prompted us to investigate a possible involvement of SPARC in response to hematopoietic stress. Therefore, Sparc−/− and littermate control mice were treated with the chemotherapeutic agent 5-FU at 10-day intervals. 5-FU targets cycling cells, leading to myelo-suppression, which in turn activates resistant dormant HSCs to replenish the injured hematopoietic system.7 Hence, repeated 5-FU treatment results in HSC exhaustion and death of the animals due to BM failure. Strikingly, Sparc−/− mice had a reduced sensitivity to serial 5-FU treatment and survived significantly longer (Figure 1B; median survival: WT = 43 days, Sparc−/− = 71 days). Intriguingly, ∼40% of the SPARC-deficient mice acquired resistance to 5-FU and survived up to 180 days, which is when the experiments were terminated (Figure 1B-C). Comparable results were obtained with another SPARC-deficient mouse model (supplemental Figure 4G).29
SPARC-deficient mice are less sensitive to serial 5-FU injections due to the absence of SPARC expression by niche cells. (A) SPARC mRNA expression by cell type of the adult BM niche including mature osteoblasts (mOBs), osteoprogenitors (iOBs), and the fraction containing mesenchymal stem cells (MSCs) and endothelial cells (ECs) (N = 10 per group; mean and SD). (B) SPARC-deficient mice show enhanced survival when injected with 5-FU at a dose of 150 μg/g at 10-day intervals (N = 10-11 per group; median survival: WT = 43 days, Sparc−/− = 71 days; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (C) Straight chimeras that lack SPARC expression by hematopoietic cells have no survival benefit in the serial 5-FU experiment. C57Bl/6J mice were transplanted with WT (littermate control) or Sparc−/− BM, and 5-FU treatment (120 μg/g at 10-day intervals) was started 12 weeks after transplantation (N = 9; median survival: WT = 23 days, Sparc−/− = 20 days; no significant difference). (D) Lack of SPARC expression by non-hematopoietic cells is sufficient to provide a survival benefit in the serial 5-FU experiment. WT or Sparc−/− mice were transplanted with WT BM (CD45.1/2), and 5-FU treatment (120 μg/g at 10-day intervals) was started 12 weeks after transplantation. (N = 13-17; median survival: WT = 42 days, Sparc−/− = 169; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test).
SPARC-deficient mice are less sensitive to serial 5-FU injections due to the absence of SPARC expression by niche cells. (A) SPARC mRNA expression by cell type of the adult BM niche including mature osteoblasts (mOBs), osteoprogenitors (iOBs), and the fraction containing mesenchymal stem cells (MSCs) and endothelial cells (ECs) (N = 10 per group; mean and SD). (B) SPARC-deficient mice show enhanced survival when injected with 5-FU at a dose of 150 μg/g at 10-day intervals (N = 10-11 per group; median survival: WT = 43 days, Sparc−/− = 71 days; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (C) Straight chimeras that lack SPARC expression by hematopoietic cells have no survival benefit in the serial 5-FU experiment. C57Bl/6J mice were transplanted with WT (littermate control) or Sparc−/− BM, and 5-FU treatment (120 μg/g at 10-day intervals) was started 12 weeks after transplantation (N = 9; median survival: WT = 23 days, Sparc−/− = 20 days; no significant difference). (D) Lack of SPARC expression by non-hematopoietic cells is sufficient to provide a survival benefit in the serial 5-FU experiment. WT or Sparc−/− mice were transplanted with WT BM (CD45.1/2), and 5-FU treatment (120 μg/g at 10-day intervals) was started 12 weeks after transplantation. (N = 13-17; median survival: WT = 42 days, Sparc−/− = 169; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test).
We next sought to determine whether the observed phenotype was caused by a cell autonomous effect of SPARC deficiency in HSCs or by a lack of SPARC expression by niche cells. Therefore, we first transplanted lethally irradiated C57BL/6J mice with BM of Sparc−/− or littermate control mice. We checked their blood chimerism after 8 weeks and excluded mice with a donor chimerism <95%. To allow the transplanted cells to establish homeostasis, we waited for 12 weeks before starting 5-FU treatment at 10-day intervals. The survival curves of the groups transplanted with Sparc−/− or littermate control BM showed no significant difference, suggesting that lack of hematopoietic cell-derived SPARC is not sufficient to provide a survival advantage to mice treated with repeated cycles of 5-FU (Figure 1C). Conversely, to address the contribution of niche cell-derived SPARC to the survival advantage observed in SPARC-deficient mice, we performed a reverse chimera experiment. Lethally irradiated Sparc−/− and C57BL/6J control mice were transplanted with WT BM (C57BL/6J; CD45.1/2 hybrid). We again analyzed their blood chimerism after 8 weeks to exclude mice with a donor chimerism <95%. Serial 5-FU treatment at 10-day intervals was started 12 weeks after transplantation. Interestingly, Sparc−/− reverse chimeras showed an increased median survival of 169 days compared with 42 days and an incomplete penetrance of the lethality phenotype, recapitulating our observation in straight SPARC knockout mice (Figure 1D). Together, these results suggest that niche-derived SPARC deficiency is the main mediator of the increased HSC resistance observed in SPARC-deficient mice in response to repeated 5-FU treatment.
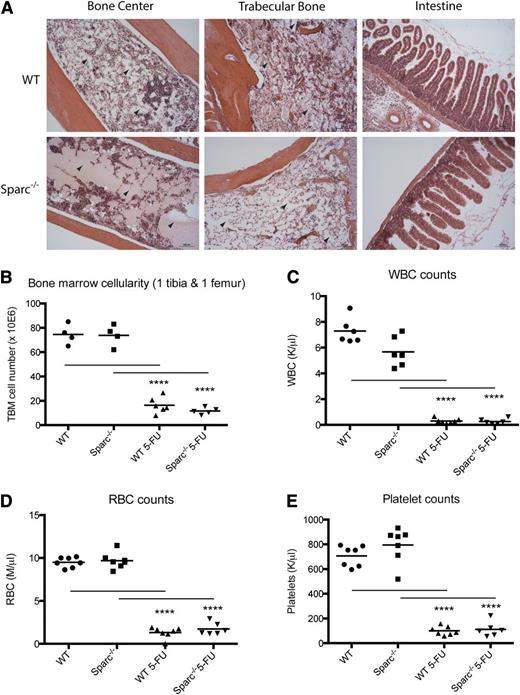
WT and SPARC-deficient mice die of hematopoietic failure in response to serial 5-FU treatment
Because 5-FU treatment not only affects hematopoietic cells, but also affects cells of the highly regenerative small intestine,30,31 we examined whether the phenotype observed in the absence of SPARC is due to its role in the hematopoietic system. To this end, we analyzed hematoxylin and eosin-stained tissue sections of bones and intestines of 5-FU–treated WT and Sparc−/− mice at the time of death. Irrespective of the genotype, all mice analyzed demonstrated an aplastic anemia in central and trabecular regions of the bone (Figure 2A). This is confirmed by the severely reduced BM cell numbers of these mice (Figure 2B). In contrast, the structure of their intestines remained largely unaffected (Figure 2A). Moreover, we analyzed peripheral blood counts of mice dying in response to serial 5-FU injections. Significantly reduced red blood cell (RBC), white blood cell (WBC), and platelet counts of all WT and Sparc−/− mice show that they suffered from severe pancytopenia before they had to be killed (Figure 2C-D). Together, our results demonstrate that both WT and SPARC knockout mice die of hematopoietic failure in the serial 5-FU experiments, therefore suggesting that SPARC deficiency has a beneficial effect on the hematopoietic system in this context.
WT and SPARC-deficient mice die of hematopoietic failure in response to serial 5-FU treatment. (A) Hematoxylin and eosin stainings of bone and gut sections of WT and Sparc−/− mice dying from serial 5-FU treatment (age at start of treatment, 8 weeks; age at examination, 14 and 16 weeks for WT and Sparc−/− mice, respectively). Trabecular and central bone regions are aplastic, suggesting WT and Sparc−/− mice die of hematopoietic failure. Examples for aplastic BM regions are indicated with arrowheads. In contrast, the intestinal architecture is still intact in WT and Sparc−/− mice. (B) BM counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment indicate that all mice dying from serial 5-FU treatment show severe aplastic anemia. (C) WBC counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment. All mice dying from serial 5-FU treatment show severe leukopenia. (D) RBC counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment. All mice dying from serial 5-FU treatment show severe anemia. (E) Platelet counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment. All mice dying from serial 5-FU treatment show severe thrombocytopenia. Each data point represents an individual mouse. N = 6-7 per group; mean; ****P < .001; unpaired 2-tailed Student t test).
WT and SPARC-deficient mice die of hematopoietic failure in response to serial 5-FU treatment. (A) Hematoxylin and eosin stainings of bone and gut sections of WT and Sparc−/− mice dying from serial 5-FU treatment (age at start of treatment, 8 weeks; age at examination, 14 and 16 weeks for WT and Sparc−/− mice, respectively). Trabecular and central bone regions are aplastic, suggesting WT and Sparc−/− mice die of hematopoietic failure. Examples for aplastic BM regions are indicated with arrowheads. In contrast, the intestinal architecture is still intact in WT and Sparc−/− mice. (B) BM counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment indicate that all mice dying from serial 5-FU treatment show severe aplastic anemia. (C) WBC counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment. All mice dying from serial 5-FU treatment show severe leukopenia. (D) RBC counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment. All mice dying from serial 5-FU treatment show severe anemia. (E) Platelet counts of untreated and WT and Sparc−/− mice dying from serial 5-FU treatment. All mice dying from serial 5-FU treatment show severe thrombocytopenia. Each data point represents an individual mouse. N = 6-7 per group; mean; ****P < .001; unpaired 2-tailed Student t test).
Hematopoietic systems of WT and SPARC-deficient mice recover with similar kinetics after 5-FU treatment
A possible explanation for the observed phenotype could be that the hematopoietic system of SPARC-deficient mice recovers faster than that of WT mice after 5-FU–induced injury. To address this possibility, we injected WT and Sparc−/− mice once with 5-FU and monitored the hematological recovery at 3-day intervals. RBC, WBC, and platelet counts of WT and Sparc−/− mice followed comparable kinetics after 5-FU injection (supplemental Figure 5A-C).
Next, we analyzed the BM of WT and Sparc−/− mice at different time points after a single 5-FU injection. Total BM cellularity was identical at all time points comparing WT and Sparc−/− mice (Figure 3A). Moreover, we did not observe significant differences in absolute numbers of B220+ B cells, CD4+/CD8+ T cells, Ter119+ erythroid cells, and Gr1+/CD11b+ myeloid cells between WT and Sparc−/− mice at homeostasis or 5, 7, 10, and 11 days after 5-FU as determined by FACS (Figure 3B and supplemental Figure 5D-F). Together, these results suggest that Sparc−/− mice recover as fast as WT mice from 5-FU–induced stress.
SPARC-deficient mice have a normal hematopoietic recovery following 5-FU treatment. (A) No significant differences in total BM cellularity (arms, legs, hips, and spine) are observed between WT and Sparc−/− mice following 5-FU treatment (N = 12 per group and time point; mean and standard deviation [SD]; unpaired 2-tailed Student t test). (B) In the BM, there are no significant differences in absolute numbers of Gr1+/CD11b+ myeloid cells between WT and Sparc−/− mice at homeostasis and after 5-FU treatment (N = 12 per group and time point; mean and SD; unpaired 2-tailed Student t test). (C-D) Sparc−/− mice have significantly less (C) HSCs (Lin−Sca-1+ CD48−CD150+ CD34−) and (D) SLAM HSCs (Lin−Sca-1+CD48−CD150+) 11 days after 5-FU (N = 12 per group and time point; mean and SD; ***P < .005; ****P < .001; unpaired Student 2-tailed t test). (E-F) Absolute numbers of LSK and LS−K (E) and HSCs (F; Lin−Sca-1+c-Kit+CD48−CD150+CD34−) in WT and Sparc−/− mice 11 days after 5-FU injection (N = 12 per group and time point; mean and SD; **P < .01; unpaired 2-tailed Student t test).
SPARC-deficient mice have a normal hematopoietic recovery following 5-FU treatment. (A) No significant differences in total BM cellularity (arms, legs, hips, and spine) are observed between WT and Sparc−/− mice following 5-FU treatment (N = 12 per group and time point; mean and standard deviation [SD]; unpaired 2-tailed Student t test). (B) In the BM, there are no significant differences in absolute numbers of Gr1+/CD11b+ myeloid cells between WT and Sparc−/− mice at homeostasis and after 5-FU treatment (N = 12 per group and time point; mean and SD; unpaired 2-tailed Student t test). (C-D) Sparc−/− mice have significantly less (C) HSCs (Lin−Sca-1+ CD48−CD150+ CD34−) and (D) SLAM HSCs (Lin−Sca-1+CD48−CD150+) 11 days after 5-FU (N = 12 per group and time point; mean and SD; ***P < .005; ****P < .001; unpaired Student 2-tailed t test). (E-F) Absolute numbers of LSK and LS−K (E) and HSCs (F; Lin−Sca-1+c-Kit+CD48−CD150+CD34−) in WT and Sparc−/− mice 11 days after 5-FU injection (N = 12 per group and time point; mean and SD; **P < .01; unpaired 2-tailed Student t test).
Analysis of the HSC compartment, however, revealed that, although HSC numbers were similar between WT and Sparc−/− mice at homeostasis and 5, 7, and 10 days after 5-FU treatment, HSC numbers were reduced in Sparc−/− mice 11 days after 5-FU injection (Figure 3C-D). This reduction in HSC numbers seems to be specific to HSCs (Figure 3E-F).
In summary, the kinetics of recovery from 5-FU–induced damage to the hematopoietic system in Sparc−/− mice is similar to that of WT mice, as concluded from quantification studies of mature hematopoietic cells in blood and BM. However, our data uncover that the expansion of HSCs following 5-FU treatment ceases earlier in Sparc−/− mice compared with WT controls.
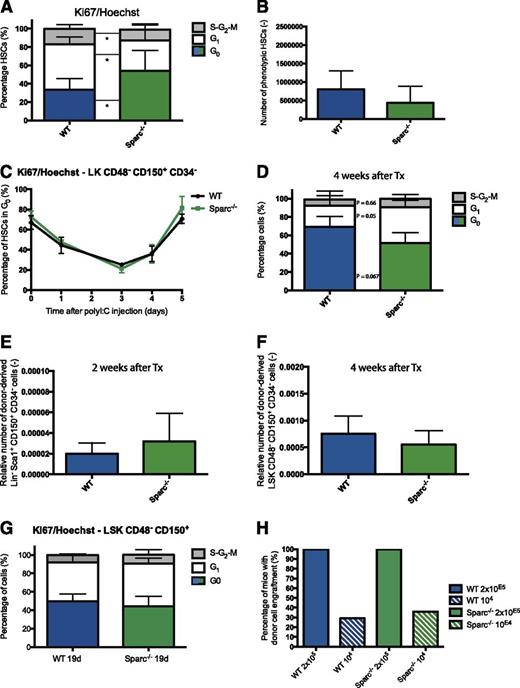
Accelerated return of HSCs to quiescence after 5-FU in SPARC-deficient mice
We hypothesized that the reduced sensitivity of SPARC-deficient mice to 5-FU could be due to an accelerated return to quiescence of the HSC population, which would protect them from the subsequent dose of 5-FU. Therefore, WT and Sparc−/− mice were treated with 5-FU at different time points prior to analysis, and the proliferation status of their HSCs was assessed by cell cycle analysis using Ki67/Hoechst staining. Strikingly, HSCs in Sparc−/− mice return to quiescence faster than in the WT situation (Figure 4A-B and supplemental Figure 6). The results obtained with the Ki67/Hoechst staining were confirmed with an in vivo BrdU assay. We detected significantly less BrdU+ HSCs in Sparc−/− mice compared with WT mice 10 and 11 days after 5-FU treatment (Figure 4C and supplemental Figure 7). Because 5-FU only affects cycling cells, WT mice harbor a higher fraction of HSCs 10 days after initial 5-FU treatment that are targets for a second 5-FU dose. Therefore, the presence of more quiescent cells provides a mechanistic explanation as to why SPARC-deficient mice are less susceptible to death induced by serial 5-FU injections at 10-day intervals.
HSCs of SPARC-deficient mice return to quiescence faster after 5-FU treatment. (A) FACS plot and quantification of time course of Ki67/Hoechst cell cycle analysis of HSCs (Lin−Sca-1+CD48−CD150+CD34−) of WT and Sparc−/− mice after 5-FU treatment (N = 12 per group and time point; mean and SD). c-Kit was omitted from the gating strategy as c-Kit expression drops after 5-FU treatment.7 (B) WT and Sparc−/− mice: percentage of HSCs in G0 phase of cell cycle at homeostasis and at different time points after 5-FU treatment (N = 12 per group and time point; mean and SD; ****P < .001; unpaired 2-tailed Student t test). In SPARC-deficient mice, HSCs return to quiescence more rapidly following 5-FU treatment. (C) WT and Sparc−/− mice: percentage of BrdU+ HSCs at homeostasis and at different time points after 5-FU treatment (N = 6 per group and time point; mean and SD; *P < .05; ****P < .001; unpaired 2-tailed Student t test). (D) Survival curve of WT and Sparc−/− mice treated with 5-FU at a dose of 150 μg/g at 7-day intervals (N = 10 per group; median survival: WT = 15.5 days, Sparc−/− = 17 days; no significant difference; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (E) Survival curve of WT and Sparc−/− mice treated with 5-FU at a dose of 150 μg/g at 11-day intervals (N = 13-14 per group; median survival: WT = 52.5 days, Sparc−/− = 79 days; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test).
HSCs of SPARC-deficient mice return to quiescence faster after 5-FU treatment. (A) FACS plot and quantification of time course of Ki67/Hoechst cell cycle analysis of HSCs (Lin−Sca-1+CD48−CD150+CD34−) of WT and Sparc−/− mice after 5-FU treatment (N = 12 per group and time point; mean and SD). c-Kit was omitted from the gating strategy as c-Kit expression drops after 5-FU treatment.7 (B) WT and Sparc−/− mice: percentage of HSCs in G0 phase of cell cycle at homeostasis and at different time points after 5-FU treatment (N = 12 per group and time point; mean and SD; ****P < .001; unpaired 2-tailed Student t test). In SPARC-deficient mice, HSCs return to quiescence more rapidly following 5-FU treatment. (C) WT and Sparc−/− mice: percentage of BrdU+ HSCs at homeostasis and at different time points after 5-FU treatment (N = 6 per group and time point; mean and SD; *P < .05; ****P < .001; unpaired 2-tailed Student t test). (D) Survival curve of WT and Sparc−/− mice treated with 5-FU at a dose of 150 μg/g at 7-day intervals (N = 10 per group; median survival: WT = 15.5 days, Sparc−/− = 17 days; no significant difference; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (E) Survival curve of WT and Sparc−/− mice treated with 5-FU at a dose of 150 μg/g at 11-day intervals (N = 13-14 per group; median survival: WT = 52.5 days, Sparc−/− = 79 days; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test).
If the survival advantage of SPARC-deficient mice in response to a 10-day 5-FU regimen is due to the accelerated return of their HSCs to quiescence, then SPARC-deficient mice should not show such a reduced sensitivity in a 7-day regimen, because the proliferative activity of their HSCs was identical to WT controls at this time point after 5-FU treatment (Figure 4B). Indeed, there was no significant difference in survival of WT and Sparc−/− mice injected with 5-FU at 7-day intervals (Figure 4D). However, 11 days after 5-FU treatment, HSCs in Sparc−/− mice have largely returned to a quiescent state in contrast to approximately half of the HSCs in WT mice. Accordingly, we could recapitulate the reduced sensitivity of SPARC-deficient mice observed in the 5-FU 10-day regimen also with an 11-day regimen (Figure 4E). Moreover, we could demonstrate that the absence of SPARC expression by niche cells is sufficient for the accelerated return of HSCs to quiescence after 5-FU treatment, as this phenomenon could also be observed in WT and Sparc−/− mice previously transplanted with WT BM (Figure 5A-B).
Accelerated return of HSCs to quiescence in the absence of SPARC is niche dependent and specific to 5-FU. (A) WT and Sparc−/− mice were transplanted with WT BM. Twenty weeks later, mice were treated with 5-FU (120 μg/g), and cell cycle status of HSCs was determined 10 days later by Ki67/Hoechst staining (N = 8-11 per group and time point; mean and SD; *P < .05; unpaired 2-tailed Student t test). (B) HSC (Lin−Sca-1+CD48−CD150+CD34−) numbers in WT and Sparc−/− reverse chimeras 10 days after 5-FU. (C) WT and Sparc−/− mice were treated with polyI:C at different time points prior to cell cycle analysis with Ki67/Hoechst (N = 6 per group and time point; mean and SD). (D-F) 106 WT BM cells were transplanted into lethally irradiated WT and Sparc−/− recipients, and (D) HSC cell cycle status was analyzed with Ki67/Hoechst after 4 weeks (N = 4-6 per group and time point; mean and SD; P values are shown) and HSC frequencies after (E) 2 and (F) 4 weeks. (G) Cell cycle analysis of HSCs of 19-day-old WT and Sparc−/− mice using Ki67/Hoechst (N = 4 per group and time point; mean and SD). (H) Saturating (2 × 105) and limiting (104) numbers of CD45.1 WT BM cells were transplanted into irradiated (2 × 5 Gy) WT or Sparc−/− recipient mice. Donor chimerism of surviving recipient mice was analyzed after 4 weeks.
Accelerated return of HSCs to quiescence in the absence of SPARC is niche dependent and specific to 5-FU. (A) WT and Sparc−/− mice were transplanted with WT BM. Twenty weeks later, mice were treated with 5-FU (120 μg/g), and cell cycle status of HSCs was determined 10 days later by Ki67/Hoechst staining (N = 8-11 per group and time point; mean and SD; *P < .05; unpaired 2-tailed Student t test). (B) HSC (Lin−Sca-1+CD48−CD150+CD34−) numbers in WT and Sparc−/− reverse chimeras 10 days after 5-FU. (C) WT and Sparc−/− mice were treated with polyI:C at different time points prior to cell cycle analysis with Ki67/Hoechst (N = 6 per group and time point; mean and SD). (D-F) 106 WT BM cells were transplanted into lethally irradiated WT and Sparc−/− recipients, and (D) HSC cell cycle status was analyzed with Ki67/Hoechst after 4 weeks (N = 4-6 per group and time point; mean and SD; P values are shown) and HSC frequencies after (E) 2 and (F) 4 weeks. (G) Cell cycle analysis of HSCs of 19-day-old WT and Sparc−/− mice using Ki67/Hoechst (N = 4 per group and time point; mean and SD). (H) Saturating (2 × 105) and limiting (104) numbers of CD45.1 WT BM cells were transplanted into irradiated (2 × 5 Gy) WT or Sparc−/− recipient mice. Donor chimerism of surviving recipient mice was analyzed after 4 weeks.
In summary, although the kinetics of mature blood cell recovery is normal, HSCs in a SPARC-deficient niche show an accelerated return to quiescence, which protects them from the lethal effects of serial 5-FU treatment.
Faster return of HSCs to quiescence in absence of SPARC is specific to 5-FU
To address whether SPARC affects the return of HSCs to quiescence following other stimuli, we analyzed the HSC cell cycle following polyI:C treatment in WT and Sparc−/− mice (Figure 5C) or following transplantation of WT HSCs into lethally irradiated WT and Sparc−/− recipients (Figure 5D-F). Additionally, we compared HSC cell cycle in 19-day-old WT and Sparc−/− mice (Figure 5G), as WT HSCs switch from an activated to a quiescent phenotype between 3 and 4 weeks of age.32,33 We did not observe significant differences in HSC cycling in any of these situations, suggesting that the effect of SPARC on the reacquisition of HSC quiescence is rather specific for 5-FU treatment. Of note, transplantation of limiting numbers of WT BM cells into irradiated WT and Sparc−/− recipients revealed that both niches support HSC homing and engraftment equally well (Figure 5H).
Accelerated return of HSCs to quiescence in SPARC-deficient mice is independent of CD81 and TGF-β signaling
A recent report has suggested a role for CD81 in the re-entry of HSCs into quiescence after 5-FU.34 We observed comparable CD81 expression on HSCs isolated from SPARC-deficient and WT mice following 5-FU treatment, suggesting that the difference in cell cycle re-entry in Sparc−/− mice is not regulated via CD81 levels (Figure 6A).
Accelerated return of HSCs to quiescence in SPARC-deficient mice is independent of TGF-β signaling. (A) CD81 expression is identical between HSCs in WT and Sparc−/− mice and shows the same changes in response to 5-FU (N = 4 per group and time point; mean and SD). (B) Levels of active TGF-β are comparable in WT and SPARC-deficient mice at homeostasis and at different time points after 5-FU treatment (N = 6 per group and time point; mean and SD). (C) Ki67/Hoechst cell cycle analysis of WT and Sparc−/− mice 11 days after 5-FU. Additionally, mice received either the TGF-β blocking antibody 2G7 or isotype control IgG1 at days 8 and 10 after 5-FU injection. TGF-β pathway inhibition delays HSC quiescence induction in WT but not Sparc−/− mice (N = 6 per group and time point; mean and SD; *P < .05; ***P < .005; ****P < .001; unpaired 2-tailed Student t test). (D) p27 mRNA expression in HSCs (Lin−Sca-1+CD48−CD150+CD34−) before and 9 or 10 days after 5-FU. (E) Survival curve of Sparcflox2 and MxCre;Sparcflox2 mice treated with 5-FU at a dose of 150 μg/g at 10-day intervals starting 5 weeks after deletion (N = 8-9 per group; median survival: Sparcflox2 = 45 days, MxCre;Sparcflox2 = 50 days; no significant difference; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (F) Niche cell frequencies of WT and Sparc−/− mice 10 days after 5-FU and at baseline. Niche cells were isolated from bone chips and identified with the indicated markers by flow cytometry (N = 4 per group and time point; mean and SD). (G) SPARC mRNA expression in niche cells of WT mice before and 5 or 10 days after 5-FU (N = 6 per group and time point; mean and SD; *P < .05; **P < .01; ***P < .005; 1-way ANOVA followed by Dunnett’s multiple comparison test). (H) SPARC mRNA expression in hematopoietic progenitors of WT mice before and 5 or 10 days after 5-FU (N = 6 per group and time point; mean and SD; *P < .05; **P < .01; 1-way ANOVA followed by Dunnett’s multiple comparison test).
Accelerated return of HSCs to quiescence in SPARC-deficient mice is independent of TGF-β signaling. (A) CD81 expression is identical between HSCs in WT and Sparc−/− mice and shows the same changes in response to 5-FU (N = 4 per group and time point; mean and SD). (B) Levels of active TGF-β are comparable in WT and SPARC-deficient mice at homeostasis and at different time points after 5-FU treatment (N = 6 per group and time point; mean and SD). (C) Ki67/Hoechst cell cycle analysis of WT and Sparc−/− mice 11 days after 5-FU. Additionally, mice received either the TGF-β blocking antibody 2G7 or isotype control IgG1 at days 8 and 10 after 5-FU injection. TGF-β pathway inhibition delays HSC quiescence induction in WT but not Sparc−/− mice (N = 6 per group and time point; mean and SD; *P < .05; ***P < .005; ****P < .001; unpaired 2-tailed Student t test). (D) p27 mRNA expression in HSCs (Lin−Sca-1+CD48−CD150+CD34−) before and 9 or 10 days after 5-FU. (E) Survival curve of Sparcflox2 and MxCre;Sparcflox2 mice treated with 5-FU at a dose of 150 μg/g at 10-day intervals starting 5 weeks after deletion (N = 8-9 per group; median survival: Sparcflox2 = 45 days, MxCre;Sparcflox2 = 50 days; no significant difference; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (F) Niche cell frequencies of WT and Sparc−/− mice 10 days after 5-FU and at baseline. Niche cells were isolated from bone chips and identified with the indicated markers by flow cytometry (N = 4 per group and time point; mean and SD). (G) SPARC mRNA expression in niche cells of WT mice before and 5 or 10 days after 5-FU (N = 6 per group and time point; mean and SD; *P < .05; **P < .01; ***P < .005; 1-way ANOVA followed by Dunnett’s multiple comparison test). (H) SPARC mRNA expression in hematopoietic progenitors of WT mice before and 5 or 10 days after 5-FU (N = 6 per group and time point; mean and SD; *P < .05; **P < .01; 1-way ANOVA followed by Dunnett’s multiple comparison test).
TGF-β signaling has been shown recently to be a major regulator of HSC quiescence35,36 and to be negatively regulated by SPARC in pericytes.37 Thus, we speculated that in the absence of SPARC, enhanced TGF-β signaling might be responsible for the accelerated return of HSCs to quiescence. To address this, we used enzyme-linked immunosorbent assays to quantify the levels of active TGF-β in BM supernatants of WT and Sparc−/− mice under homeostatic conditions, as well as at different time points following 5-FU treatment (Figure 6B). Our data did not reveal any significant difference. Mechanistically, SPARC was reported to inhibit TGF-β signaling by binding to endoglin, which is part of the TGF-β receptor complex, thereby counteracting endoglin interaction with αV integrin.37 This would suggest that SPARC might inhibit the TGF-β pathway independently of its ability to modulate the levels of active TGF-β. To address this hypothesis, we evaluated the effect of a TGF-β inhibitory antibody (2G7) administered on days 8 and 10 following 5-FU treatment of Sparc−/− and control mice. HSC cycling was analyzed on day 11 after 5-FU treatment. Strikingly, TGF-β inhibition only reduced the percentage of quiescent WT HSCs, whereas the re-entry to quiescence in the SPARC-deficient setting was unaffected by TGF-β inhibition (Figure 6C). Thus, the accelerated re-entry of HSCs to quiescence in the SPARC-deficient setting after 5-FU–induced injury seems to be independent of the TGF-β pathway.
In agreement with the accelerated return to quiescence of HSCs in Sparc−/− mice, we found p27 mRNA levels to be increased by twofold in SPARC-deficient HSCs compared with control HSCs isolated at both 9 and 10 days after 5-FU (Figure 6D).
SPARC and the niche
To further delineate the specific cell type in the niche that is responsible for SPARC-mediating effects on HSC cycling, we used the MxCre driver line to induce targeted deletion in both hematopoietic and osteolineage cells.19,38 Therefore, we asked whether MxCre;Sparcflox2 mice 5 weeks after polyI:C treatment have a survival benefit in a serial 5-FU experiment compared with Sparcflox2 controls (Figure 6E). No significant difference in survival was observed between the 2 groups, suggesting that the absence of SPARC expression by hematopoietic and osteolineage cells is not sufficient to trigger a survival benefit.
Next we asked whether different sensitivities of niche cells to 5-FU may account for the accelerated return of HSCs to quiescence in the absence of SPARC. As such, we analyzed the frequency of niche cells in SPARC-deficient and control animals at baseline and 10 days after 5-FU treatment (Figure 6F). No difference was observed.
Finally, we tested whether SPARC expression by hematopoietic stem/progenitor and niche cells was affected by 5-FU treatment. We could observe a significant increase in SPARC expression in hematopoietic stem and progenitor cells with a concomitant decrease in niche cells, which are the main cells producing SPARC in the BM (Figure 6G-H).
Discussion
Our most important finding is the protective effect of the absence of SPARC for HSCs during cyclic chemotherapy treatment. SPARC was identified as part of a cluster of extracellular matrix-related genes highly expressed in HSCs that have recently colonized the BM compared with HSCs still residing in the liver of newborn mice. This suggests that HSCs actively remodel their new BM niche by secreting these factors. Together, upregulation of this cluster may be crucial for seeding and engraftment of HSCs in the BM.
We show that SPARC-deficient mice have normal HSC numbers and that their HSCs perform as well as WT HSCs in competitive transplantation assays. These data are in accordance with a recent study by the Karlsson group, who reported normal numbers of immunophenotypic and functional HSCs using a different SPARC knockout mouse model.13
Our study demonstrates that SPARC-deficient mice have a reduced sensitivity to serial 5-FU injections, with a significant proportion of mice even acquiring resistance to 5-FU. Our data strongly suggest that this difference is due to a protective effect of SPARC deficiency on the hematopoietic system, as WT and SPARC-deficient mice that die of serial 5-FU treatment are severely pancytopenic at the time of death. A survival advantage in serial 5-FU experiments could also be observed in reverse chimeras, where the niche is SPARC deficient, but not in straight chimeras, where the hematopoietic system lacks SPARC. This demonstrates that the reduced sensitivity of SPARC-deficient mice toward 5-FU is largely due to lack of SPARC expression by non-hematopoietic cells. This is further supported by the observation that niche cells express extremely high levels of SPARC mRNA compared with HSCs.
Most importantly, we could demonstrate an accelerated return of HSCs to quiescence in SPARC-deficient mice following 5-FU. These data strongly suggest that a SPARC-deficient niche provides mice with a survival benefit in serial 5-FU treatment, as their HSCs return to quiescence faster. We also observed reduced numbers of phenotypic HSCs in SPARC-deficient mice 11 days after 5-FU treatment, which are accounted for by their accelerated return to quiescence resulting in reduced expansion of the HSC pool. In contrast, mature components of the hematopoietic system fully recover at normal speed in SPARC-deficient mice, suggesting that in SPARC-deficient mice, HSCs stop proliferating and return to quiescence when the hematopoietic system is already completely recovered, whereas their WT counterparts initially overcompensate and continue to proliferate for a short period of time.
Several niche-derived factors have been suggested to promote HSC quiescence, including membrane-bound stem cell factor, thrombopoietin, angiopoietin-1, and TGF-β.35,36,39-41 Possibly, SPARC inhibits signaling induced by 1 of these factors. In fact, as reported in a recent study, TGF-β signaling plays a key role in the return of HSCs to quiescence and the restoration of hematopoietic homeostasis after myelosuppressive chemotherapy.42 Interestingly, induction of HSC quiescence in the absence of SPARC proved to be independent of the TGF-β pathway, suggesting that loss of SPARC acts via a different mechanism to promote the induction of HSC quiescence after injury. It is possible that SPARC directly affects HSC proliferation by modulating their adhesion to adjacent niche cells or specific extracellular matrix components.43
In addition to its widespread implication in solid tumors and metastases, SPARC has also been associated with a number of hematologic malignancies. The outcome of SPARC deregulation seems to be cell type specific. In some cancer types, SPARC functions as a tumor suppressor, whereas in others, aberrant SPARC expression is related to poor prognosis.44 SPARC is deleted in del(5q) myelodysplastic syndrome and is low in acute myeloid leukemia, with rearrangements in the mixed-lineage leukemia gene,11,15,45 whereas it is highly overexpressed in imatinib-resistant chronic myeloid leukemia cells.46 More recently, SPARC overexpression was reported to promote acute myeloid leukemia growth in a xenotransplantation mouse model and to predict poor outcome.47 In addition, cell extrinsic SPARC expression is of relevance for prognosis. For instance, absence of stromal SPARC expression predicts poor prognosis in diffuse large B-cell lymphoma.48
Future work in this area may provide novel insights into how SPARC expression by niche cells affects the behavior of leukemic cells and might provide therapeutic options. In addition, inhibition of SPARC using inhibitory peptides or antibodies may alleviate the side effects of patients receiving chemotherapy, as this may be a possible strategy to protect healthy HSCs. Similarly, SPARC inhibitory peptides have been successfully used to inhibit laser-induced choroidal neovascularization in mice.49 In conclusion, this study reports a novel aspect of SPARC function in the HSC niche that may prove relevant for clinical practice in hematology and oncology.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Drs Melania Tesio, Aine Prendergast, and Gerhard Ehninger for critical reading of the manuscript and related discussions. The authors thank Melanie Neubauer, Petra Zeisberger, and Andrea Takacs for genetic screening of the animals and technical help, as well as the staff of the animal facility of the German Cancer Research Center (DKFZ) for animal husbandry.
Support by the DKFZ Flow Cytometry Service Unit, DKFZ Genomics and Proteomics Core Facility, and DKFZ Light Microscopy Facility is gratefully acknowledged. This work was supported by the BioRN Spitzencluster “Molecular and Cell Based Medicine” supported by the German Bundesministerium für Bildung und Forschung, the Forschergruppe FOR2033 “The Hematopoietic Niches” funded by the Deutsche Forschungsgemeinschaft, and the Dietmar Hopp Foundation.
Authorship
Contribution: A.E., G.O., and A.T. designed the experiments and interpreted data; A.E., T.B., and H.M. performed research and analyzed data; A.E. and A.T. wrote the manuscript; and K.M. performed research.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Andreas Trumpp, Im Neuenheimer Feld 280, D-69120 Heidelberg, Germany; e-mail: a.trumpp@dkfz-heidelberg.de.

![Figure 1. SPARC-deficient mice are less sensitive to serial 5-FU injections due to the absence of SPARC expression by niche cells. (A) SPARC mRNA expression by cell type of the adult BM niche including mature osteoblasts (mOBs), osteoprogenitors (iOBs), and the fraction containing mesenchymal stem cells (MSCs) and endothelial cells (ECs) (N = 10 per group; mean and SD). (B) SPARC-deficient mice show enhanced survival when injected with 5-FU at a dose of 150 μg/g at 10-day intervals (N = 10-11 per group; median survival: WT = 43 days, Sparc−/− = 71 days; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (C) Straight chimeras that lack SPARC expression by hematopoietic cells have no survival benefit in the serial 5-FU experiment. C57Bl/6J mice were transplanted with WT (littermate control) or Sparc−/− BM, and 5-FU treatment (120 μg/g at 10-day intervals) was started 12 weeks after transplantation (N = 9; median survival: WT = 23 days, Sparc−/− = 20 days; no significant difference). (D) Lack of SPARC expression by non-hematopoietic cells is sufficient to provide a survival benefit in the serial 5-FU experiment. WT or Sparc−/− mice were transplanted with WT BM (CD45.1/2), and 5-FU treatment (120 μg/g at 10-day intervals) was started 12 weeks after transplantation. (N = 13-17; median survival: WT = 42 days, Sparc−/− = 169; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/123/26/10.1182_blood-2013-10-533711/4/m_4054f1.jpeg?Expires=1765914119&Signature=R9POpC0YdZmqf6YZvoNLMMWihHQ5tY-ntlBd4zgivTk2aNXg0J7RXrbbAI0hV10-o93sNNMICzAVHbRoJbkdVIIzMUWBYM7pN7Inc8xdJQ1We2xBtwC1IfLeHUJJdOh8LybLMve6O4AsH7aHCsTF5UXIQAYhy4KrY7wtjFcvkagRrbs5E-m4ECtb1NG2nxcCjdt-zoIjoxe1Pd4VUvIerC3NDTJCdLbF4MIBb9PWiIxeSP2lg1AGjlRCqXFYDSdd1U-AyfNEUPWoLMCsJlq5CLQn9P3DtYpPPQ5RGBVUKZ6SAO31qh-T~R2rJzpOmEQYxz8KszXHZNMoFQB7c4gOEg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 3. SPARC-deficient mice have a normal hematopoietic recovery following 5-FU treatment. (A) No significant differences in total BM cellularity (arms, legs, hips, and spine) are observed between WT and Sparc−/− mice following 5-FU treatment (N = 12 per group and time point; mean and standard deviation [SD]; unpaired 2-tailed Student t test). (B) In the BM, there are no significant differences in absolute numbers of Gr1+/CD11b+ myeloid cells between WT and Sparc−/− mice at homeostasis and after 5-FU treatment (N = 12 per group and time point; mean and SD; unpaired 2-tailed Student t test). (C-D) Sparc−/− mice have significantly less (C) HSCs (Lin−Sca-1+ CD48−CD150+ CD34−) and (D) SLAM HSCs (Lin−Sca-1+CD48−CD150+) 11 days after 5-FU (N = 12 per group and time point; mean and SD; ***P < .005; ****P < .001; unpaired Student 2-tailed t test). (E-F) Absolute numbers of LSK and LS−K (E) and HSCs (F; Lin−Sca-1+c-Kit+CD48−CD150+CD34−) in WT and Sparc−/− mice 11 days after 5-FU injection (N = 12 per group and time point; mean and SD; **P < .01; unpaired 2-tailed Student t test).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/123/26/10.1182_blood-2013-10-533711/4/m_4054f3.jpeg?Expires=1765914119&Signature=OZIeRzbuX5AW1pwoMj17XOoOXkcCipMcYl6tavVtM2tYKkFXFdT-nnnnKKS2H6LGOQiDKkI~5KUytjVFjmkoQ1mHLdrYZm8UQ8uIwu8gbCTR8srhDfDr2vp9k6HUpvqgUfvutiF8kQQZIxz8sYA4umD1TbJ5AyP9xtblPnTNIrzuZjpZOm8q3dCnhMlPqR8Bk4kf2WhonbI1LVZpxkKUsnMuuCRgo-Pq0n9HYg4Q06UKyCLP87Nd93v2IoNZlif01omuyUiIToXoq9KHkO5U8htrWAUQXZjX2eGQa849hlzZnQtUy3Z37Cafk-Unv7mGCILdqeeM1HXZsda8c7pGOg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. HSCs of SPARC-deficient mice return to quiescence faster after 5-FU treatment. (A) FACS plot and quantification of time course of Ki67/Hoechst cell cycle analysis of HSCs (Lin−Sca-1+CD48−CD150+CD34−) of WT and Sparc−/− mice after 5-FU treatment (N = 12 per group and time point; mean and SD). c-Kit was omitted from the gating strategy as c-Kit expression drops after 5-FU treatment.7 (B) WT and Sparc−/− mice: percentage of HSCs in G0 phase of cell cycle at homeostasis and at different time points after 5-FU treatment (N = 12 per group and time point; mean and SD; ****P < .001; unpaired 2-tailed Student t test). In SPARC-deficient mice, HSCs return to quiescence more rapidly following 5-FU treatment. (C) WT and Sparc−/− mice: percentage of BrdU+ HSCs at homeostasis and at different time points after 5-FU treatment (N = 6 per group and time point; mean and SD; *P < .05; ****P < .001; unpaired 2-tailed Student t test). (D) Survival curve of WT and Sparc−/− mice treated with 5-FU at a dose of 150 μg/g at 7-day intervals (N = 10 per group; median survival: WT = 15.5 days, Sparc−/− = 17 days; no significant difference; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (E) Survival curve of WT and Sparc−/− mice treated with 5-FU at a dose of 150 μg/g at 11-day intervals (N = 13-14 per group; median survival: WT = 52.5 days, Sparc−/− = 79 days; ****P < .001; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/123/26/10.1182_blood-2013-10-533711/4/m_4054f4.jpeg?Expires=1765914119&Signature=2axUCAJacaQ7AbCgfi5DzVBuij6wd1qQ2fRpFO6Qx~JaIJYAemS9vizUsXJaNjgiMj8ay9RFEtEP2171PYG3jCS1nHnRRmWBn2hsSYHUQJxzt1qNiXx5ezXC0WBse8D-CCTtI6mKu9QvJ3VazWQyChEOkGDxp7swEV2KFkhv9hn9B3~pETmJZsxyR7dNb-~JqNLltgauj-MA07ZpvcrEKnnreeKex5SDe0MQ1Jc4Rr5guZXe3xRrQgKRIDLMl5u1CIJapRW1FMqcqg2LsIIZM0M0yNVTLEnhKVuI05RkR-WZqv~E5L6mAhmdbGMVqCNrp4NWDq~fhpUVH1iZaeuj7w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. Accelerated return of HSCs to quiescence in SPARC-deficient mice is independent of TGF-β signaling. (A) CD81 expression is identical between HSCs in WT and Sparc−/− mice and shows the same changes in response to 5-FU (N = 4 per group and time point; mean and SD). (B) Levels of active TGF-β are comparable in WT and SPARC-deficient mice at homeostasis and at different time points after 5-FU treatment (N = 6 per group and time point; mean and SD). (C) Ki67/Hoechst cell cycle analysis of WT and Sparc−/− mice 11 days after 5-FU. Additionally, mice received either the TGF-β blocking antibody 2G7 or isotype control IgG1 at days 8 and 10 after 5-FU injection. TGF-β pathway inhibition delays HSC quiescence induction in WT but not Sparc−/− mice (N = 6 per group and time point; mean and SD; *P < .05; ***P < .005; ****P < .001; unpaired 2-tailed Student t test). (D) p27 mRNA expression in HSCs (Lin−Sca-1+CD48−CD150+CD34−) before and 9 or 10 days after 5-FU. (E) Survival curve of Sparcflox2 and MxCre;Sparcflox2 mice treated with 5-FU at a dose of 150 μg/g at 10-day intervals starting 5 weeks after deletion (N = 8-9 per group; median survival: Sparcflox2 = 45 days, MxCre;Sparcflox2 = 50 days; no significant difference; log-rank [Mantel-Cox] test and Gehan-Breslow-Wilcoxon test). Time points of 5-FU injections are indicated with arrows. (F) Niche cell frequencies of WT and Sparc−/− mice 10 days after 5-FU and at baseline. Niche cells were isolated from bone chips and identified with the indicated markers by flow cytometry (N = 4 per group and time point; mean and SD). (G) SPARC mRNA expression in niche cells of WT mice before and 5 or 10 days after 5-FU (N = 6 per group and time point; mean and SD; *P < .05; **P < .01; ***P < .005; 1-way ANOVA followed by Dunnett’s multiple comparison test). (H) SPARC mRNA expression in hematopoietic progenitors of WT mice before and 5 or 10 days after 5-FU (N = 6 per group and time point; mean and SD; *P < .05; **P < .01; 1-way ANOVA followed by Dunnett’s multiple comparison test).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/123/26/10.1182_blood-2013-10-533711/4/m_4054f6.jpeg?Expires=1765914119&Signature=i9HY874uhapXfZGroFpD7rnEnQlcSWDHf01696lMmV-hYwv0dpkuuJW8THRssr3uXGGejEM-lt7vGA8OKZdhWsBcv3lUpwrBumd3YFtno7M1EGyc9RjAOOv-7SqNrm4sGmLO4rqvW3DzQ0cjd40lMQmsTBxw2KIc~7ahl1UfkINvrY2RsziuGJLSVjexv7cB4dEQ0ZVOnwGVYJyybvMe851oX8PJQYMJKbaOeOPjT0eIK-qwwP6lJ69aO0x19GFuadYEkFlYxbtjR2LTCYuKcSJOhpWho8BAeRC71BWJK-VnkflNMOU~i~d8-zPk3v-qTFoM8--UprwYMMEk2oOtuw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal