Key Points
In a randomized phase 3 trial, overall response rates, PFS, and overall survival were similar between MPT-T and mPR-R.
Toxicity with both regimens was common, but mPR-R was better tolerated, and patients on the mPR-R regimen reported better quality of life.
Abstract
This phase 3 trial (Eastern Cooperative Oncology Group [ECOG] E1A06) compared melphalan, prednisone, and thalidomide (MPT-T) with melphalan, prednisone, and lenalidomide (mPR-R) in patients with untreated multiple myeloma (MM). A noninferiority design was used, and inferiority was defined as a progression-free survival (PFS) hazard ratio (HR) of MPT-T/mPR-R ≤0.82. A total of 306 patients enrolled, with a median age of 75.7 years. Median follow-up was 40.7 months. Median time on therapy was 12.1 months and 23.1 months for the 46.6% of treated patients who received maintenance, with no differences by arm. Median PFS was 21 months on MPT-T and 18.7 months on mPR-R (HR, 0.84; 95% confidence interval, 0.64-1.09). Overall survival was 52.6 months (MPT-T) vs 47.7 months (mPR-R) (P = .476). Per-protocol response rates were 63.6% (MPT-T) and 59.9% (mPR-R) (P = .557). Grade ≥3 nonhematologic toxicity was 59.5% for MPT-T vs 40.0% for mPR-R (P = .001). Second malignancies were observed in 18 MPT-T patients vs 14 mPR-R patients. Quality-of-life analysis favored mPR-R by induction end (P = .007). Use of MPT-T or mPR-R in elderly patients with untreated MM demonstrates no statistical or clinically relevant differences in response rates, PFS, and OS; however, quality of life at end of induction was improved and lower toxicity reported with mPR-R. This trial was registered at www.clinicaltrials.gov as #NCT00602641.
Introduction
In prospective randomized trials, the combination of melphalan, prednisone, and thalidomide (MPT) significantly improves response rate and survival in elderly patients with multiple myeloma (MM) when compared with melphalan and prednisone (MP) alone.1 On this basis, MPT is considered a reference treatment of patients with newly diagnosed MM who are not candidates for high-dose melphalan-based therapies. Similarly, large phase 3 studies have demonstrated that the combination of melphalan, prednisone, and bortezomib (MPV) is also associated with improved survival vs MP alone.2 Nevertheless, the toxicities of thalidomide and bortezomib limit the potential success of either regimen. Lenalidomide is an active agent in MM with high response rates and a modest toxicity profile when used in combination with dexamethasone.3 We therefore wished to explore the use of lenalidomide in combination with MP in an attempt to further improve progression-free survival (PFS) and overall survival (OS) while minimizing toxicity in elderly MM patients.
When compared with thalidomide, lenalidomide is generally considered more potent and has a relative lack of major symptomatic toxicity (constipation, neuropathy, and fatigue). Conversely, myelosuppression is more common, a finding that has made the combination of MPR harder to tolerate without dose reductions of melphalan and thus potentially compromised efficacy.4 The largest collective experience with MPR in phase 2 studies at the time of study design was reported on 54 patients in a phase 1/2 trial.5 The maximum tolerated dose (MTD) was defined as 0.18 mg/kg melphalan per day for 4 consecutive days every month and 10 mg lenalidomide per day for 21 consecutive days every month. At the MTD, 85% of patients showed at least a partial response (PR), including 52% of patients who achieved at least a very good partial response (VGPR) and 23% who showed an immunofixation-negative complete response. PFS was 24 months in this phase 2 trial vs 20 months in a meta-analysis of larger MPT trials.1 Major grade 3 or 4 adverse events (AEs) of MPR predominantly consisted of hematologic toxicities (neutropenia, 66%; thrombocytopenia, 34%). A second phase 1 clinical trial using a more stringent definition of dose-limiting toxicity established a lower dose of 5 mg/m2 melphalan and 10 mg lenalidomide daily as the MTD,4 and this is the dosing that was chosen to move forward. Although this dose of melphalan is lower than that used in comparable trials, we believed that this would result in higher tolerability and the ability to stay on treatment longer.
Although it was anticipated that mPR might prove the superior regimen with improved PFS and lower toxicity, neither feature could be confidently predicted. A phase 3 trial was therefore required to evaluate and compare the efficacy as well as the toxicity and quality of life (QOL) between MPT and mPR. PFS was ultimately chosen to be the only practical end point. Statistical evaluation of OS was determined to require over 1000 patients and over 8 years of follow-up and was thus considered impractical in the current treatment environment of MM, with new drugs emerging at a rapid pace. We predicted superiority of the experimental arm, and we therefore chose a noninferiority design with a superiority alternative. Because emerging data supported improved PFS in a number of clinical trials using thalidomide6,7 or lenalidomide continuously,3,5,8,9 it was decided to incorporate ongoing maintenance therapy in both arms of the trial, producing the 2 arms of the trial, MPT-T and mPR-R.
Methods
Study population
Eligible patients required a confirmed diagnosis of MM as well as evidence of end-organ damage at the time of diagnosis. Patients were ≥65 years and had declined alternative treatment or were <65 years and were not candidates for autologous stem cell transplantation or had declined transplant. Eastern Cooperative Oncology Group (ECOG) performance status ≤2 was required. Eligibility laboratory values included hemoglobin >7 g/dL, platelet count >75 000 cells/mm3, absolute neutrophil count >1000 cells/mm3, creatinine <2.5 mg/dL, creatinine clearance ≥60 mL/min, total bilirubin ≤1.5 mg/dL, and aspartate aminotransferase and alanine aminotransferase ≤2.5 times the upper limit of normal. Patients must have been previously untreated for MM, although prior treatment with prednisone or dexamethasone for <4 weeks total dosing alone or in combination with thalidomide or lenalidomide for <2 weeks total dosing was allowed. Patients could be receiving bisphosphonates or growth factors (erythropoietin). Patients had to be willing and able to take antithrombotic prophylaxis.
This clinical trial was approved by the institutional review board of all participating institutions, in accordance with the Declaration of Helsinki.
Statistical considerations
Patients were randomized with equal allocation to MPT-T or mPR-R. Treatments were assigned using permuted blocks within strata with dynamic balancing within main institution and their affiliate networks.10 Patients were stratified by International Staging System stage (I-II vs III) and age (<65 years vs ≥65 years). The primary objective was to compare PFS between patients receiving MPT-T vs mPR-R. PFS was defined as the time from randomization to the earliest documentation of disease progression or death from any cause without regard for timing of disease evaluation. Patients who were alive without evidence of disease progression were censored at the date of last disease assessment. The analysis data set for the primary end point of PFS included all randomized patients according to assigned treatment (intention to treat [ITT]). The noninferiority margin for the primary analysis was a hazard ratio (HR) of 0.82 corresponding to a median PFS of 25 months for MPT-T and 20.5 months for mPR-R. This design incorporated 8 interim analyses and 1 final analysis. Repeated confidence interval (CI) methodology similar to that described by Jennison and Turnbull was used for these analyses.11 At each scheduled interim analysis, a 1-sided 95% repeated CI on the treatment PFS HR was computed, using the partial likelihood estimate and a critical value based on the Lan-DeMets error spending rate function corresponding to the truncated version of O’Brien-Fleming boundaries.12,13
When the lower confidence limit for the treatment PFS HR was >0.82, the inferiority of mPR-R would be rejected and the alternative that mPR-R was not inferior would be accepted. Next, a secondary superiority test of mPR-R would be performed based on the lower confidence limit of a 1-sided 95% CI being greater than 1. If noninferiority of mPR-R was not shown, a secondary inferiority test of mPR-R was instead performed. When the upper confidence limit of a 1-sided 95% CI for the HR was <1, the null hypothesis of no difference would be rejected and mPR-R would be considered inferior. The primary noninferiority test had 86% power at the 1-sided .05 significance level with the planned sample size of 304 patients and 221 PFS events, if the true HR was 1.2 or more. The secondary tests had 83% power under the assumption that the true HR was 1.44 or more (superiority test) or 0.70 or less (inferiority).
Additional analyses of OS and PFS during maintenance centered on 2 different methods: (1) evaluating OS and PFS from the start of maintenance treatment (including only patients who received maintenance) and (2) landmark analysis at 12 months excluding patients with an event before 12 months and estimating OS and PFS from the landmark time point. Time-to-event distributions were estimated using the Kaplan-Meier (KM) method and compared using the log-rank test.14,15 The Greenwood formula for standard error was used to obtain CIs around KM estimates.16 Cox proportional hazards regression was used to assess treatment HRs.17 Group differences in time to event distributions were also measured using restricted mean survival time representing the area under the survival curves when cutting follow-up at a certain time.18
Response evaluation was based on the International Myeloma Working Group response criteria.19 Per-protocol response rate was adjudicated centrally, and because of a high number of unevaluable cases using per-protocol criteria, a second adjudicated response by principal investigator and coordinating center was also evaluated using International Myeloma Working Group criteria. VGPR and PR rates counting unevaluable patients in the denominator were calculated and compared using Fisher’s exact test.
Toxicities were assessed using CTCAEv3 including only toxicities of treatment relation possible, probable, or definite. Global grade 3 or higher rates with and without hematologic toxicity were calculated and compared using Fisher’s exact test. Hematologic toxicity reporting was not mandated unless grade 4 or higher. Overall second primary malignancies (SPM) incidence rates per 100 person-years of follow-up were calculated counting only 1 event per case. QOL was assessed in the E1A06 trial to capture the main disease-specific and treatment-related effects that patient’s experience. The following instruments were used: FACT Physical (7 questions, score 0-28), FACT Functional (F 7 questions, score 0-28), FACT Neurotoxicity (FACT-Ntx) (11 questions, score 0-44), and FACT Multiple Myeloma (14 questions, score 0-56). For each instrument, a higher score means better QOL. The primary QOL end point was the mean change from registration (prior to randomization) to the cycle 12 visit following induction treatment using the FACT-Ntx Trial Outcome Index (Fact-Ntx TOI), which is the sum of the FACT-G Physical, FACT-G Functional, and FACT-Ntx instruments (25 questions, score 0-100). QOL assessments were first administered at registration prior to initiation of treatment and then at the end of cycles 6, 12, 18, 24, and 38 and at time of early discontinuation (+14 days).
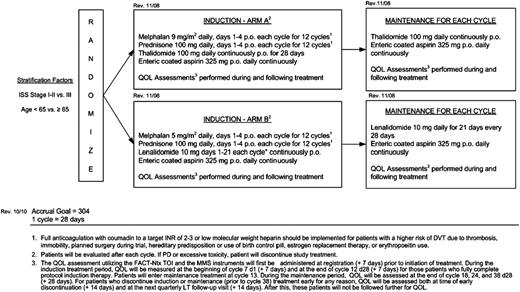
Treatment protocol
The study schema is shown in Figure 1. For induction, patients received either MPT (9 mg/m2 melphalan and 100 mg prednisone by mouth (po) on days 1 to 4 with 100 mg thalidomide daily) or mPR (5 mg/m2 melphalan and 100 mg prednisone po on days 1 to 4 with 10 mg lenalidomide po on days 1-21). Dose-reduction schedules were prespecified (see supplemental Data, available on the Blood Web site).
MPT or mPR therapy was continued for 12 28-day cycles followed by 100 mg thalidomide or 10 mg lenalidomide daily until progression or unacceptable toxicity. Maintenance was not given in patients discontinuing therapy during induction. Aspirin prophylaxis was required. Full anticoagulation was implemented for patients at higher risk for deep vein thrombosis. Dose reductions for melphalan, prednisone, thalidomide, and lenalidomide were detailed in the protocol. Bisphosphonate therapy was recommended for all patients with active bone disease with 90 mg pamidronate IV once monthly.
Results
Recruitment and baseline characteristics
The study was activated on February 29, 2008. The study was closed to accrual on November 30, 2011, with final accrual of 306 patients (154 on arm A [MPT-T], 152 on arm B [mPR-R]). Seven cooperative groups contributed, with 66% of patients coming from 33 participating ECOG centers.
Accrual averaged 7 patients per month. The median follow-up among survivors was 40.7 months. As of the date of this analysis, 222 PFS events have been observed. Treatment arms were balanced for age, International Staging System stage, and other major prognostic factors (Table 1). Median age was 75.7 years. A consort diagram is provided in supplemental Figure 1 and summarizes record status for all 306 patients enrolled.
Baseline characteristics
| . | MPT-T (n = 154) . | mPR-R (n = 152) . |
|---|---|---|
| Gender, male | 86 (55.8) | 81 (53.3) |
| Age (y), median (range) | 75.8 (54.3-91.9) | 76.6 (62.7-91.6) |
| <65 y | 9 (5.8) | 6 (4.0) |
| <75 y | 61 (39.6) | 63 (41. 5) |
| Race | ||
| White | 131 (85.6) | 132 (87.4) |
| Unknown/missing | 1 | 1 |
| International Staging System | ||
| Stage I | 45 (29.6) | 36 (23.7) |
| Stage II | 58 (38.2) | 70 (46.0) |
| Stage III | 49 (32.2) | 46 (30.3) |
| Unknown/Missing | 2 | 0 |
| ECOG performance status | ||
| 0 | 51 (33.1) | 49 (32.2) |
| 1 | 74 (48.1) | 74 (48.7) |
| 2 | 29 (18.8) | 29 (19.1) |
| Hemoglobin ≤11 g/dL | 92 (59.7) | 84 (55.3) |
| Serum creatinine >1.5 mg/dL | 16 (10.4) | 16 (10.5) |
| β-2 microglobulin ≥3.5 mg/L | 95 (62.5) | 99 (65.1) |
| Serum M-protein (g/dL) | 7.9 (4.7-13.4) | 8.3 (4.4-14.4) |
| Serum M, present | 145 (95.4) | 141 (94.0) |
| Heavy chain | ||
| IgG | 92 (71.3) | 90 (72.6) |
| IgA | 32 (24.8) | 32 (25.8) |
| IgM/IgD/biclonal | 5 (3.9) | 2 (1.6) |
| Unknown/missing | 16 | 17 |
| Light chain | ||
| κ | 96 (66.2) | 88 (63.3) |
| Λ | 49 (33.8) | 51 (36.7) |
| Unknown/missing | 0 | 2 |
| . | MPT-T (n = 154) . | mPR-R (n = 152) . |
|---|---|---|
| Gender, male | 86 (55.8) | 81 (53.3) |
| Age (y), median (range) | 75.8 (54.3-91.9) | 76.6 (62.7-91.6) |
| <65 y | 9 (5.8) | 6 (4.0) |
| <75 y | 61 (39.6) | 63 (41. 5) |
| Race | ||
| White | 131 (85.6) | 132 (87.4) |
| Unknown/missing | 1 | 1 |
| International Staging System | ||
| Stage I | 45 (29.6) | 36 (23.7) |
| Stage II | 58 (38.2) | 70 (46.0) |
| Stage III | 49 (32.2) | 46 (30.3) |
| Unknown/Missing | 2 | 0 |
| ECOG performance status | ||
| 0 | 51 (33.1) | 49 (32.2) |
| 1 | 74 (48.1) | 74 (48.7) |
| 2 | 29 (18.8) | 29 (19.1) |
| Hemoglobin ≤11 g/dL | 92 (59.7) | 84 (55.3) |
| Serum creatinine >1.5 mg/dL | 16 (10.4) | 16 (10.5) |
| β-2 microglobulin ≥3.5 mg/L | 95 (62.5) | 99 (65.1) |
| Serum M-protein (g/dL) | 7.9 (4.7-13.4) | 8.3 (4.4-14.4) |
| Serum M, present | 145 (95.4) | 141 (94.0) |
| Heavy chain | ||
| IgG | 92 (71.3) | 90 (72.6) |
| IgA | 32 (24.8) | 32 (25.8) |
| IgM/IgD/biclonal | 5 (3.9) | 2 (1.6) |
| Unknown/missing | 16 | 17 |
| Light chain | ||
| κ | 96 (66.2) | 88 (63.3) |
| Λ | 49 (33.8) | 51 (36.7) |
| Unknown/missing | 0 | 2 |
Data are presented as n (%) unless otherwise specified.
IgA, immunoglobulin A; IgD, immunoglobulin D; IgG, immunoglobulin G.
Treatment received
Two hundred seventy-five patients were off treatment as of the analysis date. Mean duration of overall treatment (induction and maintenance) was 15.6 months on MPT-T and 14.9 months on mPR-R for the entire study cohort. After 6, 9, and 12 cycles 31%, 45% and 56% of MPT-T patients had stopped treatment and 41%, 53%, and 60% of mPR-R patients were off treatment at those time points, respectively. Maintenance was not given if patients came off study due to toxicity or disease progression. A total of 139 treated patients (46.6%) went on to maintenance, with similar proportions between arms. Maintenance patients received on average 13.5 months of thalidomide maintenance and 13.3 months of lenalidomide maintenance. For the MPT-T arm, mean percent full protocol dose during induction of thalidomide and melphalan was 81.8% and 77.9%, respectively. For mPR-R, mean percent full protocol dose of lenalidomide and melphalan was 81.6% and 79.8%, respectively. Over the first 2 years of maintenance (cycles 12-36), mean percent full protocol dose was 67.1% for thalidomide and 74.0% for lenalidomide. There was no significant difference in dose intensity for any drug by age except in maintenance, where, surprisingly, both drugs were maintained at intended doses in patients ≥75 years more frequently. This was most notable for lenalidomide dose intensity, with 78% intended dose vs 70.9% for thalidomide in these elderly patients. For patients <75 years of age, percent intended dose during maintenance was 64.4% for thalidomide and 67% for lenalidomide. The primary off-treatment reasons were AEs (41.8%), which were slightly higher on the MPT-T arm, and disease progression (33.8%), which was higher in the mPR-R arm. AEs in study patients who discontinued therapy are shown in supplemental Table 1.
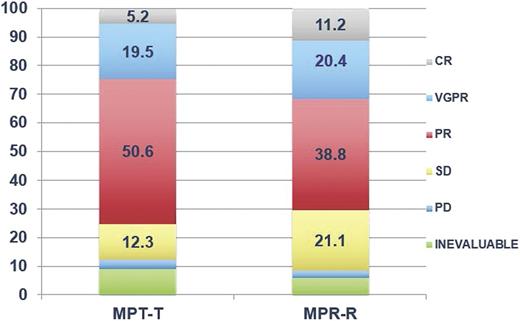
Response rates
Per-protocol PR rate was 63.6% (95% CI, 56.0%-71.2%) on MPT-T compared with 59.9% (95% CI, 52.1%-67.7%) on mPR-R (P = .557). The VGPR rate was 18.8% (95% CI, 12.7%- 25.0%) on MPT-T and 23.0% (95% CI, 16.3%-29.7%) on mPR-R (P = .401). However, 42 patients were unevaluable due primarily to protocol deviations in baseline or follow-up laboratory test results. Because this strict protocol response criteria often involved a single data point (eg, commonly a missing 24-hour urine test result), a second centrally adjudicated response rate was calculated, which resulted in higher PR rates that were considered more accurate for actual response and thus also reported (MPT-T 75.3% and mPR-R 70.4%) as well as VGPR rates (MPT-T 24.7% and mPR-R 31.6%), while trends in the difference between arms in VGPR and PR rates were maintained (Figure 2).
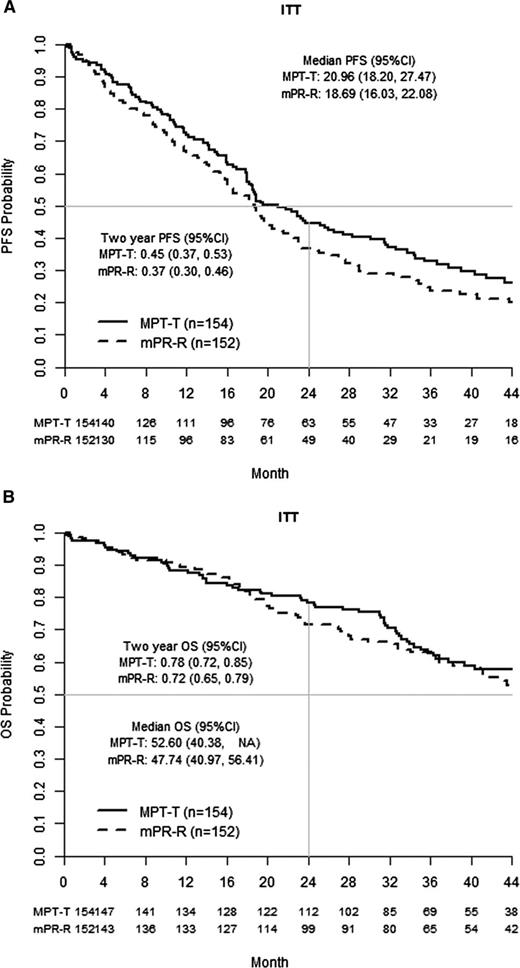
PFS and OS
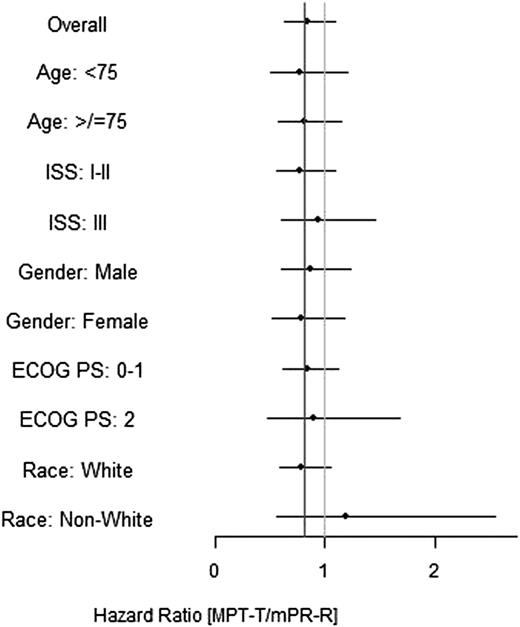
As of this analysis, 222 PFS events have been observed, exceeding full information by 1 event. For the primary ITT analysis, the median PFS observed was 21.0 months on MPT-T and 18.7 months on mPR-R (Figure 3A). Using stratified Cox regression, the treatment HR estimate was 0.84 (95% CI, 0.64-1.09; P = .186). Given the lower confidence limit was <0.82, the null hypothesis that mPR-R is inferior was not rejected and the alternative that mPR-R is noninferior was not accepted. Before the test of inferiority of mPR-R, because the upper limit of the CI was >1.0, the null hypothesis of no treatment difference was not rejected. A forest plot of the treatment effect within subgroups along with KM plots is shown in Figure 4. A total of 135 patients have died (MPT-T, 40.9% [63/154]; mPR-R, 47.4% [72/152]). Ten patients refused follow-up, and 4 were officially lost to follow-up. For the ITT analysis, the median OS observed was 52.6 months on MPT-T and 47.7 months on mPR-R (Figure 3B). Using stratified Cox regression, the treatment HR estimate was 0.88 (95% CI, 0.63-1.24; P = .476). Two-year OS probability was 0.78 (95% CI, 0.72-0.85) on MPT-T and 0.72 (95% CI, 0.65-0.79) on mPR-R.
Forest plot. The prespecified subgroup analyses showed no significant differences. ISS, International Staging System; PS, performance status.
Forest plot. The prespecified subgroup analyses showed no significant differences. ISS, International Staging System; PS, performance status.
We also calculated the effect of age (supplemental Figure 2). PFS was 25.6 months (MPT-T) vs 21.6 months (mPR-R) for those <75 years and 18.9 months (MPT-T) vs 16.6 months (mPR-R) for those ≥75 years. OS for patients <75 years was not reached for MPT-T and was 49.4 months for mPR-R, whereas OS for those ≥75 years was 52.6 vs 46.7 months trending in favor of MPT-T (but not statistically significant).
Toxicity
Reported overall grade ≥3 toxicity was 73.0% (MPT-T) vs 58.0% (mPR-R) (P = .007), and 41.8% of patients stopped therapy due to an AE or side effect (44.3% for MPT-T vs 39.3% for mPR-R). Note that reported overall global toxicity rate is likely to be underestimated, because grade <4 myelosuppression events were considered expected and not required to be reported. Grade 3 or higher nonhematologic toxicity was significantly higher in the MPT-T arm (59.5% vs 40.0%; P = .001) (Table 2). There was also a notable age effect in the MPT-T arm, with 47.2% of those >75 years experiencing a grade ≥3 AE vs 35.6% of patients <75 years (Table 2). This difference in tolerability by age was not significant in mPR-R patients. Frequent grade ≥3 events in >5% of patients (Table 3) included anemia, leukopenia, lymphopenia, neutropenia, fatigue, platelets, constipation, and dyspnea (MPT-T arm only). Deep vein thrombosis or pulmonary embolism was observed in 8.8% and 6.7% of patients on MPT-T and mPR-R, respectively.
Global treatment-related toxicity rates
| . | Nonhematologic . | Hematologic and nonhematologic . | ||||
|---|---|---|---|---|---|---|
| Worst grade by patient . | No. of patients . | Grade 3-5 . | Rate . | No. of patients . | Grade 4-5 . | Rate . |
| Overall | ||||||
| MPT-T | 148 | 88 | 59.5% | 148 | 61 | 41.2% |
| mPR-R | 150 | 60 | 40.0% | 150 | 49 | 32.7% |
| Difference | — | — | 19.5% | — | — | 8.5% |
| P value | — | — | .001 | — | — | .150 |
| During induction | ||||||
| MPT | 148 | 75 | 50.7% | 148 | 54 | 36.5% |
| mPR-R | 150 | 54 | 36.0% | 150 | 45 | 30.0% |
| Difference | — | — | 14.7% | — | — | 6.5% |
| P value | — | — | .014 | — | — | .269 |
| During maintenance | ||||||
| MPT-T | 70 | 19 | 27.1% | 70 | 6 | 8.6% |
| mPR-R | 69 | 11 | 15.9% | 69 | 6 | 8.7% |
| Difference | — | — | 11.2% | — | — | −0.1% |
| P value | — | — | .149 | — | — | 1.000 |
| Age ≥75 y | ||||||
| MPT-T | 89 | 51 | 57.3% | 89 | 39 | 43.8% |
| mPR-R | 88 | 37 | 42.0% | 88 | 31 | 35.2% |
| Difference | — | — | 15.3% | — | — | 8.6% |
| P value | — | — | .051 | — | — | .283 |
| Age <75 y | ||||||
| MPT-T | 59 | 37 | 62.7% | 59 | 22 | 37.3% |
| mPR-R | 62 | 23 | 37.1% | 62 | 18 | 29.0% |
| Total | 121 | 60 | 49.6% | 121 | 40 | 33.1% |
| Difference | — | — | 25.6% | — | — | 0.4% |
| P value | — | — | .006 | — | — | .440 |
| . | Nonhematologic . | Hematologic and nonhematologic . | ||||
|---|---|---|---|---|---|---|
| Worst grade by patient . | No. of patients . | Grade 3-5 . | Rate . | No. of patients . | Grade 4-5 . | Rate . |
| Overall | ||||||
| MPT-T | 148 | 88 | 59.5% | 148 | 61 | 41.2% |
| mPR-R | 150 | 60 | 40.0% | 150 | 49 | 32.7% |
| Difference | — | — | 19.5% | — | — | 8.5% |
| P value | — | — | .001 | — | — | .150 |
| During induction | ||||||
| MPT | 148 | 75 | 50.7% | 148 | 54 | 36.5% |
| mPR-R | 150 | 54 | 36.0% | 150 | 45 | 30.0% |
| Difference | — | — | 14.7% | — | — | 6.5% |
| P value | — | — | .014 | — | — | .269 |
| During maintenance | ||||||
| MPT-T | 70 | 19 | 27.1% | 70 | 6 | 8.6% |
| mPR-R | 69 | 11 | 15.9% | 69 | 6 | 8.7% |
| Difference | — | — | 11.2% | — | — | −0.1% |
| P value | — | — | .149 | — | — | 1.000 |
| Age ≥75 y | ||||||
| MPT-T | 89 | 51 | 57.3% | 89 | 39 | 43.8% |
| mPR-R | 88 | 37 | 42.0% | 88 | 31 | 35.2% |
| Difference | — | — | 15.3% | — | — | 8.6% |
| P value | — | — | .051 | — | — | .283 |
| Age <75 y | ||||||
| MPT-T | 59 | 37 | 62.7% | 59 | 22 | 37.3% |
| mPR-R | 62 | 23 | 37.1% | 62 | 18 | 29.0% |
| Total | 121 | 60 | 49.6% | 121 | 40 | 33.1% |
| Difference | — | — | 25.6% | — | — | 0.4% |
| P value | — | — | .006 | — | — | .440 |
Grade 3 or higher treatment-related toxicities occurring in 5% or more of patients
| Toxicity type . | Treatment arm . | |||
|---|---|---|---|---|
| MPT-T (n = 148) . | mPR-R (n = 150) . | |||
| Grade 3 . | Grade 4 . | Grade 3 . | Grade 4 . | |
| Hemoglobin | 11 | 5 | 8 | 3 |
| Leukocytes | 10 | 19 | 11 | 6 |
| Lymphopenia | 8 | 13 | 8 | 2 |
| Neutrophils | 8 | 33 | 7 | 36 |
| Platelets | 1 | 17 | 6 | 7 |
| Fatigue | 16 | — | 11 | 3 |
| Constipation | 8 | — | — | — |
| Dyspnea | 12 | — | 6 | — |
| Thrombosis/thrombus/embolism | 12 | 1 | 6 | 3 |
| Toxicity type . | Treatment arm . | |||
|---|---|---|---|---|
| MPT-T (n = 148) . | mPR-R (n = 150) . | |||
| Grade 3 . | Grade 4 . | Grade 3 . | Grade 4 . | |
| Hemoglobin | 11 | 5 | 8 | 3 |
| Leukocytes | 10 | 19 | 11 | 6 |
| Lymphopenia | 8 | 13 | 8 | 2 |
| Neutrophils | 8 | 33 | 7 | 36 |
| Platelets | 1 | 17 | 6 | 7 |
| Fatigue | 16 | — | 11 | 3 |
| Constipation | 8 | — | — | — |
| Dyspnea | 12 | — | 6 | — |
| Thrombosis/thrombus/embolism | 12 | 1 | 6 | 3 |
Data are presented as number of patients.
SPMs
Substantial attention has recently been focused on the possible development of SPMs in patients receiving prolonged lenalidomide therapy. SPMs were observed in 18 MPT-T patients vs 14 mPR-R patients. Excluding nonmelanoma skin cancers, the incidence rates were 3.47 and 2.01 (cases/100 person-years). Notably, there were 10 (6 myelodysplasia and 4 leukemias) hematologic malignancies in the MPT-T arm vs 4 (3 lymphoma and 1 leukemia) in the mPR-R arm, likely reflecting the higher melphalan dose employed (Table 4).
SPMs
| . | MPT-T . | mPR-R . | Total . |
|---|---|---|---|
| Treated patients | 148 | 150 | 298 |
| SPM events | 18 | 14 | 32 |
| IR/100 PY | 4.56 | 3.56 | 4.06 |
| Total | 12.2% | 9.3% | 10.7% |
| SPM excluding nonmelanoma skin and basal cell carcinoma | 14 | 8 | 22 |
| IR/100 PY | 3.47 | 2.01 | 2.74 |
| Total | 9.5% | 5.3% | 7.4% |
| . | MPT-T . | mPR-R . | Total . |
|---|---|---|---|
| Treated patients | 148 | 150 | 298 |
| SPM events | 18 | 14 | 32 |
| IR/100 PY | 4.56 | 3.56 | 4.06 |
| Total | 12.2% | 9.3% | 10.7% |
| SPM excluding nonmelanoma skin and basal cell carcinoma | 14 | 8 | 22 |
| IR/100 PY | 3.47 | 2.01 | 2.74 |
| Total | 9.5% | 5.3% | 7.4% |
IR, incidence rate; PY, person-years.
QOL
A statistically superior QOL was reported in favor of mPR-R, with mean change in FACT-Ntx TOI score from registration to the end of induction of −2.8 for MPT-T vs 3.3 for mPR-R (P = .007). The mean change in the FACT-MM TOI score was 2.3 for MPT-T vs 7.4 for mPR-R (P = .09). The FACT-Ntx scale showed statistical improvement for the mPR-R arm at cycles 12 and 18 and at end of treatment, whereas the FACT Physical and Functional scales showed no significant differences by arm. Details are shown in supplemental Table 2.
Discussion
For decades, MP was the standard therapy for newly diagnosed MM.20 After stem cell collection was observed to be compromised by prior melphalan, this MP treatment regimen was applied mostly to patients considered ineligible for high-dose melphalan and autologous stem cell collection.21 Subsequently, with the adoption of novel therapeutic agents, thalidomide22,23 and then bortezomib2,24 were shown to improve OS when added to the MP regimen. The MPR regimen was then tested, and although it appeared to offer higher response rates, an increase in myelosuppression required dose reduction of both melphalan and lenalidomide, thus potentially compromising efficacy.4,25 Randomized trials were then required to explore this triplet combination therapy with other established regimens. In one such trial (MM-015), a fixed-duration MPR regimen was equivalent to MP in terms of PFS and OS,9 a disappointing result attributed to myelotoxicity of the MPR regimen. However, use of continuous lenalidomide maintenance following MPR produced significant improvement in PFS.
We set out to compare MPT-T with MPR but use the designation mPR-R to delineate the lower doses of melphalan that can be coadministered as well as continuous use of lenalidomide, with a hypothesis that mPR-R would be noninferior and possible superior in terms of toxicity and survival outcomes. We hoped that the lower dose of melphalan employed would produce a more tolerable regimen with less myelosuppression and improved results. However, our trial was conducted in a very elderly population with fewer than 10% of patients <65 years and a mean age of 76 compared with 73 years in the recent Dutch-Belgium Hemato-Oncology Cooperative Group (HOVON) trial26 report and 71 years in the MM-015 study. The older age in our study likely reflects that in the United States, transplant eligibility is generally 70 years or older; newer, less toxic drugs are more readily available; and during the course of this study, melphalan fell out of fashion, except in the very elderly. Interestingly, however, our data are very similar to those of the HOVON study but inferior to the MM-015 study with lenalidomide continuous therapy. The reasons for this are not clear, although age may contribute. In our study, PFS was 5 months shorter among older patients (>75 years) in the mPR-R arm, although of interest, tolerability of drugs was somewhat independent of age (≤75 years vs >75 years) in this arm of the trial.
There were no statistically significant response or survival differences between arms, although toxicity profiles favored lenalidomide. Response rates were 82% and 83% on the HOVON study vs 75.3 and 70% for this E1a06 study, whereas VGPR rates were clearly higher in the HOVON study. We believe (but can only hypothesize based on available data) that this reflects the lower doses of melphalan in the mPR arm of E1a06 and the lower thalidomide dose in the MPT arm as well as the higher age of patients in E1a06. Surprisingly, deeper responses in the HOVON trial did not translate into better PFS, as the PFS was essentially identical between the 2 phase 3 trials.
The major discrepancies result from the MM-015 study, which showed superiority for the MPR-R regimen. This seemed most obvious in younger patients who could tolerate the higher melphalan dose employed and thus the myelosuppression. We assume this explains the wide difference in the MM-015 and E1a06 and suggests that a dose-intense approach in younger patients receiving MPR-R is advisable. We could not, however, determine such an age effect, but only 5.6% of patients in our study were <65 years; furthermore, it would not really explain the differences between the HOVON and the MM-015 trial.
Both regimens proved toxic. At least 58% of mPR-R patients and 73% of MPT-T patients experienced grade 3 toxicity, and half the patients discontinued treatment before finishing 12 months of planned induction therapy, with toxicity being the primary reason (42%) for stopping treatment. Compared with other induction MM regimens such as Rd,26 VMP,2 VTD,27 VRD,28 CyborD,28 and KRd,29 the 70% to 75% response rates of MPT and mPR were lower and the toxicity higher.
Interestingly, hematologic malignancy was higher with MPT, likely reflecting the higher melphalan dose employed. However, it is important to note that only grade ≥4 hematologic toxicity was recorded, and estimates of overall hematologic toxicity are thus incomplete for both arms. Consequently, although there was less nonhematologic toxicity with the mPR-R regimen, it seems that neither regimen is particularly well tolerated. In our study, QOL was measured, and use of lenalidomide was associated with a better patient-reported QOL. Much of this difference appears attributable to lower neuropathy rates with lenalidomide than with thalidomide.
A perusal of other phase 3 trials using melphalan as a backbone (Table 5) suggests that (1) The use of continuous lenalidomide seems to improve PFS, (2) contemporaneous salvage therapies result in outcomes following MPT-T superior to those seen in historical controls and, finally, (3) OS rates are seemingly equivalent no matter what partner drug is added to MP.
A comparison of randomized phase 3 trials using a melphalan and prednisone backbone
| . | Median PFS (mo) . | Median OS (mo) . |
|---|---|---|
| MPT10 (meta-analysis) | 21 | 39 |
| MPT-T (E1A06) | 21 | 53 |
| MPT-T (HOVON)26 | 20 | 49 |
| MPR (MM-015)9 | 14 | 52 |
| MPR-R (E1A06) | 19 | 48 |
| MPR-R (HOVON) | 22 | 50 |
| MPR-R (MM-015)9 | 31 | 56 |
| MPV (Vista)2 | 24 | 56 |
In summary, this phase 3 trial demonstrates comparable efficacy of MPT-T and mPR-R in elderly patients with newly diagnosed MM. Response rates, PFS, and OS were not statistically different between arms; however, there was significantly better patient-reported QOL at 12 months (mainly due to better neurotoxicity scores) and lower overall nonhematologic and grade 4 or higher hematologic toxicity with mPR-R.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study was coordinated by the ECOG-ACRIN Cancer Research Group (Robert L. Comis and Mitchell D. Schnall, group co-chairs).
This study was supported in part by Public Health Service Grants CA180820, CA180794, CA180790, CA189956, CA180799, and CA31946 and by the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services. Its content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute.
Authorship
Contribution: A.K.S., S.V.R., N.S.C., and S.J. designed the trial, conducted trial analysis, and wrote the first draft of the manuscript, which was subsequently reviewed, edited, and approved by all authors; R.F. was responsible for ancillary laboratory studies and patient accrual; M.W. conducted QOL studies; and A.A.K.-C. was principal investigator for CALGB and contributed to writing the manuscript.
Conflict-of-interest disclosure: A.K.S. has received consulting and advisory board fees from Celgene, Novartis, Bristol Meyers Squib, Sanofi Aventis, and Janssen. R.F. has received consulting fees from Celgene, BMS, Lilly, Onyx, Binding Site, Millennium, Bayer, Novartis, Applied Biosciences, and AMGEN and has conducted research sponsored by Onyx Pharmaceuticals. The remaining authors declare no competing financial interests.
Correspondence: A. Keith Stewart, Division of Hematology/Oncology, Room 1-006, Collaborative Research Building, Mayo Clinic in Arizona, 13400 E Shea Blvd, Scottsdale, AZ 85259; e-mail: stewart.keith@mayo.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal