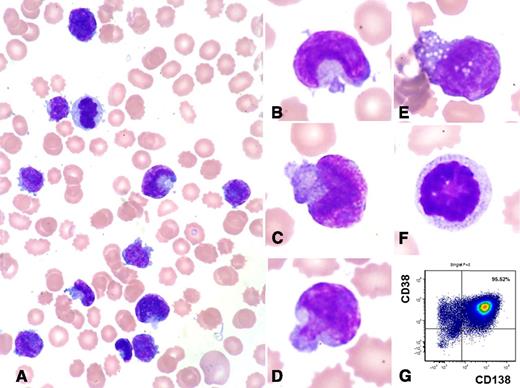
This peripheral blood smear is from a 72-year-old woman, taken several hours before she died of recurrent plasma cell myeloma and newly developed secondary plasma cell leukemia. Her white blood cell count increased from 39.5 × 103/μL to 233.2 × 103/μL in 28 hours. The peripheral blood smear shows marked leukocytosis with numerous small- to medium-sized bizarre-looking cells (95% of white blood cells) (panels A-E), which were not seen in her initial bone marrow aspirate. These cells have pleomorphic nuclear shapes such as a fish mouth, a mushroom, or a moon. All cells have scant pale cytoplasm, and some have cytoplasmic vacuoles. Mitotic figures are identified (panels A and F).
Despite the unusual cellular morphology, flow cytometric analysis confirmed these cells to be aberrant plasma cells (positive for CD38, CD138, partial CD56, and κ light chain, and negative for CD45, CD19, CD20, CD28, CD117, and λ light chain) (panel G). Her initial cytogenetics study showed a complex karyotype: 45∼46,XX,+1,add(1)(p13),der(3)t(3;11)(q29;q13),t(11;14)(q13;q32),+14, del(14)(q24). Fluorescence in situ hybridization reported monosomy 13, t(11;14) IgH/cyclinD1 translocation, CSK1B gene amplification, and TP53 gene deletion. Cytogenetics was not performed during her last admission. Her initial serum lactate dehydrogenase level was normal, but her last serum lactate dehydrogenase level was 30 489 IU/L (normal, 313-618 IU/L). Her initial and last serum β2-microglobulin levels were 9.5 and 7.4 mg/L (normal, 0.8-2.3), respectively. This case highlights the broad morphologic spectrum of plasma cell myeloma/leukemia.
This peripheral blood smear is from a 72-year-old woman, taken several hours before she died of recurrent plasma cell myeloma and newly developed secondary plasma cell leukemia. Her white blood cell count increased from 39.5 × 103/μL to 233.2 × 103/μL in 28 hours. The peripheral blood smear shows marked leukocytosis with numerous small- to medium-sized bizarre-looking cells (95% of white blood cells) (panels A-E), which were not seen in her initial bone marrow aspirate. These cells have pleomorphic nuclear shapes such as a fish mouth, a mushroom, or a moon. All cells have scant pale cytoplasm, and some have cytoplasmic vacuoles. Mitotic figures are identified (panels A and F).
Despite the unusual cellular morphology, flow cytometric analysis confirmed these cells to be aberrant plasma cells (positive for CD38, CD138, partial CD56, and κ light chain, and negative for CD45, CD19, CD20, CD28, CD117, and λ light chain) (panel G). Her initial cytogenetics study showed a complex karyotype: 45∼46,XX,+1,add(1)(p13),der(3)t(3;11)(q29;q13),t(11;14)(q13;q32),+14, del(14)(q24). Fluorescence in situ hybridization reported monosomy 13, t(11;14) IgH/cyclinD1 translocation, CSK1B gene amplification, and TP53 gene deletion. Cytogenetics was not performed during her last admission. Her initial serum lactate dehydrogenase level was normal, but her last serum lactate dehydrogenase level was 30 489 IU/L (normal, 313-618 IU/L). Her initial and last serum β2-microglobulin levels were 9.5 and 7.4 mg/L (normal, 0.8-2.3), respectively. This case highlights the broad morphologic spectrum of plasma cell myeloma/leukemia.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal